
- •Preface to the 3rd edition
- •General Pharmacology
- •Systems Pharmacology
- •Therapy of Selected Diseases
- •Subject Index
- •Abbreviations
- •General Pharmacology
- •History of Pharmacology
- •Drug and Active Principle
- •The Aims of Isolating Active Principles
- •European Plants as Sources of Effective Medicines
- •Drug Development
- •Congeneric Drugs and Name Diversity
- •Oral Dosage Forms
- •Drug Administration by Inhalation
- •Dermatological Agents
- •From Application to Distribution in the Body
- •Potential Targets of Drug Action
- •External Barriers of the Body
- •Blood–Tissue Barriers
- •Membrane Permeation
- •Binding to Plasma Proteins
- •The Liver as an Excretory Organ
- •Biotransformation of Drugs
- •Drug Metabolism by Cytochrome P450
- •The Kidney as an Excretory Organ
- •Presystemic Elimination
- •Drug Concentration in the Body as a Function of Time—First Order (Exponential) Rate Processes
- •Time Course of Drug Concentration in Plasma
- •Time Course of Drug Plasma Levels during Repeated Dosing (A)
- •Time Course of Drug Plasma Levels during Irregular Intake (B)
- •Accumulation: Dose, Dose Interval, and Plasma Level Fluctuation (A)
- •Dose–Response Relationship
- •Concentration–Effect Curves (B)
- •Concentration–Binding Curves
- •Types of Binding Forces
- •Agonists—Antagonists
- •Other Forms of Antagonism
- •Enantioselectivity of Drug Action
- •Receptor Types
- •Undesirable Drug Effects, Side Effects
- •Drug Allergy
- •Cutaneous Reactions
- •Drug Toxicity in Pregnancy and Lactation
- •Pharmacogenetics
- •Placebo (A)
- •Systems Pharmacology
- •Sympathetic Nervous System
- •Structure of the Sympathetic Nervous System
- •Adrenergic Synapse
- •Adrenoceptor Subtypes and Catecholamine Actions
- •Smooth Muscle Effects
- •Cardiostimulation
- •Metabolic Effects
- •Structure–Activity Relationships of Sympathomimetics
- •Indirect Sympathomimetics
- •Types of
- •Antiadrenergics
- •Parasympathetic Nervous System
- •Cholinergic Synapse
- •Parasympathomimetics
- •Parasympatholytics
- •Actions of Nicotine
- •Localization of Nicotinic ACh Receptors
- •Effects of Nicotine on Body Function
- •Aids for Smoking Cessation
- •Consequences of Tobacco Smoking
- •Dopamine
- •Histamine Effects and Their Pharmacological Properties
- •Serotonin
- •Vasodilators—Overview
- •Organic Nitrates
- •Calcium Antagonists
- •ACE Inhibitors
- •Drugs Used to Influence Smooth Muscle Organs
- •Cardiac Drugs
- •Cardiac Glycosides
- •Antiarrhythmic Drugs
- •Iron Compounds
- •Prophylaxis and Therapy of Thromboses
- •Possibilities for Interference (B)
- •Heparin (A)
- •Hirudin and Derivatives (B)
- •Fibrinolytics
- •Intra-arterial Thrombus Formation (A)
- •Formation, Activation, and Aggregation of Platelets (B)
- •Inhibitors of Platelet Aggregation (A)
- •Presystemic Effect of ASA
- •Plasma Volume Expanders
- •Lipid-lowering Agents
- •Diuretics—An Overview
- •NaCl Reabsorption in the Kidney (A)
- •Aquaporins (AQP)
- •Osmotic Diuretics (B)
- •Diuretics of the Sulfonamide Type
- •Potassium-sparing Diuretics (A)
- •Vasopressin and Derivatives (B)
- •Drugs for Gastric and Duodenal Ulcers
- •Laxatives
- •Antidiarrheal Agents
- •Drugs Affecting Motor Function
- •Muscle Relaxants
- •Nondepolarizing Muscle Relaxants
- •Depolarizing Muscle Relaxants
- •Antiparkinsonian Drugs
- •Antiepileptics
- •Pain Mechanisms and Pathways
- •Eicosanoids
- •Antipyretic Analgesics
- •Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- •Cyclooxygenase (COX) Inhibitors
- •Local Anesthetics
- •Opioid Analgesics—Morphine Type
- •General Anesthesia and General Anesthetic Drugs
- •Inhalational Anesthetics
- •Injectable Anesthetics
- •Sedatives, Hypnotics
- •Benzodiazepines
- •Pharmacokinetics of Benzodiazepines
- •Therapy of Depressive Illness
- •Mania
- •Therapy of Schizophrenia
- •Psychotomimetics (Psychedelics, Hallucinogens)
- •Hypothalamic and Hypophyseal Hormones
- •Thyroid Hormone Therapy
- •Glucocorticoid Therapy
- •Follicular Growth and Ovulation, Estrogen and Progestin Production
- •Oral Contraceptives
- •Antiestrogen and Antiprogestin Active Principles
- •Aromatase Inhibitors
- •Insulin Formulations
- •Treatment of Insulin-dependent Diabetes Mellitus
- •Treatment of Maturity-Onset (Type II) Diabetes Mellitus
- •Oral Antidiabetics
- •Drugs for Maintaining Calcium Homeostasis
- •Drugs for Treating Bacterial Infections
- •Inhibitors of Cell Wall Synthesis
- •Inhibitors of Tetrahydrofolate Synthesis
- •Inhibitors of DNA Function
- •Inhibitors of Protein Synthesis
- •Drugs for Treating Mycobacterial Infections
- •Drugs Used in the Treatment of Fungal Infections
- •Chemotherapy of Viral Infections
- •Drugs for the Treatment of AIDS
- •Drugs for Treating Endoparasitic and Ectoparasitic Infestations
- •Antimalarials
- •Other Tropical Diseases
- •Chemotherapy of Malignant Tumors
- •Targeting of Antineoplastic Drug Action (A)
- •Mechanisms of Resistance to Cytostatics (B)
- •Inhibition of Immune Responses
- •Antidotes and Treatment of Poisonings
- •Therapy of Selected Diseases
- •Hypertension
- •Angina Pectoris
- •Antianginal Drugs
- •Acute Coronary Syndrome— Myocardial Infarction
- •Congestive Heart Failure
- •Hypotension
- •Gout
- •Obesity—Sequelae and Therapeutic Approaches
- •Osteoporosis
- •Rheumatoid Arthritis
- •Migraine
- •Common Cold
- •Bronchial Asthma
- •Emesis
- •Alcohol Abuse
- •Local Treatment of Glaucoma
- •Further Reading
- •Further Reading
- •Picture Credits
- •Drug Indexes

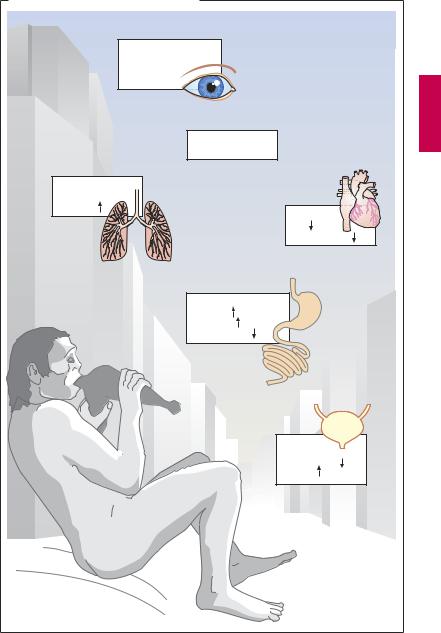
102 Drugs Acting on the Parasympathetic Nervous System
Parasympathetic Nervous System
Responses to activation of the parasympathetic system. Parasympathetic nerves regulate processes connected with energy assimilation (food intake, digestion, absorption) and storage. These processes operate when the body is at rest, allowing a decreased tidal volume (increased bronchomotor tone) and decreased cardiac activity. Secretion of saliva and intestinal fluids promotes the digestion of food stuffs; transport of intestinal contents is speeded up because of enhanced peristaltic activity and lowered tone of sphincteric muscles. To empty the urinary bladder (micturition), wall tension is increased by detrusor activation with a concurrent relaxation of sphincter tonus.
Activation of ocular parasympathetic fibers (see below) results in narrowing of the pupil and increased curvature of the lens, enabling near objects to be brought into focus (accommodation).
Anatomy of the parasympathetic system.
The cell bodies of parasympathetic preganglionic neurons are located in the brainstem and the sacral spinal cord. Parasympathetic outflow is channeled from the brainstem (1) through the third cranial nerve (oculomotor n.) via the ciliary ganglion to the eye; (2) through the seventh cranial nerve (facial n.) via the pterygopalatine and submaxillary
ganglia to lachrymal glands and salivary glands (sublingual, submandibular), respectively; (3) through the ninth cranial nerve (glossopharyngeal n.) via the otic ganglion to the parotid gland; and (4) via the tenth cranial nerve (vagus n.) to intramural ganglia in thoracic and abdominal viscera. Approximately 75% of all parasympathetic fibers are contained within the vagus nerve. The neurons of the sacral division innervate the distal colon, rectum, bladder, the distal ureters, and the external genitalia.
Acetylcholine (ACh) as a transmitter. ACh serves as mediator at terminals of all postganglionic parasympathetic fibers, in addition to fulfilling its transmitter role at ganglionic synapses within both the sympathetic and parasympathetic divisions and the motor end plates on striated muscle (p.182). However, different types of receptors are present at these synaptic junctions (see table). The existence of distinct cholinoceptors at different cholinergic synapses allows selective pharmacological interventions.
Localization of Receptors |
Agonist |
Antagonist |
Receptor Type |
|
|
|
|
|
|
Target tissues of 2nd para- |
ACh |
Atropine |
Muscarinic (M) cholino- |
|
sympathetic neurons; e.g., |
Muscarine |
|
ceptor; G-protein-coupled |
|
smooth muscle, glands |
|
|
receptor protein with 7 |
|
|
|
|
transmembrane domains |
|
|
|
|
|
|
Sympathetic & parasympa- |
ACh |
Trimethaphan |
¸ |
Ganglionic type |
thetic gangliocytes |
Nicotine |
|
Ô |
Nicotinic (N) cholinocep- |
|
|
|
Ô |
|
|
|
|
|
|
Motor end plate in skeletal |
ACh |
d-Tubocurarine |
˝ |
tor ligand-gated cation |
muscle |
Nicotine |
|
Ô |
channel |
|
|
|
Ô |
|
|
|
|
˛ |
Muscle type |
|
|
|
|
|
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
Parasympathetic Nervous System |
103 |
A. Responses to parasympathetic activation |
Eyes: |
Accommodation |
for near vision, |
miosis |
Saliva: |
copious, liquid |
Bronchi: |
constriction |
secretion |
Heart: |
rate |
blood pressure |
GI tract: |
secretion |
peristaltis |
sphincter tone |
Bladder: |
sphincter tone |
detrusor |
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.

104 Drugs Acting on the Parasympathetic Nervous System
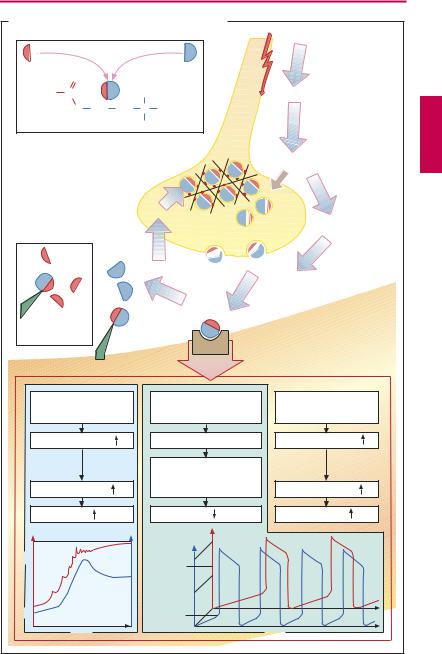
Cholinergic Synapse
Acetylcholine (ACh) is the transmitter at postganglionic synapses of parasympathetic nerve endings. It is highly concentrated in synaptic storage vesicles densely present in the axoplasm of the presynaptic terminal. ACh is formed from choline and activated acetate (acetylcoenzyme A), a reaction catalyzed by the cytosolic enzyme choline acetyltransferase. The highly polar choline is taken up into the axoplasm by the specific choline-transporter (CHT) localized to membranes of cholinergic axons terminals and a subset of storage vesicles. During persistent or intensive stimulation, the CHT ensures that ACh synthesis and release are sustained. The newly formed ACh is loaded into storage vesicles by the vesicular ACh transporter (VAChT). The mechanism of transmitter release is not known in full detail. The vesicles are anchored via the protein synapsin to the cytoskeletal network. This arrangement permits clustering of vesicles near the presynaptic membrane while preventing fusion with it. During activation of the nerve membrane, Ca2+ is thought to enter the axoplasm through voltage-gated channels and to activate protein kinases that phosphorylate synapsin. As a result, vesicles close to the membrane are detached from their anchoring and allowed to fuse with the presynaptic membrane. During fusion, vesicles discharge their contents into the synaptic gap and simultaneously insert CHT into the plasma membrane. ACh quickly diffuses through the synaptic gap (the acetylcholine molecule is a little longer than 0.5 nm; the synaptic gap as narrow as 20–30 nm). At the postsynaptic effector cell membrane, ACh reacts with its receptors. As these receptors can also be activated by the alkaloid muscarine, they are referred to as muscarinic (M-) ACh receptors. In contrast, at ganglionic and motor end plate (p.182) ACh receptors, the action of ACh is mimicked by nicotine and, hence, mediated by nicotinic ACh receptors.
Released ACh is rapidly hydrolyzed and inactivated by a specific acetylcholinesterase, localized to preand postjunctional membranes (basal lamina of motor end plates), or by a less specific serum cholinesterase (butyrylcholinesterase), a soluble enzyme present in serum and interstitial fluid.
M-ACh receptors can be divided into five subtypes according to their molecular structure, signal transduction, and ligand af nity. Here, the M1, M2 and M3 receptor subtypes are considered. M1 receptors are present on nerve cells, e.g., in ganglia, where they enhance impulse transmission from preganglionic axon terminals to ganglion cells. M2 receptors mediate acetylcholine effects on the heart: opening of K+ channels leads to slowing of diastolic depolarization in sinoatrial pacemaker cells and a decrease in heart rate. M3 receptors play a role in the regulation of smooth muscle tone, e.g., in the gut and bronchi, where their activation causes stimulation of phospholipase C, membrane depolarization, and increase in muscle tone. M3 receptors are also found in glandular epithelia, which similarly respond with activation of phospholipase C and increased secretory activity. In the CNS, where all subtypes are present, ACh receptors serve diverse functions ranging from regulation of cortical excitability, memory and learning, pain processing, and brainstem motor control.
In bloodvessels,therelaxantaction ofACh on muscle tone is indirect, because it involves stimulation of M3-cholinoceptors on endothelial cells that respond by liberating NO (nitrous oxid = endothelium-derived relaxing factor). The latter diffuses into the subjacent smooth musculature, where it causes a relaxation of active tonus (p.124).
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
|
|
|
|
Cholinergic Synapse |
105 |
|
A. Acetylcholine: release, effects, and degradation |
|
|
||||
Acetyl-coenzyme A + choline |
Action potential |
|
||||
|
Choline acetyltransferase |
|
||||
|
|
|
||||
|
O |
|
|
|
|
|
H3C |
C |
|
|
CH3 |
Ca2+ influx |
|
|
O |
CH |
CH |
N+ CH |
|
|
|
|
2 |
2 |
3 |
|
|
|
Acetylcholine |
CH3 |
|
|
||
|
|
|
Storage of |
Ca2+ |
|
|
|
|
|
acetylcholine |
|
|
|
|
|
|
in vesicles |
|
|
|
|
|
active |
|
Vesicle |
|
|
|
|
reuptake of |
|
|||
|
|
choline |
|
release |
|
|
|
|
|
|
|
Exocytosis |
|
|
|
|
|
esteric |
Receptor |
|
|
|
|
|
cleavage |
occupation |
|
Serum- |
|
|
Acetylcholine |
|
|
|
cholinesterase |
|
|
|
|||
|
|
|
esterase: |
|
|
|
|
|
|
membrane- |
|
|
|
|
|
|
associated |
|
|
|
Smooth muscle cell |
Heart pacemaker cell |
Secretory cell |
|
|||
M3-receptor |
|
M2-receptor |
M3-receptor |
|
||
Phospholipase C |
|
K+-channel activation |
Phospholipase C |
|
||
|
|
|
|
Slowing of |
|
|
Ca2+ in cytosol |
|
diastolic |
Ca2+ in cytosol |
|
||
|
depolarization |
|
||||
|
Tone |
|
|
Rate |
Secretion |
|
|
|
|
|
mV |
|
|
|
|
|
|
0 |
|
|
-30 |
|
|
|
ACh |
|
|
|
|
|
effect |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
-45 |
|
|
mV |
|
|
mN |
-90 |
|
|
-70 |
|
|
|
|
|
|
|
|
|
Control |
|
|
|
|
|
|
|
condition |
|
|
|
Time |
|
|
|
Time |
|
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
