
- •Preface to the 3rd edition
- •General Pharmacology
- •Systems Pharmacology
- •Therapy of Selected Diseases
- •Subject Index
- •Abbreviations
- •General Pharmacology
- •History of Pharmacology
- •Drug and Active Principle
- •The Aims of Isolating Active Principles
- •European Plants as Sources of Effective Medicines
- •Drug Development
- •Congeneric Drugs and Name Diversity
- •Oral Dosage Forms
- •Drug Administration by Inhalation
- •Dermatological Agents
- •From Application to Distribution in the Body
- •Potential Targets of Drug Action
- •External Barriers of the Body
- •Blood–Tissue Barriers
- •Membrane Permeation
- •Binding to Plasma Proteins
- •The Liver as an Excretory Organ
- •Biotransformation of Drugs
- •Drug Metabolism by Cytochrome P450
- •The Kidney as an Excretory Organ
- •Presystemic Elimination
- •Drug Concentration in the Body as a Function of Time—First Order (Exponential) Rate Processes
- •Time Course of Drug Concentration in Plasma
- •Time Course of Drug Plasma Levels during Repeated Dosing (A)
- •Time Course of Drug Plasma Levels during Irregular Intake (B)
- •Accumulation: Dose, Dose Interval, and Plasma Level Fluctuation (A)
- •Dose–Response Relationship
- •Concentration–Effect Curves (B)
- •Concentration–Binding Curves
- •Types of Binding Forces
- •Agonists—Antagonists
- •Other Forms of Antagonism
- •Enantioselectivity of Drug Action
- •Receptor Types
- •Undesirable Drug Effects, Side Effects
- •Drug Allergy
- •Cutaneous Reactions
- •Drug Toxicity in Pregnancy and Lactation
- •Pharmacogenetics
- •Placebo (A)
- •Systems Pharmacology
- •Sympathetic Nervous System
- •Structure of the Sympathetic Nervous System
- •Adrenergic Synapse
- •Adrenoceptor Subtypes and Catecholamine Actions
- •Smooth Muscle Effects
- •Cardiostimulation
- •Metabolic Effects
- •Structure–Activity Relationships of Sympathomimetics
- •Indirect Sympathomimetics
- •Types of
- •Antiadrenergics
- •Parasympathetic Nervous System
- •Cholinergic Synapse
- •Parasympathomimetics
- •Parasympatholytics
- •Actions of Nicotine
- •Localization of Nicotinic ACh Receptors
- •Effects of Nicotine on Body Function
- •Aids for Smoking Cessation
- •Consequences of Tobacco Smoking
- •Dopamine
- •Histamine Effects and Their Pharmacological Properties
- •Serotonin
- •Vasodilators—Overview
- •Organic Nitrates
- •Calcium Antagonists
- •ACE Inhibitors
- •Drugs Used to Influence Smooth Muscle Organs
- •Cardiac Drugs
- •Cardiac Glycosides
- •Antiarrhythmic Drugs
- •Iron Compounds
- •Prophylaxis and Therapy of Thromboses
- •Possibilities for Interference (B)
- •Heparin (A)
- •Hirudin and Derivatives (B)
- •Fibrinolytics
- •Intra-arterial Thrombus Formation (A)
- •Formation, Activation, and Aggregation of Platelets (B)
- •Inhibitors of Platelet Aggregation (A)
- •Presystemic Effect of ASA
- •Plasma Volume Expanders
- •Lipid-lowering Agents
- •Diuretics—An Overview
- •NaCl Reabsorption in the Kidney (A)
- •Aquaporins (AQP)
- •Osmotic Diuretics (B)
- •Diuretics of the Sulfonamide Type
- •Potassium-sparing Diuretics (A)
- •Vasopressin and Derivatives (B)
- •Drugs for Gastric and Duodenal Ulcers
- •Laxatives
- •Antidiarrheal Agents
- •Drugs Affecting Motor Function
- •Muscle Relaxants
- •Nondepolarizing Muscle Relaxants
- •Depolarizing Muscle Relaxants
- •Antiparkinsonian Drugs
- •Antiepileptics
- •Pain Mechanisms and Pathways
- •Eicosanoids
- •Antipyretic Analgesics
- •Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- •Cyclooxygenase (COX) Inhibitors
- •Local Anesthetics
- •Opioid Analgesics—Morphine Type
- •General Anesthesia and General Anesthetic Drugs
- •Inhalational Anesthetics
- •Injectable Anesthetics
- •Sedatives, Hypnotics
- •Benzodiazepines
- •Pharmacokinetics of Benzodiazepines
- •Therapy of Depressive Illness
- •Mania
- •Therapy of Schizophrenia
- •Psychotomimetics (Psychedelics, Hallucinogens)
- •Hypothalamic and Hypophyseal Hormones
- •Thyroid Hormone Therapy
- •Glucocorticoid Therapy
- •Follicular Growth and Ovulation, Estrogen and Progestin Production
- •Oral Contraceptives
- •Antiestrogen and Antiprogestin Active Principles
- •Aromatase Inhibitors
- •Insulin Formulations
- •Treatment of Insulin-dependent Diabetes Mellitus
- •Treatment of Maturity-Onset (Type II) Diabetes Mellitus
- •Oral Antidiabetics
- •Drugs for Maintaining Calcium Homeostasis
- •Drugs for Treating Bacterial Infections
- •Inhibitors of Cell Wall Synthesis
- •Inhibitors of Tetrahydrofolate Synthesis
- •Inhibitors of DNA Function
- •Inhibitors of Protein Synthesis
- •Drugs for Treating Mycobacterial Infections
- •Drugs Used in the Treatment of Fungal Infections
- •Chemotherapy of Viral Infections
- •Drugs for the Treatment of AIDS
- •Drugs for Treating Endoparasitic and Ectoparasitic Infestations
- •Antimalarials
- •Other Tropical Diseases
- •Chemotherapy of Malignant Tumors
- •Targeting of Antineoplastic Drug Action (A)
- •Mechanisms of Resistance to Cytostatics (B)
- •Inhibition of Immune Responses
- •Antidotes and Treatment of Poisonings
- •Therapy of Selected Diseases
- •Hypertension
- •Angina Pectoris
- •Antianginal Drugs
- •Acute Coronary Syndrome— Myocardial Infarction
- •Congestive Heart Failure
- •Hypotension
- •Gout
- •Obesity—Sequelae and Therapeutic Approaches
- •Osteoporosis
- •Rheumatoid Arthritis
- •Migraine
- •Common Cold
- •Bronchial Asthma
- •Emesis
- •Alcohol Abuse
- •Local Treatment of Glaucoma
- •Further Reading
- •Further Reading
- •Picture Credits
- •Drug Indexes

162 Diuretics
Diuretics—An Overview
Diuretics (saluretics) elicit increased production of urine (diuresis). In the strict sense, the term is applied to drugs with a direct renal action. The predominant action of such agents is to augment urine excretion by inhibiting the reabsorption of NaCl and water.
The most important indications for diuretics are the following.
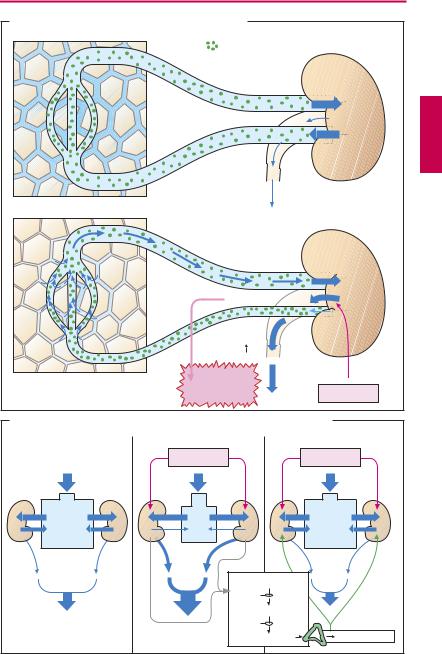
Mobilization of edemas (A). In edema there is swelling of tissues owing to accumulation of fluid, chiefly in the extracellular (interstitial) space. When a diuretic is given, increased renal excretion of Na+ and H2O causes a reduction in plasma volume with hemoconcentration. As a result, plasma protein concentration rises along with oncotic pressure. As the latter operates to attract water, fluid will shift from interstitium into the capillary bed. The fluid content of tissues thus falls and the edemas recede. The decrease in plasma volume and interstitial volume means a diminution of the extracellular fluid volume (EFV). Depending on the condition, use is made of thiazides, loop diuretics, aldosterone antagonists, and osmotic diuretics.
Antihypertensive therapy. Diuretics have been used as drugs of first choice for lowering elevated blood pressure (p.314). Even at low dosage, they decrease peripheral resistance (without significantly reducing EFV) and thereby normalize blood pressure.
Therapy of congestive heart failure. By lowering peripheral resistance, diuretics aid the heart in ejecting blood (reduction in afterload, p.322); cardiac output and exercise tolerance are increased. Owing to the increased excretion of fluid, EFV and venous return decrease (reduction in preload). Symptoms of venous congestion, such as ankle edema and hepatic enlargement, subside. The drugs principally used are thiazides (possibly combined with K+-sparing diuretics) and loop diuretics.
Prophylaxis of renal failure. In circulatory failure (shock), e.g., secondary to mas-
sive hemorrhage, renal production of urine may cease (anuria). By means of diuretics, an attempt is made to maintain urinary flow. Use of either osmotic or loop diuretics is indicated.
Massive use of diuretics entails a hazard of adverse effects (A):
1.The decrease in blood volume can lead to hypotension and collapse.
2.Blood viscosity rises owing to the increase in erythrocyte and thrombocyte concentrations, bringing an increased risk of in-
travascular coagulation or thrombosis. When depletion of NaCl and water (EFV reduction) occurs as a result of diuretic therapy, the body can initiate counterregulatory responses (B), namely, activation of the renin–angiotensin–aldosterone system (p.128). Because of the diminished blood volume, renal blood flow is jeopardized. This leads to release from the kidneys of the hormone renin, which enzymatically catalyzes the formation of angiotensin I. Angiotensin I is converted to angiotensin II by the action of “angiotensin-converting enzyme” (ACE). Angiotensin II stimulates release of aldosterone. The mineralocorticoid promotes renal reabsorption of NaCl and water and thus counteracts the effect of diuretics. ACE inhibitors (p.128) and angiotensin II antagonists augment the effectiveness of diuretics by preventing this counterregulatory response.
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
|
Diuretics—An Overview |
163 |
|
A. Mechanism of edema fluid mobilization by diuretics |
|
|
|
|
Protein molecules |
|
|
Edema |
|
|
|
|
Hemoconcentration |
|
|
|
Colloid- |
|
|
|
osmotic |
|
|
|
pressure |
|
|
Mobilization of |
Collapse, |
|
|
danger of |
Diuretic |
|
|
edema fluid |
thrombosis |
|
|
B. Possible counter-regulatory responses during long-term diuretic therapy
Salt and |
Diuretic |
Diuretic |
|
fluid retention |
|||
|
|
||
EFV: |
|
|
|
Na+, Cl-, |
|
|
|
H2O |
|
|
|
|
Angiotensinogen |
|
|
|
Renin |
|
|
|
Angiotensin I |
|
|
|
ACE |
|
|
|
Angiotensin II |
Aldosterone |
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.

164 Diuretics
NaCl Reabsorption in the Kidney (A)
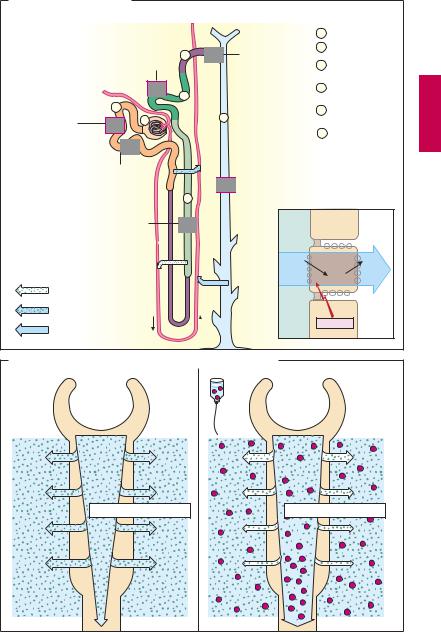
The smallest functional unit of the kidney is the nephron. In the glomerular capillary loops, ultrafiltration of plasma fluid into Bowman’s capsule yields primary urine. In the proximal tubules (pT), ~ 70% of the ultrafiltrate is retrieved by iso-osmotic reabsorption of NaCl and water. Downstream, in the thick portion of the ascending limb of Henle’s loop, NaCl is absorbed unaccompanied by water. The differing properties of the limbs of Henle’s loop, together with the parallel arrangement of vasa recta, are the prerequisites for the hairpin countercurrent mechanism that allows build-up of a very high NaCl concentration in the renal medulla. NaCl is again reabsorbed in the distal convoluted tubules, the connecting segment, and the collecting ducts, accompanied by a compensatory secretion of K+ in the (cortical) collecting tubules. In the connecting tubules and collecting ducts, vasopressin (antidiuretic hormone, ADH) increases the epithelial permeability for water by insertion of aquaporin molecules into the luminal plasmalemma. The driving force for the passage of water comes from the hyperosmolar milieu of the renal medulla. In this manner, water is retained in the body, and concentrated urine can leave the kidney. The ef - cient mechanisms of reabsorption permit the production of ~ 1 l/day of final urine from 150–180 l/day of primary urine.
Na+ transport through the tubular cells basically occurs in similar fashion in all segments of the nephron. The intracellular concentration of Na+ is significantly below that in primary urine because the Na+/K+-ATPase of the basolateral membrane continuously pumps Na+ fromthecellintotheinterstitium. Along the resulting luminal–intracellular concentrationgradient,movementofsodium ions across the membrane proceeds bya carrier mechanism. All diuretics inhibit Na+ reabsorption. Thiseffectisbasedontwomechanisms: either the inward movement is diminishedorthe outwardtransportimpaired.
Aquaporins (AQP)
By virtue of their structure, cell membranes are water-impermeable. Therefore, special pores are built into the membrane to allow permeation of water. These consist of proteins called aquaporins that, of necessity, occur widely and with many variations in both the plant and animal kingdoms. In the human kidney, the following types exist:
AQP-1 localized in the proximal tubulus and the descending limb of Henle’s loop.
AQP-2 localized in the connecting tubuli and collecting ducts; its density in the luminal plasmalemma is regulated by vasopressin.
AQP-3 and AQP-4 present in the basolateral membrane region to allow passage of water into the interstitium.
Osmotic Diuretics (B)
These include mannitol and sorbitol which act mainly in the proximal tubules to prevent reabsorption of water. These polyhydric alcohols cannot be absorbed and therefore bind a corresponding volume of water. Since body cells lack transport mechanisms for these substances (structure on p.175), they also cannot be absorbed through the intestinal epithelium and thus need to be given by intravenous infusion. The result of osmotic diuresis is a large volume of dilute urine, as in decompensated diabetes mellitus. Osmotic diuretics are indicated in the prophylaxis of renal hypovolemic failure, the mobilization of brain edema, and the treatmentofacute glaucomaattacks(p.346).
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
NaCl Reabsorption in the Kidney |
165 |
A. Renal actions of diuretics
Na+, Cl- transport (thiazide diuretics)
Reabsorption
of Na+, H2O and many other
constituents of |
2 |
primary urine |
1 |
Carbonic anhydrase mechanism (acetazolamide)
|
Inward Na+ |
1 |
Glomerulus |
|
|
current linked |
2 |
Prox. tubule |
|
5 |
to K+ channel |
|||
|
|
|||
|
(amiloride) |
3 |
Distal tubule |
|
|
outward current |
|
pars recta |
|
4 |
Aldosterone |
4 |
Dist. tubule |
|
increases |
|
pars contorta |
||
|
|
|
||
6 |
synthesis of |
5 |
Connecting tubule |
|
channels |
|
|
||
|
|
6 |
Collecting duct |
Aquaporin 2 (vasopressin increases 
 expression): H2O uptake
expression): H2O uptake
|
|
|
|
|
3 |
|
|
|
|
Na+, K+, |
|
|
|
|
|
|
|||
2Cl- cotransport |
|
Lumen |
|
|
Inter- |
||||
(loop diuretics) |
|
|
|
|
stitium |
||||
|
|
|
|
|
|
Na+ |
“carrier” |
Na+ |
|
|
|
|
|
|
|
|
|
Na+ |
Na/K- |
|
|
|
|
|
|
|
|
ATPase |
|
Na+, Cl- |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Na+, Cl- + H |
2 |
O |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
H2O |
|
|
|
|
|
|
Diuretics |
|
|
|
|
|
|
|
|
|
|
|
|
B. NaCl reabsorption in proximal tubule and effect of mannitol |
|
|
|
|
|||||
|
|
|
|
|
Mannitol |
|
|
|
|
[Na+] |
inside |
= [Na+] |
outside |
[Na+] |
inside |
< [Na+] |
outside |
||
Luellmann, Color Atlas of Pharmacology © 2005 Thieme
All rights reserved. Usage subject to terms and conditions of license.
