
- •VOLUME 1
- •CONTRIBUTOR LIST
- •PREFACE
- •LIST OF ARTICLES
- •ABBREVIATIONS AND ACRONYMS
- •CONVERSION FACTORS AND UNIT SYMBOLS
- •ABLATION.
- •ABSORBABLE BIOMATERIALS.
- •ACRYLIC BONE CEMENT.
- •ACTINOTHERAPY.
- •ADOPTIVE IMMUNOTHERAPY.
- •AFFINITY CHROMATOGRAPHY.
- •ALLOYS, SHAPE MEMORY
- •AMBULATORY MONITORING
- •ANALYTICAL METHODS, AUTOMATED
- •ANALYZER, OXYGEN.
- •ANESTHESIA MACHINES
- •ANESTHESIA MONITORING.
- •ANESTHESIA, COMPUTERS IN
- •ANGER CAMERA
- •ANGIOPLASTY.
- •ANORECTAL MANOMETRY
- •ANTIBODIES, MONOCLONAL.
- •APNEA DETECTION.
- •ARRHYTHMIA, TREATMENT.
- •ARRHYTHMIA ANALYSIS, AUTOMATED
- •ARTERIAL TONOMETRY.
- •ARTIFICIAL BLOOD.
- •ARTIFICIAL HEART.
- •ARTIFICIAL HEART VALVE.
- •ARTIFICIAL HIP JOINTS.
- •ARTIFICIAL LARYNX.
- •ARTIFICIAL PANCREAS.
- •ARTERIES, ELASTIC PROPERTIES OF
- •ASSISTIVE DEVICES FOR THE DISABLED.
- •ATOMIC ABSORPTION SPECTROMETRY.
- •AUDIOMETRY
- •BACTERIAL DETECTION SYSTEMS.
- •BALLOON PUMP.
- •BANKED BLOOD.
- •BAROTRAUMA.
- •BARRIER CONTRACEPTIVE DEVICES.
- •BIOCERAMICS.
- •BIOCOMPATIBILITY OF MATERIALS
- •BIOELECTRODES
- •BIOFEEDBACK
- •BIOHEAT TRANSFER
- •BIOIMPEDANCE IN CARDIOVASCULAR MEDICINE
- •BIOINFORMATICS
- •BIOLOGIC THERAPY.
- •BIOMAGNETISM
- •BIOMATERIALS, ABSORBABLE
- •BIOMATERIALS: AN OVERVIEW
- •BIOMATERIALS: BIOCERAMICS
- •BIOMATERIALS: CARBON
- •BIOMATERIALS CORROSION AND WEAR OF
- •BIOMATERIALS FOR DENTISTRY
- •BIOMATERIALS, POLYMERS
- •BIOMATERIALS, SURFACE PROPERTIES OF
- •BIOMATERIALS, TESTING AND STRUCTURAL PROPERTIES OF
- •BIOMATERIALS: TISSUE-ENGINEERING AND SCAFFOLDS
- •BIOMECHANICS OF EXERCISE FITNESS
- •BIOMECHANICS OF JOINTS.
- •BIOMECHANICS OF SCOLIOSIS.
- •BIOMECHANICS OF SKIN.
- •BIOMECHANICS OF THE HUMAN SPINE.
- •BIOMECHANICS OF TOOTH AND JAW.
- •BIOMEDICAL ENGINEERING EDUCATION
- •BIOSURFACE ENGINEERING
- •BIOSENSORS.
- •BIOTELEMETRY
- •BIRTH CONTROL.
- •BLEEDING, GASTROINTESTINAL.
- •BLADDER DYSFUNCTION, NEUROSTIMULATION OF
- •BLIND AND VISUALLY IMPAIRED, ASSISTIVE TECHNOLOGY FOR
- •BLOOD BANKING.
- •BLOOD CELL COUNTERS.
- •BLOOD COLLECTION AND PROCESSING
- •BLOOD FLOW.
- •BLOOD GAS MEASUREMENTS
- •BLOOD PRESSURE MEASUREMENT
- •BLOOD PRESSURE, AUTOMATIC CONTROL OF
- •BLOOD RHEOLOGY
- •BLOOD, ARTIFICIAL
- •BONDING, ENAMEL.
- •BONE AND TEETH, PROPERTIES OF
- •BONE CEMENT, ACRYLIC
- •BONE DENSITY MEASUREMENT
- •BORON NEUTRON CAPTURE THERAPY
- •BRACHYTHERAPY, HIGH DOSAGE RATE
- •BRACHYTHERAPY, INTRAVASCULAR
- •BRAIN ELECTRICAL ACTIVITY.
- •BURN WOUND COVERINGS.
- •BYPASS, CORONARY.
- •BYPASS, CARDIOPULMONARY.
42 ANESTHESIA, COMPUTERS IN
control. Many new anesthesia ventilators offer multiple modes of ventilation (in addition to the traditional volume control), such as pressure control, pressure support, and synchronized intermittent mandatory ventilation. These modes assess patient effort using electronic flow and pressure sensors that are included in many new breathing circuits. Lastly, some anesthesia ventilators use an electronically controlled piston instead of the traditional pneumatically compressed bellows. Piston ventilators, which are electrically powered, dramatically decrease compressed gas consumption of the anesthesia delivery system. However, they actively draw gas out of the breathing circuit during the expiratory cycle (as opposed to bellows, which fill passively) so they cannot be used with a traditional circle system (see Fig. 7 for an example of a piston ventilator used with a fresh gas decoupled breathing circuit).
AUTOMATED CHECKOUT
Many new anesthesia delivery systems feature semiautomated preuse checkout procedures. These ensure that the machine is functioning properly prior to use by (1) testing electronic and computer performance, (2) calibrating flow sensors and oxygen monitors, (3) measuring breathing circuit compliance and leakage, and (4) testing the ventilator.
Future Challenges
The current trend is to design machines that provide advanced capabilities through the use of computerized electronic monitoring and controls. This provides the infrastructure for features such as closed-loop feedback, smart alarms, and information management that will be increasingly incorporated in the future. We can anticipate closedloop controllers that automatically maintain a user-set exhaled anesthetic concentration (an indicator of anesthetic depth), or exhaled carbon dioxide concentration (an indicator of adequacy of ventilation). We can look forward to smart alarms that pinpoint the location of leaks or obstructions in the breathing circuit, alert the user and switch to a different anesthetic when a vaporizer becomes empty, or notify the user and switch to a backup cylinder if a pipeline failure or contamination event is detected. We can foresee information management systems that automatically incorporate anesthesia machine settings into a nationwide repository of anesthesia records that facilitate outcomes-guided medical practice, critical event investigations, and nationwide access to patient medical records. Anesthesia machine technology continues to evolve.
BIBLIOGRAPHY
Cited References
1.ASTM F1850. Standard Specification for Particular Requirements for Anesthesia Workstations and Their Components. ASTM International; 2000.
2.ISO 5358. Anaesthetic machines for use with humans. International Organization for Standardization; 1992.
3.ISO 8835-2. Inhalational anaesthesia systems—Part 2: Anaesthetic breathing systems for adults. International Organization for Standardization; 1999.
4.ISO 8835-3. Inhalational anaesthesia systems—Part 3: Anaesthetic gas scavenging systems—Transfer and receiving systems. International Organization for Standardization; 1997.
5.ISO 8835-4. Inhalational anaesthesia systems—Part 4: Anaesthetic vapour delivery devices. International Organization for Standardization; 2004.
6.ISO 8835-5. Inhalational anaesthesia systems—Part 5: Anaesthetic ventilators. International Organization for Standardization; 2004.
7.Anesthesia Apparatus Checkout Recommendations. United States Food and Drug Administration. Available at http:// www.fda.gov//cdrh/humfac//anesckot.html. 1993.
8.Standards for Basic Anesthetic Monitoring, American Society of Anesthesiologists. Available at http://www.asahq.org/publicationsAndServices/standards/02.pdf. Accessed 2004.
9.CGA V-5. Diameter Index Safety System (Noninterchangeable Low Pressure Connections for Medical Gas Applications). Compressed Gas Association; 2000.
10.CGA V-1. Compressed Gas Association Standard for Compressed Gas Cylinder Valve Outlet and Inlet Connections. Compressed Gas Association; 2003.
Reading List
Dorsch J, Dorsch S. Understanding Anesthesia Equipment. 4th ed. Williams & Wilkins; 1999.
Brockwell RC, Andrews JJ. Inhaled Anesthetic Delivery Systems. In: Miller RD. et al. editors. Miller’s Anesthesia. 6th ed. Philadelphia: Elsevier Churchill Livingstone; 2005.
Ehrenwerth J, Eisenkraft JB, editors. Anesthesia Equipment: Principles and Applications. St. Louis: Mosby; 1993
Lampotang S, Lizdas D, Liem EB, Dobbins W. The Virtual Anesthesia Machine. http://vam.anest.ufl.edu/.
See also CONTINUOUS POSITIVE AIRWAY PRESSURE; EQUIPMENT ACQUISITION; EQUIPMENT MAINTENANCE, BIOMEDICAL; GAS AND VACUUM SYSTEMS,
CENTRALLY PIPED MEDICAL; VENTILATORY MONITORING.
ANESTHESIA MONITORING. See MONITORING IN
ANESTHESIA.
ANESTHESIA, COMPUTERS IN
LE YI WANG
HONG WANG
Wayne State University
Detroit, Michigan
INTRODUCTION
Computer applications in anesthesia patient care have evolved with advancement of computer technology, information processing capability, and anesthesia devices and procedures.
Anesthesia is an integral part of most surgical operations. The objectives of anesthesia are to achieve hypnosis (consciousness control), analgesia (pain control), and immobility (body movement control) simultaneously throughout surgical operations, while maintaining the vital functions of the body. Vital functions, such as respiration and circulation of blood, are assessed by signs such as blood pressures, heart rate, end-tidal carbon dioxide (CO2), oxygen saturation by pulse oximetry (SpO2), and so on. These objectives are

ANESTHESIA, COMPUTERS IN |
43 |
Figure 1. Some anesthesia equipment in an operating room.
carefully balanced and maintained by a dedicated anesthesia provider using a combination of sedative agents, hypnotic drugs, narcotic drugs, and, in many surgeries, muscle relaxants. Anesthesia decisions and management are complicated tasks, in which anesthetic requirements and agent dosages depend critically on the surgical procedures, the patient’s medical conditions, drug interactions, and coordinated levels of anesthesia depth and physiological variables. Anesthesia decisions impact significantly on surgery and patient outcomes, drug consumptions, hospital stays, and therefore quality of patient care and healthcare cost (Fig. 1).
Computer technologies have played essential roles in assisting and improving patient care in anesthesia. Development of computer technology started from its early stages of bulky computing machines, progressed to minicomputers and microcomputers, exploded with its storage capability and computational speed, and evolved into multiprocessor systems, distributed systems, computer networks, and multimedia systems. Computer applications in anesthesia have taken advantage of this technology advancement. Early computer applications in medicine date back to the late 1950s when some hospitals began to develop computer data processing systems to assist administration, such as storage, management, and analysis of patient and procedural data and records. The main goals were to reduce manpower in managing ever-growing patient data, patient and room scheduling, anesthesia supply tracking, and billing. During the past four decades computer utility in anesthesia has significantly progressed to include computer-controlled fluid administration and drug dispersing, advanced anesthesia monitoring, anesthesia information systems, computerassisted anesthesia control, computer-assisted diagnosis and decisions, and telemedicine in anesthesia.
COMPUTER UTILITY IN ADVANCED ANESTHESIA MONITORING
The quality of anesthesia patient care has been greatly influenced by monitoring technology development. A
Figure 2. Anesthesia monitoring devices without computer technologies. (Courtsey of Sheffield Museum of Anesthesia used with permission.)
patient’s state during a surgery is assessed using vital signs. In earlier days of anesthesiology, vital signs were limited to manual measurements of blood pressures, stethoscope auscultation of heart–lung sounds, and heart rates. These values were measured intermittently and as needed during surgery. Thanks to advancement of materials, sensing methods, and signal processing techniques, many vital signs can now be directly, accurately, and continuously measured. For example, since the invention of pulse oximetry in the early 1980s, this noninvasive method of continuously monitoring the arterial oxygen saturation level in a patient’s blood (SpO2) has become a standard method in the clinical environment, resulting in a significant improvement of patient safety. Before this invention, blood must be drawn from patients and analyzed using laboratory equipment.
Integrating these vital signs into a comprehensive anesthesia monitoring system has been achieved by computer data interfacing, multisignal processing, and computer graphics. Advanced anesthesia monitors are capable of acquiring multiple signals from many vital sign sensors and anesthesia machine itself, displaying current readings and historic trends, and providing audio and visual warning signals. At present, heart rate, electrocardiogram (ECG), arterial blood pressures, temperature, ventilation parameters (inspired–expired gas concentration, peak airway pressure, plateau airway pressure, inspired and expired volumes, etc.), end-tidal CO2 concentrations, blood oxygen saturation (SpO2), and so on, are routinely and reliably monitored (Figs. 2 and 3).
However, there are still many other variables reflecting a patient’s state that must be inferred by the physician, such as anesthesia depth and pain intensity. Pursuit of new
Figure 3. An anesthesia monitor from GE Healthcare in 2005. (Courtsey of GE Healthcare.)
44 ANESTHESIA, COMPUTERS IN
physiological monitoring devices for direct and reliable measurements of some of these variables is of great value and imposes great challenges at the same time (1). Anesthesia depth has become a main focus of research in the anesthesia field. At present, most methods rely in part or in whole on processing of the electroencephalogram (EEG) and frontalis electromyogram (FEMG) signals. Proposed methods include the median frequency, spectral edge frequency, visual evoked potential, auditory evoked potential, entropy, and bispectral index (2,3). Some of these technologies have been commercialized, leading to several anesthesia depth monitors for use in general anesthesia and sedation. Rather than using indirect implications from blood pressures, heart rate, and involuntary muscle movements to derive consciousness levels, these monitors purport to give a direct index of a patient’s anesthesia depth. Consequently, combined effects of anesthesia drugs on the patient anesthesia depth can potentially be understood clearly and unambiguously. Currently (the year 2005), the BIS Monitor by Aspect Medical Systems, Inc. (www.aspectmedical.com), Entropy Monitor by GE Healthcare (www.gehealthcare. com), and Patient State Analyzer (PSA) by Hospira, Inc. (www.hospira.com) are three FDA (U.S. Food and Drug Administration) approved commercial monitors for anesthesia depth.
Availability of commercialized anesthesia depth monitors has prompted a burst of research activity on computerized depth control. Improvement of their reliability remains a research frontier. Artifacts have fundamental impact on reliability of EEG signals. In particular, muscle movements, eye blinks, and other neural stimulation effects corrupt EEG signals, challenging all the methods that rely on EEG to derive anesthesia depth. As a result, reliability of these devices in intensive care units (ICU) and emergency medicine remains to be improved.
Another area of research is pain-intensity measurement and monitoring. Despite a long history of research and development, pain intensity is still evaluated by subjective assessment and patient self-scoring. The main thrust is to establish the relation between subjective pain scores, such as the visual analog scale (VAS) system, and objective measures of vital signs. Computer-generated objective and continuous monitoring of pain will be a significant advance in anesthesia pain control. This remains an open and active area of research and development (R&D). As an intermediate step, patient-controlled analgesia (PCA) devices have been developed (see, e.g., LifeCare PCA systems from Hospira, Inc., which is a 2003 spin-off of Abbott Laboratories) that allow a patient to assess his/her pain intensity and control analgesia as needed.
Currently, anesthesia monitors are limited to data recording and patient state display. Also, their basic functions do not offer substantial interaction with human and environment. Future monitors must enhance fundamentally human-factors design: Intelligent human–machine interface and integrated human–machine–environment systems (4). Ideally, a monitor will intelligently organize observation data into useful information, adapt its functions according to surgical and anesthesia events, select the most relevant information to display, modify its display layouts to reduce distraction and amplify essential
information, tune safety boundaries for its warning systems on the basis of the individual medical conditions of the patient, analyze data to help diagnosis and treatment, and allow user-friendly interactive navigation of the monitor system. Such a monitor will eventually become an extension of a physician’s senses and an assistant of decision-making processes.
COMPUTER INFORMATION TECHNOLOGY IN ANESTHESIA
Anesthesia Information Systems
Patient information processing systems have undergone a long history of evolution. Starting in the 1960s, some computer programming software and languages were introduced to construct patient information systems. One example is MUMPS (Massachusetts General Hospital Utility Multi-Programming System), which was developed in Massachusetts General Hospital and used by other hospitals, as well as the U.S. Department of Defense and the U.S. Veteran’s Administration. During the same period, Duke University’s GEMISCH, a multi-user database programming language, was created to streamline data sharing and retrieval capabilities.
Currently, a typical anesthesia information system (AIS) consists of a central computer station or a server that is interconnected via wired or wireless data communication networks to many subsystems. Subsystems include anesthesia monitors and record-keeping systems in operating rooms, preoperative areas, postanesthesia care units (PACU), ICUs; data entry and record systems of hospital testing labs; office computers of anesthesiologists. The system also communicates with hospital mainframe information systems to further exchange information with inand out-patient care services, patient database, and billing systems.
Information from an operating room is first collected by medical devices and anesthesia monitors and locally sorted and recorded in the record-keeping system. Selected data are then transmitted to the mainframe server through the data network. Anesthesia events, procedures, physician observations and diagnosis, patient care plans, testing results, drug and fluid data can also be entered into the record-keeping system, and broadcast to the main server and/or other related subsystems.
The main server and observation station provide a center in which patient status in many operating rooms, preoperative area and PACUs can be simultaneously monitored in real time. More importantly, the central anesthesia information system keeps accurately patient data and makes them promptly accessible to many important functions, including patient care assessment, quality assurance, room scheduling, physician assignment, clinical studies, medical billing, regulation compliance, equipment and personnel utility, drug and blood inventory, postoperative in-patient and out-patient service, to name just a few examples (Fig. 4).
One example of AIS is the automation software system CareSuite of PICIS, Inc. (www.picis.com). The system delivers comprehensive perioperative automation. It provides surgical

ANESTHESIA, COMPUTERS IN |
45 |
and anesthesia supply management, intraoperative nursing notes, surgical infection control monitoring, adverse event tracking and intervention, patient tracking, resource tracking, outlier alerts, anesthesia record, anesthesia times, case compliance, and so on. Similarly, the surgical and anesthesia management software by Surgical Information Systems (SIS), Inc. (www.orsoftware.com) streamlines patient care and facilitates analysis and performance improvement.
Anesthesia information systems are part of an emerging discipline called medical informatics, which studies clinical information and clinical decision support systems. Although technology maturity of computer hardware and software has made medical information systems highly feasible, creating seamless exchange of information among disparate systems remain a difficult task. This presents new opportunities and challenges for broader application of medical informatics in anesthesia practice.
Computer Simulation: Human Patient Simulators
Human patient simulators (HPS) are computerized mannequins whose integrated mechanical systems and computer hardware, and sophisticated computer software mimic authentically many related physiological, pathological, and pharmacological aspects of the human patient during a surgery or a medical procedure (Fig. 5). The mannequins are designed to simulate an adult or pediatric patient of either gender under a medical stress condition. They are accommodated in a clinical setting, such as an operating room, a trauma site, an emergence suite, or an ICU. Infusion pumps use clean liquid (usually water) through bar-coded syringes, whose barcodes are read by the HPS code recognition system to identify the drugs, to administer the simulated drugs, infusion liquids, or transfused blood during an anesthesia administration. The HPS allows invasive procedures such as intubation.
The HPS responds comprehensively to administered drugs, surgical events, patient conditions, and medical crisis; and displays on standard anesthesia monitors most
Figure 4. An illustration of a surgical/ anesthesia information management system from surgical information systems, Inc. (www. orsoftware.com).
related physiological vital signs, including blood pressures, heart rate, EKG, and oxygen saturations. They also generate normal and adventurous heart and lung sounds for auscultation. All these characteristics are internally generated by the computer software that utilizes mathematics models of typical human patients to simulate the human responses. The patient’s physical parameters (age, weight, smoker, etc.), preexisting medical conditions (high blood pressure, asthma, diabetic, etc.), surgical procedures, clinical events, and critical conditions are easily programmed by a computer Scenario Editor with a user-friendly graphical interface. The Scenario Editor also allows interactive reprogramming of scenarios during an operation. This on-the-fly function of scenario generation is especially useful for training. It gives the instructor great flexibility to create new scenarios according to the trainee’s reactions to previous scenarios.
The HPS is a great educational tool that has been used extensively in training medical students, nurse anesthetists, anesthesia residents, emergency, and battlefield
Figure 5. Human patient simulator complex at Wayne State University.
46 ANESTHESIA, COMPUTERS IN
Figure 6. Anesthesia resident training on an HPS manufactured by METI, Inc. (Used with permission.)
medics. Its preliminary development can be traced back to the 1950s, with limited computer hardware or software. Its more comprehensive improvement occurred in pace with computer technology in the late 1960s when highly computerized models were incorporated into high fidelity HPS systems with interfaces to external computers.
Due to rareness of anesthesia crisis, student and resident training on frequent and repeated critical medical conditions and scenarios is not possible in operating rooms. The HPS permits the trainee to practice clinical skills and manage complex and critical clinical conditions by generating and repeating difficult medical scenarios. The instructor can design individualized programs to evaluate and improve trainees’ crisis management skills. For invasive skills, such as intubation, practice
on simulators is not harmful to human patients. Catastrophic or basic events are presented with many variations so that trainees can recognize their symptoms, diagnose their occurrences, treat them according to established guidelines, and avert disasters. For those students who have difficulties to transform classroom knowledge to clinical hands-on skills, the HPS training is a comfortable bridge for them to rehearse in simulated clinical environments (5) (Fig. 6).
There are several models of HPSs on market. For example, the MedSim-Eagle Patient Simulator (Fig. 7) is a realistic, hands-on simulator of the anesthetized or critically ill patient, developed at Stanford University and manufactured by Eagle Simulation, Inc. METI (Medical Education Technologies, Inc.) (www.meti.com) manufactures adult HPS (Stan), pediatric HPS (PediaSim), emergency care simulator (ECS), pediatric emergency simulator (PediaSim-ECS), and related simulation suites such as airway tools (AirSim), surgical training tools (SurgicalSim). Laerdal Medical AS (www.laerdal.com) has developed a comprehensive portable HPS that can be operated without the usual operating room settings for HPS operations.
Human simulations, however, are not a total reality. Regardless how comprehensive the HPS has become, real environments are far more complex. There are many complications that cannot be easily simulated. Consequences of overly aggressive handling of certain medical catastrophic events may not be fully represented. Issues like these have prompted further efforts in improving HPS technologies and enhancing their utilities in anesthesia education, training, and research.
Figure 7. A human patient simulator SimMan, by Laerdal Medical Corporation. (Used with permission.)

ANESTHESIA, COMPUTERS IN |
47 |
Large Area Computer Networks: Telemedicine in Anesthesia
Telemedicine can be used to deliver healthcare over geographically separated locations. High speed telecommunication systems allow interactive video-mediated clinical consultation, and the possibility in the future of remote anesthesia administration. Wide availability of high speed computer and wireless network systems have made telemedicine a viable area for computer applications. Telemedicine could enable the delivery of specialized anesthesia care to remote locations that may not be accessible to high quality anesthesia services and knowledge, may reduce significantly travel costs, and expand the supervision capability of highly trained anesthesiologists.
In a typical telemedicine anesthesia consultation, an anesthesiologist in the consultation center communicates by a high speed network with the patient and the local anesthesia care provider, such as a nurse, at the remote location (Fig. 8). Data, audio and video connections enable the parties to transfer data, conduct conversations on medical history and other consultation routines, share graphs, discuss diagnosis, and examine the patient by cameras. The anesthesiologist can evaluate the airway management, ventilation systems, anesthesia monitor, and cardiovascular systems. Heart and lung sound auscultation can be remotely performed. Airway can be visually examined. The anesthesiologist can then provide consultation and instructions to the remote anesthesia provider on anesthesia management.
Although telemedicine is a technology-ready field of computer applications and has been used in many medicine specialties, at present its usage for systematic anesthesia consultation remains at its infancy. One study reports a case of telemedicine anesthesia between the Amazonian rainforests of Ecuador and Virginia Commonwealth University, via a commercially developed telemedicine system
(6). In another pilot study, the University Health Network in Toronto utilized Northern Ontario Remote Telecommunication Health (NORTH) Network to provide telemedicine
Figure 8. Telemedicine connects remote medical centers for patient care.
clinical consultations to residents of central and northern Ontario in Canada (7).
COMPUTER-AIDED ANESTHESIA CONTROL
The heart of most medical decisions is a clear understanding of the outcome from drug administration or from specific procedures performed on the patient. To achieve a satisfactory decision, one needs to characterize outcomes (outputs), establish causal links between drugs and procedures (inputs) and the outcomes, define classes of decisions in consideration (classes of possible actions and controllers), and design actions (decisions and control). Anesthesia providers perform these cognitive tasks on the basis of their expertise, experience, knowledge of guidelines, and their own subjective judgments. It has long been perceived in the field of anesthesiology that computers may help in this decision and control process.
At a relatively low level of control and decision assistance, there has been routine use by anesthesia providers of computers to supply comprehensive and accurate information about anesthesia drugs, procedures, and guidelines in relation to individual patient care. Thanks to miniaturization and internets, there are now commonly and commercially available digital reference databases on anesthesia drugs, their detailed user manuals, and anesthesia procedures. With a palm-held device, all information becomes readily available to anesthesia providers in operating rooms, and other clinical settings. New data can be routinely downloaded to keep information up-to-date.
More challenging aspects of computer applications are those involving uncertainty, control, and intelligence that are the core of medical decision processes. These include individualized models of human patients, outcome prediction, computer-assisted control, diagnosis, and decision assistance. Such tools need to be further developed and commercialized for anesthesia use.
48 ANESTHESIA, COMPUTERS IN
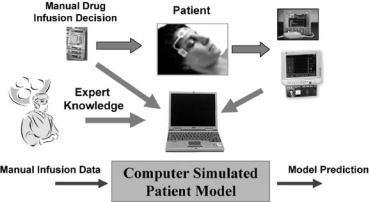
Figure 9. Utility of patient models to predict outcomes of drug infusion.
Patient Modeling and Outcome Prediction
Response of a patient’s physiological and pathological state to drugs and procedures is the key information that an anesthesiologist uses in their management. The response, that is, the outcome, can be represented by either the values of the patient vital signs such as anesthesia depth and blood pressures, or consequence values such as length of ICU stay, hospital stay, complications. Usually, drug impact on patient outcomes is evaluated in clinical trials on a large and representative population and by subsequent statistical analysis. These population-based models (average responses of the selected population) link drug and procedural inputs to their effects on the patient state. These models can then be used to develop anesthesia management guidelines (Fig. 9).
For real-time anesthesia control in operating rooms, the patient model also must represent dynamic aspects of the patient response to drugs and procedures (8). This realtime dynamic outcome prediction requires a higher level of modeling accuracy, and is more challenging than off-line statistical analysis of drug impact. Real-time anesthesia control problems are broadly exemplified by anesthesia drug infusion, fluid resuscitation, pain management, sedation control, automated drug rates for diabetics, and so on.
There have been substantial modeling efforts to capture pharmacokinetic and pharmacodynamic aspects of drug impact as well as their control applications (9). These are mostly physiology-based and compartment-modeling approaches. By modeling each process of infusion pump dynamics, drug propagation, concentration of drugs on various target sites, effect of drug concentration on nerve systems, physiological response to nerve stimulations, and sensor dynamics, an overall patient response model can be established. Verification of such models has been performed by comparing model-predicted responses to measured drug concentration and physiological variables. These models have been used in evaluating drug impact, decision assistance and control designs.
Computer Automation: Anesthesia Control Systems
At present, an anesthesiologist decides on an initial drug control strategy by reviewing the patient’s medical conditions, then adapts the strategy after observing the patient’s actual response to the drug infusion. The strategy is
further tuned under different surgical events, such as incision, operation, and closing. Difficulties in maintaining smooth and accurate anesthesia control can have dire consequences, from increased drug consumption, side effects, shortand long-term impairments, and even death. Real-time and computer-assisted information processing can play a pivotal role in extracting critical information, deriving accurate drug outcome predictions, and assisting anesthesia control.
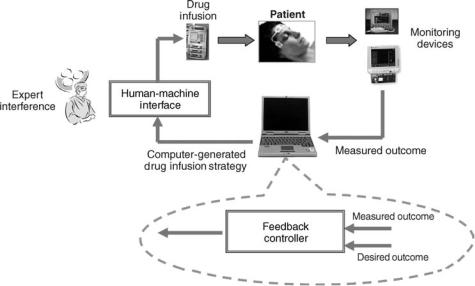
Research efforts to develop computer-assisted anesthesia control systems have been ongoing since the early 1950s (10–14). The recent surge of interest in computer-assisted anesthesia diagnosis, prediction, and controls is partly driven by the advances in anesthesia monitoring technologies, such as depth measurements, computer-program- able infusion pumps, and multisignal real-time data acquisition capabilities. These signals provide fast and more accurate information on the patient state, making computer-aided control a viable possibility. Research findings from computer simulations, animal studies, and limited human trials, have demonstrated that many standard control techniques, such as proportional-integral- derivative (PID) controllers, nonlinear control techniques, fuzzy logic, model predictive control, can potentially provide better performance under routine anesthesia conditions in operating rooms (Fig. 10).
Target Concentration and Effect Control. Target concentration or drug effect control is an open-loop control strategy. It relies on computer models that relate drug infusion rates to drug concentrations on certain target sites or to drug effects on physiological or nerve systems. Since at present drug concentration or drug effects are not directly measured in real-time, feedback control is often not possible. Implementation of this control strategy can be briefly described as follows. For a prespecified time interval, the desired drug concentration profile is defined. This profile is usually determined a priori by expert knowledge, safety mandates, and smooth control requirements. A performance index is then devised that includes terms for control accuracy (to follow the desired profiles closely), drug consumption, constraints on physiological variables (safety constraints), and so on. Then, an optimal control is derived by optimizing the performance index under the given constraints and the dynamic
ANESTHESIA, COMPUTERS IN |
49 |
models of the patient. One common method of designing optimal control strategies is dynamic programming, although many other optimal or suboptimal control design methodologies for nonlinear control systems are also available in the control field. Due to lack of feedback correction in target concentration control, optimality and accuracy of control actions may be compromised. However, even this open-loop control has seen many successful applications, such as glucose level control. Feedback control may become feasible in the future when new sensors become available to measure directly drug concentration.
Automatic Feedback Control. Computer-assisted anesthesia control has been frequently compared to autopilot systems in aviation. The autopilot system controls flying trajectories, altitude and position, airplane stability and smoothness, automatically with minimum human supervision. Success of such systems has resulted in their ubiquitous applications in most airplanes. It was speculated that an anesthesia provider’s routine control tasks during a surgery may be taken over by a computer that adjusts automatically drug infusions to maintain desirable patient states. Potential and speculated advantages of such systems may include less reliance on experience, avoidance of fatigue-related medical mistakes, smoother control outcomes, reduced drug consumptions, and consequently faster recovery. So far, these aspects have been demonstrated only in a few selective cases of research subjects.
System Identification and Adaptive Control for Individualized Control Strategies. One possible remedy for compensating variations in surgical procedures and patient conditions in control design is to use real-time data to adjust patient models that are used in either target concentration control or feedback control. Successful implementation of this idea will generate individualized models that will capture the unique characteristics of the patient. This real-time patient model can then be used to tune
Figure 10. Computer-assisted drug infusion control (a) without expert interference: automated anesthesia feedback control. (b) With expert interference: anesthesia decision assistance systems.
the controllers that will deliver best performance for the patient. This control tuning is the core idea of adaptive control systems: Modifying control strategies on the basis of individually identified patient models. Adaptive control has been successfully applied to a vast array of industrial systems. The main methods of model reference adaptive control, gain scheduling, self-tuning regulators, and machine learning are potentially applicable in anesthesia control. This is especially appealing since variations and uncertainties in patient conditions and surgical events and procedures are far more complicated than industrial systems.
Most control algorithms that have been employed in anesthesia control are standard. The main difficulties in applying automated anesthesia control are not the main control methodologies, but rather an integrated system with high reliability and robustness, and well-designed human-machine interaction and navigation. Unlike an airplane in midair or industrial systems, anesthesia patients vary vastly in their responses to drugs and procedures. Control strategies devised for a patient population may not work well in individual patients. Real-time, onsite, and automatic calibration of control strategies are far more difficult than designing an initial control strategy for a patient population. Adaptation adds a layer of nonlinear feedback over the underlying control, leading to adaptive PID, tuned fuzzy, adaptive neural frameworks, and so on. Stability, accuracy, and robustness of such control structures are more difficult to establish. Furthermore, human interference must be integrated into anesthesia control systems to permit doctors to give guidelines and sometimes take control. Due to high standard in patient safety, at present automated anesthesia control remains largely in a phase of research, and in a very limited sense, toward technology transfer to medical devices. It will require a major commercialization effort and large clinical studies to transform research findings into product development of anesthesia controllers.
Moreover, medical complications occur routinely, which cannot be completely modeled or represented in control
50 ANESTHESIA, COMPUTERS IN
strategies. Since such events usually are not automatically measured, it is strenuous to compensate their impact quickly. In addition, medical liability issues have raised the bar of applying automated systems. These concerns have curtailed a widespread realization of automated anesthesia control systems, despite a history of active research over four decades on anesthesia control systems.
COMPUTER INTELLIGENCE: DIAGNOSIS AND DECISION ASSISTANCE
In parallel to development of automatic anesthesia control systems, a broader application of computers in anesthesia management is computer-aided anesthesia diagnosis, decision assistance, and expert systems. Surveys of anesthesia providers have indicated that the field of anesthesiology favors system features that advise or guide rather than control (15). Direct interventions, closed-loop control, lockout systems, or any other coercive method draw more concerns. In this aspect, it seems that anesthesia expert decision support systems may be an important milestone to achieve before automated systems.
Anesthesia Diagnosis and Decision Assistance
Computer-aided diagnosis will extract useful information from patient data and vital-sign measurements, apply computerized logic and rigorous evaluations of the data, provide diagnosis on probable causes, and suggest guidelinedriven remedy solutions. The outcome of the analysis and diagnosis can be presented to the anesthesia care provider with graphical displays, interactive user interfaces, and audio and visual warnings.
Decision assistance systems provide decision suggestions, rather direct and automatic decision implementations. Such systems provide a menu of possible actions for an event, or dosage suggestions for control purposes, and potential consequences of selected decisions. Diagnosis of possible causes can remind the anesthesiologist what might be overlooked in a crisis situation. The system can have interactive interfaces to allow the physician to discuss further actions and the corresponding outcomes with the computer. This idea of physician-assistant systems aims to provide concise, timely, and accurate references to the anesthesiologist for improved decisions. Since the physician remains as the ultimate decision maker, their management will be enhanced by the available information and diagnosis, but not taken over.
Suggested remedies of undesirable events are essentially recommendations from anesthesia management guidelines, brought out electronically to the anesthesiologist. Some computer simulators for anesthesia education are developed on the basis of this idea. For example, Anesthesia Simulator by Anesoft Corporation (www. anesoft.com) contains a software module of expert consultation that incorporates anesthesia emergency scenarios and suggests expert advices. Utility of expert systems in resident training has been widely accepted. However, decision support systems in the operating rooms are slow in development and acceptance. Generally speaking, a decision support system must interact with the compli-
cated cognitive environment of the operating rooms. To make such systems a useful tool, they must be designed to accommodate the common practice in which the anesthesiologist thinks, sees, and reasons, rather than imposing a complicated new monitoring mode for the clinician to be retrained. This is again an issue of human-factors design.
Dosage recommendations for anesthesia drugs are internally derived from embedded modeling and control strategies. In principle, the control strategies discussed in the previous sections can support the decision assistance system. By including the physician in the decision loop, some issues associated with automated control systems can be alleviated. Reliability of such control strategies, user interfaces, and clinical evidence of cost-effectiveness of the decision support system will be the key steps toward successful clinical applications of such systems.
FUTURE UTILITY OF COMPUTER TECHNOLOGY IN ANESTHESIA
The discussions in the previous sections outline briefly critical roles that computers have played in improving anesthesia management. New development in computerrelated technologies are of much larger potential.
Micro-Electro-Mechanical Systems (MEMS) is a technology that integrates electrical and mechanical elements on a common silicon material. This technology has been used in developing miniature sensors and actuators, such as micro infusion pumps and in vivo sensors. Integrated with computing and communication capabilities, these devices become smart sensors and smart actuators. The MEMS technology has reached its maturity. Further into the realms of fabrication technology at atom levels, emergence of nanotechnology holds even further potential of new generations of medical devices and technologies. There are many exciting possibilities for utility of these technologies in anesthesia: In vitro sensors based on nanodevices can potentially pinpoint drug concentrations at specific target sites, providing more accurate values for automated anesthesia drug control; Microactuators can directly deliver drugs to the target locations promptly and accurately, reducing drastically reliance on trial- and-error and sharpened experience in anesthesia drug infusion control; MEMS and nanosensors together with computer graphical tools will allow two-dimensional (2D) or three-dimensional (3D) visual displays of drug propagation, drug concentration, distributed blood pressures, heart and lung functions, brain functions, consequently assisting anesthesiologists in making better decisions about drug delivery for optimal patient care.
On another frontier of technology advancement, computer parallel computing (many computers working in symphony to solve complicated problems), computer imaging processing, data mining (extracting useful information from large amount of data), machine intelligence, wireless communication technologies, and human-factors science and design provide a vast opportunity and a promising horizon in advancing anesthesia management.
Advanced anesthesia control systems will manage routine drug infusion with their control actions tuned to
