
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index

22 |
R. Guleria and J. Kumar |
|
|
•Supplemental oxygen can be provided through nasal prongs at a flow rate of 1–3 L/min or through a Venturi mask to deliver 24–28% oxygen in hypercapnic failure.
•Nasal prongs are better tolerated but provide less predictable oxygen concentration in comparison to the Venturi mask.
•The aim is to maintain oxygen saturation above 90%, PaO2 more than 60 mmHg, and pH more than 7.35.
Assisted ventilation
•Assisted ventilation, either noninvasive or invasive, is indicated if there is clinical deterioration or if respiratory acidosis persists despite optimum oxygen and medical therapy. Refer to specific Chaps. 3 and 4 for further details.
Step 7: Further management
• Optimum treatment for the underlying etiology must be undertaken simultaneously.
Suggested Reading
1.Epstein SK. Acute respiratory failure. In: Bope ET, Kellerman R, Rakel RE, editors. Conn’s current therapy 2011. 1st ed. Philadelphia: Elsevier Saunders, Section 4; 2011. p. 233–8.
This chapter discusses causes and treatment strategies for acute respiratory failure.
2.Goldman L. Goldman’s Cecil medicine. 24th ed. Philadelphia: Elsevier Saunders, Chapter 104; 2011. p. 629–38.
This chapter discusses the physiology and algorithmic approach for acute respiratory failure.
3.Yeow ME, Santanilla JI. Non-invasive positive pressure ventilation in the emergency department. Emerg Med Clin North Am. 2008; 26:835–47.
4.Lellouche F. Non-invasive ventilation in patients with hypoxemic acute respiratory failure. Curr Opin Crit Care. 2007;13(1):12–9.
This article discusses the role of noninvasive ventilation in management of acute respiratory failure.
5.Baudouin S, Blumenthal S, Cooper B, et al. Role of non-invasive ventilation in management of acute respiratory failure in emergency department. Thorax. 2002;57:192–211.
BTS standards of care committee—noninvasive ventilation in acute respiratory failure.

Noninvasive Positive-Pressure |
3 |
Ventilation |
Rajesh Chawla and Subhash Todi
A 56-year-old male patient, a known case of chronic obstructive pulmonary disease (COPD), presented with acute breathlessness, cough with increase in expectoration, and low-grade fever. On examination, he was found to be in acute respiratory distress, with respiratory rate (RR) of 28/min. He was using his accessory muscles, was slightly drowsy, and breath sounds were diminished on both sides.
Noninvasive positive-pressure ventilation (NIPPV) augments spontaneous ventilation using the tight-fitting nasal or oronasal mask without endotracheal intubation. This can be used in a large number of conditions if there is no contraindication. The application of NIPPV should not delay clinically indicated endotracheal intubation.
Step 1: Initial resuscitation
•The patient should be resuscitated as mentioned in Chap. 78.
•The first step after resuscitation would be to quickly examine the patient in detail.
•Look for hemodynamic instability, sensorium, and oxygenation by pulse oximetry.
•If SpO2 is low, give oxygen—not more than 1–2 L/min. Titrate oxygen to minimum flow to keep SpO2 at 87–92%.
R. Chawla, M.D., F.C.C.M. (*)
Department of Respiratory, Critical Care & Sleep Medicine, Indraprastha Apollo Hospitals, New Delhi, India
e-mail: drchawla@hotmail.com
S. Todi, M.D., M.R.C.P.
Critical Care & Emergency, A.M.R.I. Hospital, Kolkata, India
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
23 |
DOI 10.1007/978-81-322-0535-7_3, © Springer India 2012 |
|
24 |
R. Chawla and S. Todi |
|
|
•Check arterial blood gas (ABG) and initiate other investigations as mentioned below:
–Hemogram, blood urea, serum creatinine, and serum electrolytes
–Blood and sputum culture if infection is suspected
–Chest skiagram
–Electrocardiogram (ECG) and Echocardiogram (Echo)
Disease-specific treatment such as bronchodilators (salbutamol and ipratropium nebulization), antibiotics, corticosteroids should be started.
Step 2: Assess the need of NIPPV
•In addition to the rest of the treatment, NIPPV should be applied simultaneously to a patient in acute respiratory failure (ARF), based on the clinical criteria (Table 3.1), provided there is no contraindication.
•There are no absolute contraindications for the use of NIPPV. Some contraindications have, however, been suggested (Table 3.2).
•NIPPV is indicated in patients with appropriate diagnosis and proven evidence of effectiveness of NIPPV if any two of the clinical criteria are fulfilled (Table 3.1).
Table 3.1 Clinical criteria
Table 3.2 Contraindications
Moderate to severe respiratory distress
Tachypnea (respiratory rate >25/min)
Accessory muscle use or abdominal paradox
Blood gas derangement pH < 7.35, PaCO2 > 45 mmHg
PaO2/FiO2 < 300 or SpO2 < 92% with FiO2 0.5
Nonavailability of trained medical personnel
Inability to protect the airways—comatose patients, patients with cerebrovascular accident or bulbar involvement, confused and agitated patients, upper airway obstruction
Hemodynamic instability—uncontrolled arrhythmia, patients on very high doses of inotropes, recent myocardial infarction
Inability to fix the interface—facial abnormalities, facial burns, facial trauma, facial anomaly
Severe gastrointestinal symptoms—vomiting, obstructed bowel; recent gastrointestinal surgery, upper gastrointestinal bleeding
Life-threatening hypoxemia
Copious secretions
Conditions in which NIPPV has not been found to be effective
NIPPV should only be applied in ARF if there is evidence for its efficacy in that disease state (Table 3.3)
3 Noninvasive Positive-Pressure Ventilation |
25 |
|
|
Table 3.3 Effectiveness for NIPPV in ARF from different causes |
|
Causes of ARF |
Level of evidence |
Acute exacerbation of COPD (AECOPD) |
A |
Weaning (AECOPD) |
A |
Cardiogenic pulmonary edema (CPE) |
A |
Immunocompromised patient |
A |
Postoperative respiratory failure |
B |
Preintubation oxygenation |
B |
Endoscopy |
B |
Asthma exacerbations |
C |
Acute respiratory distress syndrome (ARDS) |
C |
Postextubation respiratory failure |
C |
Do-not-intubate status |
C |
Pneumonia |
C |
A strong, B intermediate, C weak |
|
Step 3: Application of NIPPV
Protocol for application of NIPPV: For successful NIPPV, it is important to fine-tune the patient, interface, and ventilator.
•Patient interface—nasal or oronasal mask.
•Mode of ventilation:
–Bilevel positive airway pressure—spontaneous or spontaneous/timed mode in portable pressure ventilators or NIPPV option on conventional ventilators.
–Pressure support/pressure control/volume control—conventional ventilators. Explain the therapy and its benefit to the patient in detail. Also, discuss the
possibility of intubation.
•Choose the correct size interface. The oronasal mask is preferred in ARF.
•Set the NIPPV portable pressure ventilator in spontaneous or spontaneous/timed mode.
•Start with very low settings, low inspiratory positive airway pressure (IPAP) of
6–8 cm H2O with 2–4 cm H2O of expiratory positive airway pressure (EPAP). The difference between IPAP and EPAP should be at least 4 cm H2O at all times.
•To start with administer oxygen at 2 L/min.
•Hold the mask with the hand over the face. Do not fix it.
•Increase EPAP by 1–2 cm increments until the patient’s inspiratory efforts are able to trigger the ventilator.
•If the patient is making inspiratory effort and the ventilator does not respond, it indicates that the patient has not generated enough respiratory effort to counter auto-PEEP and trigger the ventilator (in COPD patients). Increase EPAP further
until this happens. Most of the patients require EPAP of about 4–6 cm H2O. Patients who are obese or have obstructive sleep apnea require higher EPAP to trigger the ventilator.
•When the patient’s effort is triggering the ventilator, leave EPAP at that level.
26 |
R. Chawla and S. Todi |
|
|
•Now, start increasing IPAP in increments of 1–2 cm up to a maximum pressure, which the patient can tolerate without discomfort and there is no major mouth or air leak.
•In some NIPPV machines, inspiratory time (Ti) can be adjusted. Setting the Ti at 1 s is a reasonable approach.
•Now, secure interface with head straps. Avoid excessive tightness. If the patient has a nasogastric tube, put a seal connector in the dome of the mask to minimize air leakage.
•After titrating the pressure, increase oxygen to bring oxygen saturation to around 90%.
•As the settings may be different in wakefulness and sleep, readjust them accordingly.
When NIPPV is being initiated for ARF, close monitoring and the capability to
initiate endotracheal intubation and other resuscitation measures should be available in the same setup. Start NIPPV preferably in the intensive care unit or in the emergency room in ARF.
Application of NIPPV using a critical care ventilator
•The first step is to select a ventilator, which is capable of fulfilling the needs of the patient.
•Explain the therapy to the patient.
•Choose the appropriate mode. Usually, pressure support or pressure control modes are preferred. Standard critical care ventilators using flow-by system (noninvasive mode option) allow the patient to breathe without expending effort to open valves. In selected patients, such as those suffering from neuromuscular diseases, volume assist or volume control mode may be used.
•Choose an appropriate interface.
•Silent ventilator alarms.
•Keep FiO2 at 0.5.
Using pressure support/control approach
•Start with low settings such as inspiratory pressure support at 5–6 cm H2O and PEEP at 4 cm H2O.
•Initiate NIPPV while holding the mask in place and confirm optimum fit. If it is big or small or loose, change it.
•Hold the mask. Do not fix the headgear.
•Now, increase PEEP until inspiratory efforts are able to trigger the ventilator.
•If the patient is making inspiratory effort and the ventilator does not respond, it indicates that the patient has not generated enough respiratory effort to counter auto-PEEP and trigger the ventilator (in COPD patients). Increase PEEP further until this happens.
•Once the patient’s inspiratory efforts trigger the ventilator, start increasing pressure support further, keeping the patient’s comfort in mind. (Reduced respiratory rate, reduced use of respiratory accessory muscle, etc.) Ensure that there are no major leaks.

3 Noninvasive Positive-Pressure Ventilation |
27 |
|
|
Table 3.4 Monitoring
of NIPPV in ARF
Mask comfort
Tolerance of ventilator settings
Respiratory distress
Respiratory rate
Sensorium
Accessory muscle use
Abdominal paradox
Ventilator parameters
Air leaking
Adequacy of pressure support
Adequacy of PEEP
Tidal volume (5–7 mL/kg)
Patient–ventilator synchrony
Continuous oximetry (until stable)
ABG, baseline and 1–2 h, then as indicated
•When there is significant mouth leak, there may be asynchrony. In that case,
pressure control will be the preferred mode of NIPPV and the Ti can be set to avoid asynchrony.
•Increase fraction of oxygen concentration to maintain oxygen saturation more than 90% at all times.
•Secure interface with the headgear. It should be tight, but not overtight. Small leaks are acceptable.
•A peak inspiratory pressure of more than 25 cm is rarely required in COPD, but higher pressures can be used when using NIPPV for other indications. PEEP is usually titrated between 5 and 10 cm H2O to improve triggering and oxygenation.
Step 4: Patient must be monitored very closely
•The patient must be monitored very closely clinically (Table 3.4). All this must be documented every 15 min for the first hour in the clinical notes.
•The patient will show improvement in parameters if NIPPV is effective.
•ABG sample should be sent after 30 min to 1 h after the application of noninvasive ventilation.
•In ventilator setting, look for air leaks, triggering and patient–ventilator interaction.
Step 5: Continuously look for complications and manage them
•Monitor carefully the worsening respiratory distress, sensorium, tachypnea, and deteriorating blood gases, and intervene early because delay in intubation is a very common major complication of NIPPV.
•Most complications are minor that can be managed very easily, and so every attempt should be made to continue NIPPV.
28 |
R. Chawla and S. Todi |
|
|
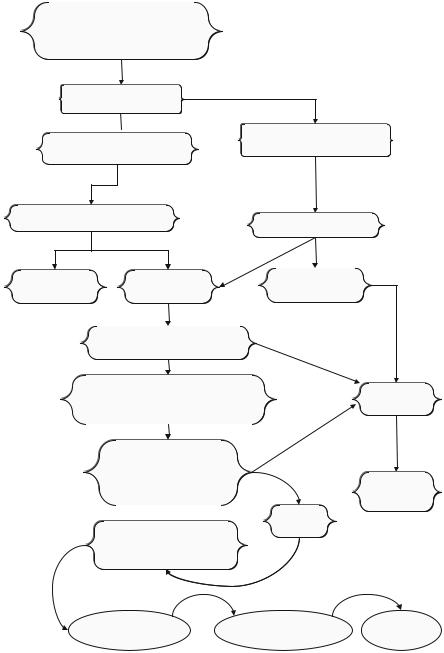
Acute respiratory distress
Tachypnoic RR >25/min
Respiratory failure
PaCO2>45, and/or pH <7.35
Check for underlying
Diseases
 Level of evidence C with for NIPPV Level of evidence A, B for NIPPV Ref.to table3
Level of evidence C with for NIPPV Level of evidence A, B for NIPPV Ref.to table3
Ref.to table3
Need for ventilatory requirement |
|
Assess for use of NIPPV |
||||
|
|
|
||||
No |
Yes |
|
|
|
|
|
Supportive |
Good candidate for |
|
|
Poor candidate for |
|
|
medical therapy |
NIPPV |
|
|
NIPPV |
|
|
Check for contraindications |
|
|
|
|||
|
Table 2 |
|
|
Yes |
|
|
No |
|
|
|
|
||
Start NIPPV with use of appropriate |
|
Intubate |
||||
facemask and oxygen |
|
|
|
|||
Use pressure support or CPAP mode |
|
|
||||
|
|
|
|
No |
|
|
1-2 hour check point |
|
|
|
|
||
• Improve gas exchange |
|
|
Consider NIV |
|||
• |
Patient tolerance |
|
Yes |
|
||
|
|
for extubation |
||||
|
|
|
|
|||
|
|
|
|
|
in selected cases |
|
|
|
|
|
Continue |
|
|
Improvement in respiratory failure |
|
NIV |
|
|||
|
|
|
||||
and primary diseases O2 saturation |
|
|
|
|||
>90% on 6 lit / min O2 FiO2 |
|
|
|
|
||
Start intermittent |
- Patient remains stable |
Discontinue |
||||
discontinuation |
||||||
- No respiratory distress |
NIPPV |
|||||
|
|
|||||
of NIPPV
Fig. 3.1 Application of NIPPV
