
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index
Transfusion Practices and Complications |
61 |
|
|
Nayana Amin and Vijaya Patil |
|
A 54-year-old male patient with carcinoma of the rectum was admitted to the ICU with profuse bleeding per rectum for the previous 12 h. He was hypotensive and tachycardic. His hemoglobin (Hb) was 6.0 g/dL, platelet count was 150 × 103/ mm3, international normalized ratio (INR) was 1.8, and activated partial thromboplastin time (APTT) was 30 s. He was transfused with three units of packed red blood cell.
Blood transfusion is a common practice in the ICU with an estimate of 40% patients having transfusion. It is generally safe but occasionally may lead to minor or lifethreatening consequences if attention to details and protocols is not met during transfusion.
Step 1: Resuscitate
•Secure two large-bore (14G/16G) IV cannulae.
•Send blood for grouping, cross-matching, complete blood count (CBC), coagulation profile, and other appropriate investigations.
•Proper coordination with blood bank is mandatory in these situations for early and proper acquisition of blood products.
Step 2: Transfuse packed RBCs or blood components (Tables 61.1 and 61.2)
•If the patient is bleeding profusely and hemodynamically unstable, use groupspecific uncross-matched blood or O Rh-negative packed cells while waiting for cross-matched blood.
N. Amin, M.D. • V. Patil, M.D. (*)
Department of Anaesthesia, Critical Care and Pain, Tata Memorial Hospital, Mumbai, India
e-mail: vijayappatil@yahoo.com
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
479 |
DOI 10.1007/978-81-322-0535-7_61, © Springer India 2012 |
|
480
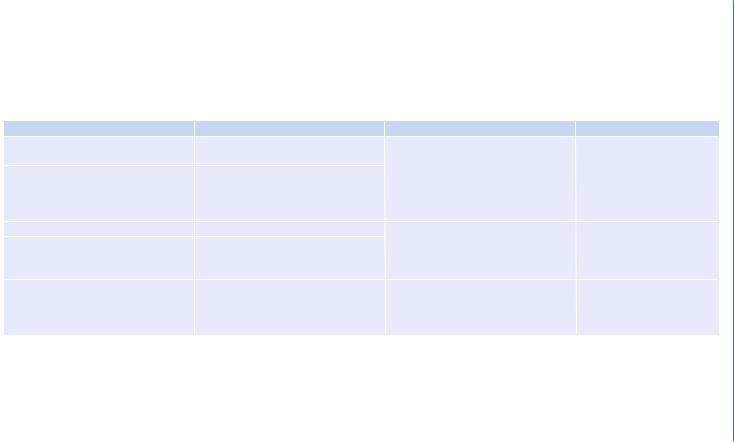
Table 61.1 Alternative red blood cell products |
|
|
|
Technique |
Purpose |
Indications |
Comments |
Leukoreduction |
Minimize the risk of cytomegalovirus |
High-risk immunocompromised |
Does not prevent TA-GVHD |
|
transmission |
patients, patients needing multiple |
(transfusion-associated graft |
Separate type of filters to allow for |
Febrile nonhemolytic transfusion |
transfusions, patients who have had |
vs. host disease) |
RBC and platelet passage only, ideally |
reactions (FNHTR) and |
FNHTR |
|
should be used during collection but |
alloimmunization |
|
|
may be used during transfusion |
|
|
|
Washed RBCs |
Prevent allergic reaction |
Recurrent severe allergic reactions in |
Not equivalent to leukoreduc- |
RBCs washed with saline to remove |
Reduce risk of hyperkalemia |
spite of premedication, IgA-deficient |
tion, 15–20% loss of RBCs |
>98% of plasma proteins, antibodies, |
|
patients, patients at risk of |
|
leukocytes, and electrolytes |
|
hyperkalemia |
|
Gamma irradiation to inactivate |
Prevents TA-GVHD |
Premature infants, patients with |
Does not reduce infectious |
leukocytes |
|
malignancy, recipients of allogenic |
risks or FNHTR |
|
|
hemopoietic transplants, transfusion to |
|
|
|
blood relatives |
|
Patil .V and Amin .N

Table 61.2 Blood components and antifibrinolytics |
|
|
|
||
Product |
Content |
Indications |
Dose |
Caution |
Expected correction |
FFP (fresh frozen |
All coagulation factors |
Deficiencies and |
15 mL/kg |
Should be group specific |
15 mL/kg of FFP will |
plasma) |
in normal concentration |
consumption of |
|
|
increase coagulation |
|
and plasma proteins |
coagulation factors |
|
|
factor concentration by |
|
Thawed plasma may be |
Reversal of factor VI and |
|
Thawed plasma should |
25–30%, which is |
|
stored (1–6°C) up to |
factor V anticoagulants |
|
be transfused within 24 h |
enough for adequate |
|
5 days |
effect (warfarin) |
|
if kept at room |
clotting |
|
|
|
|
temperature |
|
|
|
Massive blood transfu- |
|
Use blood filters |
|
|
|
sion (>1 blood volume |
|
|
|
|
|
within several hours) |
|
|
|
|
|
Replacement in |
|
|
|
|
|
plasmapheresis |
|
|
|
|
|
Raised INR and planned |
|
|
|
|
|
invasive procedure |
|
|
|
|
|
Treatment of thrombotic |
|
|
|
|
|
thrombocytopenic |
|
|
|
|
|
purpura |
|
|
|
|
|
|
|
|
(continued) |
Complications and Practices Transfusion 61
481
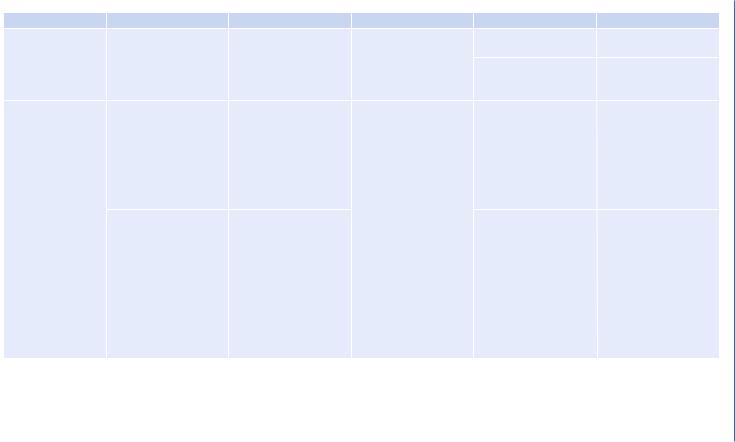
Table 61.2 (continued) |
|
|
|
|
|
Product |
Content |
Indications |
Dose |
Caution |
Expected correction |
Cryoprecipitate |
Fibrinogen, factor VIII/ |
Decreased fibrinogen, |
1 unit/7–10 kg body |
Should be transfused |
1 unit cryoprecipi- |
|
vWF (von Willebrand’s |
liver disease, post- |
weight |
within 6 h of thawing |
tate/10 kg body weight |
|
factor), factor XIII, and |
thrombolysis bleeding |
|
Use blood filters |
Raises plasma fibrinogen |
|
fibronectin |
|
|
|
concentration by |
|
|
|
|
|
~50 mg/dL |
Platelet |
Random donor |
Bleeding due to critically |
Infused over 30–60 min |
Should be group specific |
Expect an adult platelet |
|
platelets—approximately |
decreased circulating |
|
|
count increment of |
|
8.0 × 1010 platelets with |
platelet counts or |
|
|
~7,000–10,000/mm3 for |
|
50 mL plasma |
functionally abnormal |
|
|
each RDP (random |
|
|
platelets |
|
|
donor platelet) given or |
|
|
|
|
|
30,000–60,000/mm3 for |
|
|
|
|
|
each SDP (single donor |
|
|
|
|
|
platelet)given |
|
Single donor plate- |
Maintain platelet count |
|
Do not refrigerate |
In pediatrics, a dose of |
|
lets—3.5–4.0 × 1011 |
>10,000/mm3 in stable |
|
|
5–10 mL/kg of platelets |
|
platelets with 250 mL |
nonbleeding patients, |
|
|
(RDP or SDP) should |
|
plasma |
>30,000/mm3 in unstable |
|
|
result in 50–100,000/ |
|
|
nonbleeding patients, |
|
|
mm3 increment |
|
|
and >50,000/mm3 in |
|
|
|
|
|
patients undergoing |
|
|
|
|
|
invasive procedures or |
|
|
|
|
|
actively bleeding |
|
|
|
|
|
>100,000/mm3 or for |
|
|
|
|
|
CNS trauma |
|
|
|
482
Patil .V and Amin .N
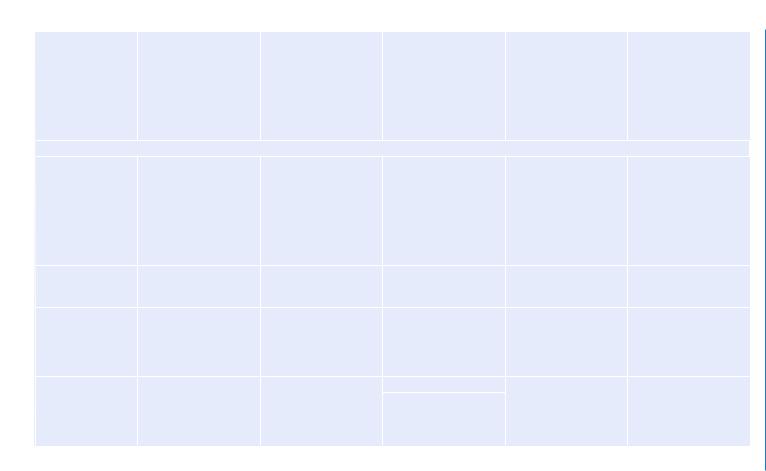
Product |
Content |
Indications |
Dose |
Caution |
Expected correction |
Desmopressin |
Stimulate the endothelial |
Hemophilia A, von |
0.3mcg/kg repeated as |
|
Tachyphylaxis may |
|
release of factor VIII and |
Willebrand’s disease, |
clinically necessary at |
|
occur after three or four |
|
vWF into the plasma |
uremic thrombocytopathy |
intervals of 12–24 h |
|
doses |
|
(V2 receptor-mediated |
|
|
|
|
|
effect), where they form |
|
|
|
|
|
a complex with platelets |
|
|
|
|
|
and enhance their ability |
|
|
|
|
|
to aggregate |
|
|
|
|
Antifibrinolytic drugs |
|
|
|
|
|
Epsilon- |
Competitive inhibitor of |
Situations associated |
100 mg/kg as an IV |
|
|
aminocaproic acid |
plasminogen activation |
with hyperfibrinolysis |
bolus followed by an |
|
|
|
|
such as operations |
infusion of 15 mg/kg/h |
|
|
|
|
requiring cardiopulmo- |
(max 24 gm/day) |
|
|
|
|
nary bypass, liver |
|
|
|
|
|
transplantation, and |
|
|
|
|
|
some urological and |
|
|
|
|
|
orthopedic operations |
|
|
|
Tranexamic acid |
Competitive inhibitor of |
|
Bolus dose of 10–15 mg/ |
|
|
|
plasminogen activation |
|
kg IV followed by 1 mg/ |
|
|
|
|
|
kg/h for 5–8 h |
|
|
Aprotinin |
Powerful inhibitor of |
Cardiac surgery, major |
Loading dose of 2 |
|
|
|
plasmin, trypsin, |
orthopedic surgeries, |
million international unit |
|
|
|
chymotrypsin, kallikrein, |
liver transplant |
followed by continuous |
|
|
|
thrombin, and activated |
|
infusion of 500,000 |
|
|
|
protein C |
|
KIU/h |
|
|
Activated factor VIIa |
|
Factor VIIa deficiency, |
30 up to 90 mcg/kg |
|
Target trough activity of |
|
|
retropubic prostatec- |
Repeat every 2–3 h till |
|
at least 10–15 IU% |
|
|
tomy, bleeding in |
satisfactory hemostasis |
|
(10–15%) is needed |
|
|
trauma, orthotopic liver |
is achieved |
|
|
|
|
transplantation |
|
|
|
Complications and Practices Transfusion 61
483
484 |
N. Amin and V. Patil |
|
|
•In the presence of active bleeding, transfuse blood rapidly over 30 min (if available, use the rapid infusion pump, which can give fluids at a faster rate).
•4 mL/Kg of packed RBCs (usually one unit) increases the hemoglobin by 1 g/dL and hematocrit by 3% in absence of active bleeding.
•Blood should be transfused within 4 h except in emergency. Rate of transfusion can be adjusted as per need, that is, rapidly in hypovolemic patients and slowly in stable patients; however, once issued from blood bank, blood transfusion should get over within 4 h to prevent growth of organisms. If blood cannot be transfused fully within this time, it is advisable to discard it.
•Transfuse blood and blood products through the filter adequate to prevent passage of small clots that may form in stored blood.
•The filter with a pore size of 170–200 mm is recommended for routine transfusions of RBCs, platelets, fresh frozen plasma (FFP), and cryoprecipitate.
•Filters with smaller pore size are more efficient, but they would increase resistance and filter out platelet aggregates, reducing efficiency of transfused platelets.
•Microaggregate filters with 20–40 mm size are recommended during cardiopulmonary bypass only.
•Filters can slow down the rate of blood transfusion. So the standard recommendation is to use a new set for every transfusion. In case of rapid transfusion if filter does not look clogged, change the set every two transfusions.
•Use fluid warmer to transfuse blood in massive blood loss. This helps to prevent hypothermia, which can contribute to the coagulopathy by causing reversible platelet dysfunction, altering coagulation kinetics, and enhancing fibrinolysis.
•Hypothermia also causes ventricular dysrhythmias and citrate toxicity due to reduced citrate metabolism.
•Do not use unconventional and uncontrolled methods such as keeping near heat source or immersing the bag in hot water bath.
Step 3: Correct coagulopathy (see Chap. 62)
•Correct high INR with FFP or low platelets with platelet transfusions only in an actively bleeding patient.
•Do not correct raised INR prophylactically in a nonbleeding patient unless a surgical intervention is contemplated.
•Other coagulopathic abnormalities need to be corrected.
•Antifibrinolytic agents may be used to minimize bleeding in situation like trauma.
•Correct hypothermia.
•Normalize calcium.
•Consider activated factor VII in some specific situations.
Step 4: Control the source of bleeding
•Investigate to find out the source of bleeding and consider options available for controlling the bleeding (interventional radiology or surgery).
•Urgent consultation is required if needed with these specialities.
61 Transfusion Practices and Complications |
485 |
|
|
Step 5: Assess the severity of bleeding
•Massive blood loss may be defined as:
–Loss of one blood volume within a 24-h period
–Loss of blood equivalent to 7% of in lean body weight in an adult (5 L) and 8–9% in a child
–Loss of 50% of blood volume within 3 h
–Loss of blood at a rate in excess of 150 mL/min
Step 6: Manage massive blood loss
•Institute continuous invasive pressure monitoring for fluid management if the patient continues to remain hypotensive due to ongoing bleeding.
•Serial CBC (Hb and platelets) and coagulation tests (prothrombin time, APTT, and fibrinogen), blood gas analysis, serum electrolytes (Na, K, Mg, ionized calcium), and serum lactate should be done.
•These should be repeated frequently in ongoing bleeding and after every component therapy.
•Transfusion of platelets, FFPs, and cryoprecipitate should be guided by laboratory results.
•FFP administration should begin after loss of one blood volume and platelets after loss of 1.5 times the blood volume.
•1:1:2 ratio should be maintained for packed RBCs, FFP, and random donor platelets to prevent dilutional coagulopathy and dilutional thrombocytopenia due to massive blood transfusion, which results in a vicious cycle of bleeding diathesis.
•Administer cryoprecipitate if fibrinogen is less than 100 mg/dL or there is a fear of volume overload by use of FFP.
•If patients with A or B blood group have received multiple units of O Rh-positive whole blood, then they can be switched back to their inherent group-specific blood only after subsequent testing by the blood bank indicates it is safe to do so.
Step 7: Identify and manage transfusion-induced complications (Table 61.3)
•Stop blood transfusion immediately if any acute hemolytic transfusion reaction is suspected.
•Hypotension may be due to acute ongoing hemorrhage, acute severe transfusion reaction, allergic reaction/anaphylaxis, or rarely due to septic shock (due to transfusion of blood with bacterial contamination).
•Check the identity of the recipient with the details on the bag and the cross-match form.
•Transfusion-associated circulatory overload (TACO) is circulatory overload following transfusion of blood or blood product.
•Transfusion-associated acute lung injury (TRALI) is defined as new acute lung injury (with hypoxemia and bilateral infiltrates on chest radiograph but no evidence of left atrial hypertension) occurring during or within 6 h after a transfusion, with a clear temporal relationship to the transfusion, and not explained by another acute lung injury (ALI) risk factor.

Table 61.3 Transfusion-related complications |
|
|
|
Reaction |
Cause |
Clinical signs |
Treatment |
Febrile nonhemolytic transfusion |
Reaction between the recipient’s |
Fever, temperature rise |
Give paracetamol and resume |
reaction (FNHTR) |
antibodies and transfused leukocytes |
|
transfusion at a slow rate |
|
Pyrogenic cytokines released from the |
|
|
|
leukocytes in stored blood |
|
|
Allergic reaction |
Reaction to soluble allergens in the |
Urticaria, flushing, pruritus |
Give 10 mg IV chlorpheniramine |
|
donor’s plasma |
|
maleate and resume transfusion |
Anaphylaxis |
IgA-deficient individuals react to IgA |
Flushing, pruritus, laryngospasm, |
Stop transfusion |
|
in transfused units |
bronchospasm |
Supplement O2 |
|
|
|
SC/IV epinephrine, 100 mg IV |
|
|
|
hydrocortisone, 10 mg IV |
|
|
|
chlorpheniramine maleate |
|
|
|
Salbutamol nebulization |
|
|
|
IV fluids |
|
|
|
Send the blood back to the blood |
|
|
|
bank along with a sample of the |
|
|
|
patient’s blood |
|
|
|
Use washed RBCs in future |
Sepsis |
Bacterial contamination of blood and |
Fever, chills, hypotension |
Stop transfusion |
|
blood products, Yersinia, bacteria, |
|
Contact the blood bank and send |
|
malaria |
|
the remaining blood to the blood |
|
|
|
bank |
Acute hemolytic transfusion reaction |
Immune-mediated—due to cytokines |
Fever, chills, flushing, chest pain, |
Send blood for CBC, coagulation |
(<24 h) |
in transfused blood |
back pain, vomiting, tachycardia, |
profile, direct Coombs’ test, lactate |
|
|
hypotension |
dehydrogenase, haptoglobin, liver |
Delayed hemolytic transfusion |
Nonimmune-mediated—transfusion |
|
function tests for indirect |
reaction (24 h to 28 days) |
of damaged red cells |
|
bilirubinemia, peripheral smear for |
|
|
|
evidence of hemolysis |
|
|
|
Gram staining and blood culture if |
|
|
|
bacterial contamination is |
|
|
|
suspected |
486
Patil .V and Amin .N

Reaction |
Cause |
Clinical signs |
Treatment |
|
|
|
Send urine for hemoglobinuria O2 |
|
|
|
supplementation, fluid resuscita- |
|
|
|
tion, and vasopressors to maintain |
|
|
|
mean arterial pressure >65 mmHg |
|
|
|
Broad-spectrum antibiotics if |
|
|
|
sepsis is suspected |
ABO (major blood group) |
Mismatched transfusion, IgM |
Fever, chills, flushing, chest pain or |
Stop transfusion |
incompatibility |
antibody against major RBC antigen, |
low back pain, hypotension, and |
Reconfirm the patient’s identity |
|
leading to intravascular hemolysis, |
dyspnea |
and blood group |
|
renal failure, disseminated intravascu- |
|
Inform the blood bank and return |
|
lar coagulation (DIC) |
|
|
|
|
blood to the blood bank |
|
|
|
|
|
|
|
|
Infuse saline to maintain urine |
|
|
|
output of 100 mL/h |
|
|
|
Give diuretics if urine output falls |
|
|
|
Treat DIC with appropriate blood |
|
|
|
components |
Transfusion-associated graft-versus- |
Donor lymphocytes initiate an |
Fever, skin rash, liver dysfunction, |
No treatment |
host disease (TA-GVHD) 2–30 days |
immune attack against recipient’s |
diarrhea, severe pancytopenia |
Prevention by using gamma-irradi- |
after transfusion |
cells |
|
ated blood products in high-risk |
|
|
|
patients |
|
Cause |
Presentation |
Treatment |
TACO |
Volume overload |
Dyspnea, rales, hypertension, and |
O2 supplementation, diuretics, |
|
|
desaturation, raised central venous |
ventilatory support |
|
|
pressure (CVP) |
|
TRALI |
Antibodies in the donor’s blood react |
Dyspnea, rales, hypotension, and |
Supportive management |
|
with neutrophil antigen in the |
desaturation, normal or low CVP |
Ventilate according to acute |
|
recipient |
|
respiratory distress syndrome |
|
|
|
network protocol |
|
|
|
Steroids not indicated |
Complications and Practices Transfusion 61
487
