
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index

48 |
F.N. Kapadia and U. Bhutada |
|
|
¥Use only when paralytic agents are discontinued.
¥Response is seen within 5 days. If there is no response, it may be discontinued.
¥If favorable response, continue for 14 days or until extubation, thereafter half dose for 7 days followed by one-fourth dose for another 7 days, and then stop.
¥The safety proÞle is proven including no added risk of infection.
Step 10: Administer fluids conservatively
¥Monitoring ßuid status with the central line is required. Pulmonary artery catheter is not recommended.
¥Conservative ßuid management strategy should be adopted but not at the risk of organ perfusion.
¥Hemodynamics is maintained with ßuids, vasopressors, and dobutamine for low cardiac index.
Step 11: Consider immunonutrition
Present guidelines recommend to initiate enteral immunonutrition with formulation containing antiinßammatory lipid proÞle, that is, eicosapentenoic acid, gamalinoleic acid (GLA) (omega-3 Þsh oil, borage oil), and antioxidants. There has been a recent study casting doubt on enteral immune nutrition.
Step 12: Decide on need for tracheostomy
¥Tracheostomy should be performed once the patient is off high FiO2 and PEEP support but still needs continuing ventilator support due to high minute ventilation. (See Chap. 96 on Percutaneous Tracheostomy)
Step 13: Consider weaning (see Chap. 7)
¥Weaning attempts should be started once FiO2 and PEEP support decrease and minute ventilation requirement comes down.
Step 14: Initiate aggressive mobilization regimen
In order to prevent long-term neuromuscular disability, early aggressive physiotherapy should be started from the initial days.
Suggested Reading
1.The ARDS DeÞnition Task Force. Acute Respiratory Distress Syndrome The Berlin DeÞnition. JAMA. 2012;():1Ð8. doi:10.1001/jama.2012.5669.
The Berlin definition of ARDS has classified ARDS into Mild, Moderate AND Severe ARDS. The updated and revised Berlin Definition addresses a number of limitations of previous definition.
2.Sud S, Friedrich JO, Taccone P, Polli F, Adhikari NK, Latini R, Pesenti A. Prone ventilation reduces mortality in patients with acute respiratory failure and severe hypoxemia: systematic review and meta-analysis. Intensive Care Med. 2010;36(4):585Ð99.
Post hoc analysis demonstrated prone position improved statistically significant mortality in the more hypoxemic subgroup and significant differences were seen between subgroups using a range of PaO2/FiO2 thresholds up to approximately 140 mmHg.

5 Mechanical Ventilation in Acute Respiratory Distress Syndrome |
49 |
|
|
3.Meduri GU, Golden E, Freire AX, Taylor E, Zaman M, Carson SJ, Gibson M, Umberger R. Methylprednisolone infusion in early severe ARDS results of a randomized controlled trial. Chest. 2009;136(5 Suppl):E30.
This study shows that steroid results in reduction in the duration of mechanical ventilation, ICU stay and ICU mortality.
4.National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network, Wiedemann HP, Wheeler AP, Bernard GR, Thompson BT, Hayden D, deBoisblanc B, Connors AF Jr, Hite RD, Harabin AL. Comparison of two ßuid-management strategies in acute lung injury. N Engl J Med. 2006;354(24):2564Ð75.
The conservative strategy group shows improvement in the oxygenation and the lung injury score and increased number of ventilator-free days (P < 0.001).
5.National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network, Wheeler AP, Bernard GR, Thompson BT, Schoenfeld D, Wiedemann HP, deBoisblanc B, Connors AF Jr, Hite RD, Harabin AL. Pulmonary-artery versus central venous catheter to guide treatment of acute lung injury. N Engl J Med. 2006;354(21):2213Ð24.
PAC-guided therapy does not improve survival or organ function but is associated with more complications than CVC-guided therapy.
6.Steinberg KP, Hudson LD, Goodman RB, Hough CL, Lanken PN, Hyzy R, Thompson BT, Ancukiewicz M, National Heart, Lung, and Blood Institute Acute Respiratory Distress Syndrome (ARDS) Clinical Trials Network. EfÞcacy and safety of corticosteroids for persistent acute respiratory distress syndrome. N Engl J Med. 2006;354(16):1671Ð84.
These results do not support the routine use of methylprednisolone for persistent ARDS despite the improvement in cardiopulmonary physiology. This study also showed that starting methylprednisolone therapy more than 2 weeks after the onset of ARDS may increase the risk of death.
7.Brower RG, Lanken PN, MacIntyre N, Matthay MA, Morris A, Ancukiewicz M, Schoenfeld D, Thompson BT, National Heart, Lung, and Blood Institute ARDS Clinical Trials Network. Higher versus lower positive end-expiratory pressures in patients with the acute respiratory distress syndrome. N Engl J Med. 2004;351(4):327Ð36.
Clinical outcomes are similar whether lower or higher peep levels are used, with a tidal volume goal of 6 mL/kg of predicted body weight and an end-inspiratory plateau-pressure limit of 30 cm H2O.
8.The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301Ð08.
Mortality is lower in the group treated with lower tidal volumes than in the group treated with traditional tidal volumes (31.0% vs. 39.8%, P = 0.007).
Websites
1.http://www.ardsnet.org
The ofÞcial website of the ARDS Network, initiated by National Heart, Lung, and Blood Institute and National Institutes of Heath to carry out multicenter clinical trials of ARDS treatments.

Mechanical Ventilation in Obstructive |
6 |
Airway Diseases |
Raj Kumar Mani
A 23-year-old female patient, known to be asthmatic since childhood and on regular inhalers, developed breathlessness at work. Several puffs of salbutamol failed to relieve the symptoms, and she rapidly went on to have wheezing and restlessness followed by air hunger. She was brought to the emergency department.
Obstructive pulmonary diseases are a major cause of mortality and morbidity. Acute respiratory failure in chronic obstructive pulmonary disease (COPD) is one of the common reasons for admission to the intensive care unit (ICU). Use of noninvasive ventilation has revolutionized the treatment and outcome of COPD patients.
Step 1: Initiate resuscitation
•The patient should be resuscitated as mentioned in Chap. 78.
•All the patients admitted with respiratory distress require immediate attention to the airway. This assessment is done mainly by clinical means.
They should be put on oxygen flow to increase SpO2 to more than 90%. For
chronic obstructive pulmonary disease (COPD) patient, use controlled inhaled oxygen through the venturi mask to keep SpO2 88–90%. Patients who have increased work of breathing and seem to be getting exhausted may require assisted ventilation.
Step2: Assess severity
It is done based on the following:
•Able to speak full sentences.
•Restlessness.
R.K. Mani, M.D., F.R.C.P. (*)
Department of Pulmonology and Critical Care, Artemis Health Institute, Gurgaon, India e-mail: rkmjs@vsnl.net
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
51 |
DOI 10.1007/978-81-322-0535-7_6, © Springer India 2012 |
|
52 |
R.K. Mani |
|
|
•Respiratory rate and pattern of respiration.
•Use of accessory muscles.
•Pulse rate and pulsus paradoxus (inspiratory decrease in systolic blood pressure by > 10 mmHg).
•Sensorium, fatigue.
•Auscultation: Wheezes and crackles; silent chest signifies very severe airflow obstruction.
•Peak expiratory flow rate is an objective measure of airflow obstruction: less than 30% of baseline/predicted would indicate likelihood of respiratory failure. Initially, check every 30 min to assess response to the therapy.
•SpO2: Hypoxia is usually correctable with supplemental oxygen. Refractory hypoxia should trigger search for pneumothorax, atelectasis, pneumonia, or occult sepsis.
•Arterial blood gases: In asthma, normal or elevated PaCO2 signifies respiratory failure due to respiratory muscle fatigue. pH of less than 7.28 would indicate the need for ventilatory support. Hyperlactatemia may occur due to muscle fatigue or adrenergic agents.
Step 3: In the absence of imminent respiratory or circulatory failure, start immediate medical management of asthma
•Nebulized salbutamol 2.5 mg (0.5 mL of 5% solution in 2.5 mL saline) or levosalbutamol should be repeated every 20 min for three doses and then less frequently, dictated by the patient’s clinical response. More frequent and even continuous nebulization of salbutamol at a dosage of 10–15 mg can be used in acute bronchial asthma within limits of toxic effects such as tachycardia and tremors.
•Nebulized ipratropium (0.5 mg every 20 min) should be included in initial treatment concomitantly with salbutamol for better bronchodilatation.
•If the nebulizer is not available, use four puffs of salbutamol meter dose inhalers (MDI) through a spacer device.
•Corticosteroids should be initiated at the earliest to prevent respiratory failure. The usual doses are as follows: Hydrocortisone injection 100 mg every 6 h or methylprednisolone 60–125 mg every 6–8 h. Oral prednisolone 60 mg is equally effective especially in COPD.
•Oxygen supplementation is continued to keep SpO2 more than 90%.
•Methylxanthines: Aminophylline may be used as a second-line agent, although its role is much debated. A loading dose of 5–6 mg/kg is followed by a continuous infusion of 0.6 mg/kg/h. Avoid loading dose in case the patient has been on oral theophyllines earlier.
•Magnesium sulfate (2 g infusion) over 20 min can also be tried in refractory cases of asthma, although its role is unproven.
•Antibiotics are not required routinely in bronchial asthma exacerbation and should be given only if there is evidence of infection.
•Quinolones or macrolides may be used for COPD exacerbation and should be given only if there is evidence of infection, although most of these are viral in origin.
6 Mechanical Ventilation in Obstructive Airway Diseases |
53 |
|
|
Step 4: Assess need for respiratory support
•Noninvasive ventilation (NIV): For a fatiguing patient, struggling to breathe in spite of medical treatment, NIV may be tried. Inspiratory positive airway pressure reduces work of breathing and expiratory positive airway pressure overcomes auto-positive end-expiratory pressure (auto-PEEP). Extended trials of NIV may be warranted if the sensorium and patient comfort are improving (see Chap. 3).
•Noninvasive positive pressure ventilation is more useful in patients with COPD; there are limited data on its use in acute severe asthma.
•Continuously monitor the heart rate, respiratory rate, SpO2, blood pressure, and sensorium. Reassess every 30 min until the patient is stable and comfortable. Nursing attendance should be continuous.
Step 5: Assess the need for intubation and mechanical ventilation (MV)
•Impending respiratory arrest.
•Circulatory failure.
•Altered sensorium: progressive drowsiness, agitation, or severe restlessness.
•In a conscious patient, no improvement or deterioration after 3–4 h of optimal medical therapy and NIV support.
•In asthma, PCO2 of more than 55 mmHg and pH less than 7.28.
•In COPD, more severe hypercarbia and acidosis are well tolerated. However, the general appearance and the degree of distress and fatigue of the patient are more important than the absolute values. NIV is initially used in these patients. MV is used only if there are contraindications or failure of NIV.
Step 6: Initiate MV
Principles: Because of severe airway obstruction, dynamic hyperinflation or air trapping takes place. Progressive inflation leads to equilibrium of inflow and outflow of air in the lungs to take place at a high resting lung volume. MV aimed at normalizing blood gas values would further overdistend the lungs with its attendant barotrauma and circulatory consequences.
•Orotracheal intubation: Follow the steps of rapid sequence intubation. As far as possible, a tube size of 8 or more is used, and therefore orotracheal route is preferred.
•Sedation and paralysis: At the time of intubation, short-acting sedatives (midazolam) and short-acting neuromuscular blocking agents (succinylcholine) are used. For maintenance of sedation to assist MV, midazolam/propofol infusion can be used. Neuromuscular blocking agents should be avoided as infusion to prevent critical illness neuropathy.
•Avoid delivering high rate and tidal volume with bag ventilation.
•Initial ventilator settings: Controlled mechanical ventilation (CMV) mode; tidal volume 8–10 mL/kg or less; respiratory rate 10–15 breaths/min; minute ventila-
tion 6–8 L/min or less; peak flow rate 100 L/min or more; FiO2 of 1.0, I:E ratio at least 1:3; PEEP should be set to zero to avoid overinflation in control ventilation (Table 6.1).
54 |
R.K. Mani |
|
|
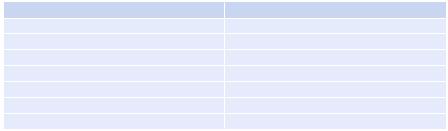
Table 6.1 Initial ventilator settings in status asthmaticus and COPD |
|
Setting |
Recommendation |
Respiratory rate |
10–15 breaths/min |
Tidal volume |
8–10 mL/kg |
Minute ventilation |
6–8 L/min |
PEEP |
0 cm H2O |
Inspiratory flow |
³100 L/min |
I:E ratio |
³1:3 |
FiO2 |
1.00 |
•When the patient is on assist control mode of ventilation, PEEP may be titrated cautiously to counteract auto-PEEP for easier triggering.
Aerosolized bronchodilator therapy should be used properly during MV as mentioned below:
•Always do proper suctioning before starting nebulization.
•Heat and moisture exchangers, if used, should be removed.
•Water in circuit reduces delivery of aerolized bronchodilators, and therefore remove this before starting bronchodilators.
•Change alarm limits and other settings on the ventilator to suit the use of nebulizers, and do not forget to reset them back to the original settings after nebulization is over.
•Nebulizers and pressurized meter dose inhalers (PMDIs) are equally effective.
•Higher dose of bronchodilators is required in MV than in ambulatory patients.
•PMDIs should be used with adaptors and synchronized with inspiration of the ventilatory cycle.
•The nebulizer should be attached in inspiratory line of the ventilator 46 cm away from the Y-piece.
•Nebulizer gas flow should be kept at 6–8 L/min.
•The ultrasonic nebulizer can also be used to give nebulizer therapy.
Monitor:
•Pplat (plateau pressure) reflects intrinsic PEEP (PEEPi) or dynamic hyperinflation and should be kept at less than 30 cm H2O.
•Peak airway pressure reflects only proximal airway pressure and is generally high.
•Avoid overventilation. The risk of barotrauma generally correlates with endexpiratory lung volume, not with the pressure. Hypotension is usual after MV due to dynamic hyperinflation, intrinsic PEEP, dehydration, and use of sedatives. It should be managed by giving fluid challenge.
Step 7: Liberation from MV (see Chap. 7)
Once the airway resistance decreases as reflected by improvement in Pplat and hypercarbia, larger minute ventilation becomes possible without increase in dynamic hyperinflation (DHI).
