
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index
Pericardiocentesis |
99 |
|
|
Rajesh Chawla, Sananta K. Dash, and Vipul Roy |
|
A 60-year-old patient—a case of non-Hodgkin’s lymphoma—presented in the emergency department with acute breathlessness. His pulse was 80/min, and blood pressure was 80/60 mmHg. Neck veins were prominent and heart sounds were feeble. ECG showed low voltage and echocardiogram showed massive pericardial effusion. A pericardiocentesis was planned.
The removal of fluid from the pericardial space is called pericardiocentesis. The abrupt collection of fluid raises intrapericardial pressure, compresses the heart, and decreases cardiac output. This condition is called cardiac tamponade. Echocardiography is recommended to make urgent diagnosis and look for diastolic collapse of the right atrium and ventricle due to cardiac tamponade. Immediate aspiration of fluid is recommended in such a case.
Step 1: Assess the patient
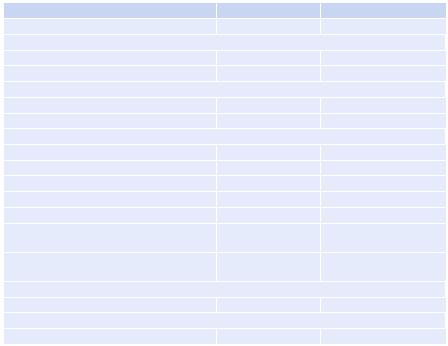
Assessment of a patient of excessive pericardial fluid is done clinically based on the clinical signs, ECG, and echocardiography (Table 99.1).
R. Chawla, M.D., F.C.C.M. (*)
Department of Respiratory, Critical Care & Sleep Medicine, Indraprastha Apollo Hospitals, New Delhi, India
e-mail: drchawla@hotmail.com
S.K. Dash, M.D.
Department of Respiratory & Critical Care Medicine, Indraprastha Apollo Hospitals, New Delhi, India
V. Roy, M.D., D.M.
Department of Cardiology, Indraprastha Apollo Hospitals, New Delhi, India
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
797 |
DOI 10.1007/978-81-322-0535-7_99, © Springer India 2012 |
|
798 |
|
R. Chawla et al. |
|
||
Table 99.1 Differentiating cardiac tamponade and constrictive pericarditis |
||
Clinical signs |
Tamponade |
Constrictive pericarditis |
Pulsus paradoxus |
Common |
Usually absent |
Jugular veins |
|
|
Prominent y descent |
Absent |
Usually present |
Prominent x descent |
Present |
Usually present |
Electrocardiogram |
|
|
Low ECG voltage |
May be present |
May be present |
Electrical alternans |
May be present |
Absent |
Echocardiography |
|
|
Thickened pericardium |
Absent |
Present |
Pericardial calcification |
Absent |
Often present |
Pericardial effusion |
Present |
Absent |
Right ventricle size |
Usually small |
Usually normal |
Myocardial thickness |
Normal |
Normal |
Right atrial collapse and right ventricular |
Present |
Absent |
diastolic collapse |
|
|
Exaggerated respiratory variation in flow |
Present |
Present |
velocity |
|
|
CT/MRI |
|
|
Thickened/calcific pericardium |
Absent |
Present |
Cardiac catheterization |
|
|
Equalization of diastolic pressures |
Usually present |
Usually present |
Step 2: Assess the need of needle pericardiocentesis and contraindications
A.Indications Emergency
I. Evidence of cardiac tamponade:
(a)Hypotension (refractory to fluid resuscitation and vasopressors)
(b)Distended neck veins with cyanosis
(c)Central venous pressure more than 20 mmHg
(d)Narrowed pulse pressure
(e)No other explanation of hypotension (e.g., pneumothorax)
II. Penetrating injury to the chest between the nipples
Elective
Purely diagnostic pericardiocentesis should be limited to selective cases:
I. Cytologic evaluation (discriminate a bacterial, traumatic, neoplastic, or idiopathic cause)
II. Removal of chronic pericardial effusion, which may also produce immediate clinical improvement
III. Placement of a catheter for repeated pericardial drainage and lavage IV. Instillation of antimicrobial agents into the pericardial space
V. Suspicion of purulent pericarditis
99 Pericardiocentesis |
799 |
|
|
B.Contraindications
(i)Septic pleuritis (may introduce infection into pericardial space).
(ii)External wounds overlying the site of centesis (The approach for the procedure can be from either side of thorax.)
(iii)Thrombocytopenia (<50,000/mm3), bleeding disorders, and anticoagulant therapy (for elective pericardiocentesis).
Step 3: Know the options
1. Needle pericardiocentesis: It is decompression of pericardial tamponade by needle aspiration of blood or fluid from the pericardial space.
2. Intrapericardial catheterization: This is a nonsurgical, usually done in a catheterization laboratory under fluoroscopic or echocardiography guidance using dilatational technique.
Step 4: Procedure
•Aggressive resuscitation measures should continue along with preparation for emergency pericardiocentesis.
•Vasopressor and inotropic support should be considered in fluid unresponsive shock.
•The required preprocedure investigations include complete hemogram, prothrombin time, activated partial thromboplastin time, renal functions tests (RFT), and liver functions tests (LFT).
•Blind pericardiocentesis is no longer recommended. Echocardiography-guided procedure is safe and desirable (Table 99.2)
A. Percutaneous blind technique
1.Take written informed consent.
2.Patient preparation: Monitor vital signs and attach cardiac monitor. Keep the head of the bed elevated to approximately 45°. The patient should be placed at a comfortable height for the physician. A central venous catheter is essential for monitoring of right heart pressure and rapid infusion of saline and drugs. Invasive arterial pressure monitoring is indicated. Oxygen supplementation is essential:
•Localizing the entry site: Locate the patient’s xiphoid process and the border of the left costal margin using inspection and careful palpation. The needle entry site should be 0.5 cm to the (patient’s) left of the xiphoid process and 0.5–1.0 cm inferior to the costal margin.
•Skin preparation: Strict asepsis is required with povidone iodine preparation. Local anesthesia is required (lidocaine 2%) prior to the puncture.
•Puncture: Puncture at a 45° angle to the skin with the needle toward the inferior tip of the left scapula.
•Advancement: Advance the needle posteriorly (while initially pressing the liver hard with the other hand to avoid a tear of the liver) with intermittent aspiration and injection of lidocaine through the path. Pass the tip beyond the posterior border of the bony thorax (usually lies within
800 |
R. Chawla et al. |
|
|
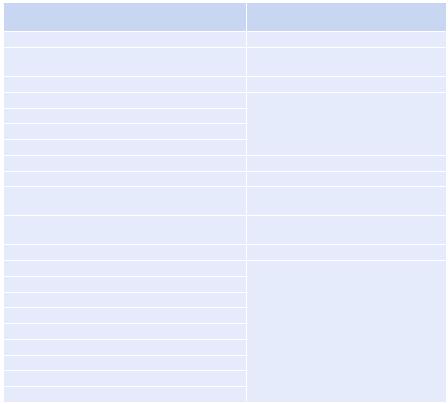
Table 99.2 Equipment for pericardiocentesis |
|
|
Equipments for intrapericardial |
Equipments for needle pericardiocentesis |
catheterization |
Preparation of the site |
Catheter placement |
Antiseptic |
Teflon-coated, flexible J-curved |
|
guidewire |
Gauze, sterile drapes, and towels |
5F or other system |
Sterile gloves, masks, gowns, caps |
A 35-cm flexible pigtail catheter with |
A 5-mL or 10-mL syringe with a 25-gauge needle |
multiple fenestrations (end and side |
1% or 2% lidocaine (without epinephrine) |
holes) |
|
|
Emergency drugs |
|
Procedure |
Drainage system |
No. 11 blade |
A three-way stopcock |
A 20-mL syringe with 10 mL of 1% lidocaine |
Sterile IV tubing |
(without epinephrine) |
|
An 18-gauge, 8-cm, thin-walled needle with the |
A 500-mL sterile-collecting bag (or |
blunt tip |
bottle) |
Multiple 20and 50-mL syringes |
Sterile gauze and adhesive bag (or bottle) |
Hemostat |
Suture material |
Electrocardiogram machine |
|
Three red top tubes |
|
Two purple top (heparinized) tubes |
|
Culture bottles |
|
Postprocedure |
|
Suture material |
|
Scissors |
|
Sterile gauze and bandage |
|
2.5 cm of the skin surface). If bone contact occurs, then walk the needle behind the posterior (costal) margin. Reduce the angle of contact to 15° once the tip has passed the posterior margin of the bony thorax, and continue in the same direction.
•Further advancement is done with continuous aspiration. If electrocardiographic guidance is used, the sterile alligator clip is applied to the needle hub. Monitor continuous ECG throughout the procedure. Look for ST-segment elevation or premature ventricular contractions (evidence of epicardial contact) as the needle is advanced.
•End point:
–Advance the needle along this extrapleural path until a definite giveway is felt and fluid is aspirated from the pericardial space (usually 6.0–7.5 cm from the skin). Some patients may experience a vasovagal response at this point and require atropine intravenously to increase their blood pressure and heart rate.
–If ST-segment elevation or premature ventricular complexes occur (i.e., the needle in contact with pericardium), withdraw the needle
99 Pericardiocentesis |
801 |
|
|
toward the skin surface while aspirating, and if unsuccessful, then retry in the same way (caution is not to do any lateral motion as it can damage the epicardial vessels).
–Collect the samples and send investigations accordingly.
•Evidence of successful decompression
•Decreased intrapericardial pressure to levels between −3 and +3 mmHg:
–Fall in right atrial pressure and separation between the right and left ventricular diastolic pressures
–Increased cardiac output
–Increased systemic blood pressure
–Reduced pulsus paradoxus to physiologic levels (£10 mmHg) Please note that these blind techniques have a high incidence of morbidity and mortality, and they are no longer justified without echocardiography.
B.Echocardiography-guided intrapericardial catheterization pericardiocentesis
•Take an informed consent.
•The patient is placed in the semi-reclining position, slightly rotated leftward to enhance the fluid collection in the inferoanterior part.
•Define the site of entry and needle trajectory. The site of needle insertion is the place where the pericardial space is closest to the probe and the fluid accumulation is maximum.
•Local site preparation is the same as that for the percutaneous blind technique.
•A straight trajectory that avoids puncture of vital organs is chosen. The site should be 3–5 cm from the parasternal border to avoid puncture of the internal mammary artery. The optimal needle trajectory has to be preimagined by the operator.
•A 14–16-gauge Teflon sheath needle attached with a saline-filled syringe is used. On entering the fluid, a further advancement of 2 mm is advised; the sheath is advanced over the needle and the needle is withdrawn. Confirmation of the needle position is done by 5 mL of agitated saline and seen by echocardiography in the pericardial space.
•Seldinger technique is used to place a guidewire through the sheath, and then, sheath is removed. A series of skin dilation is then performed to finally allow an 8F, 35-cm flexible pigtail catheter to be guided over the guidewire into the pericardial space.
•Maintenance of the system—secure the pigtail with suture and connect it to a reservoir. Flush the drain every 4–6 h with 10–15 mL saline to maintain the patency.
•Other different methods and kits are now available as possible alternate techniques.
802 R. Chawla et al.
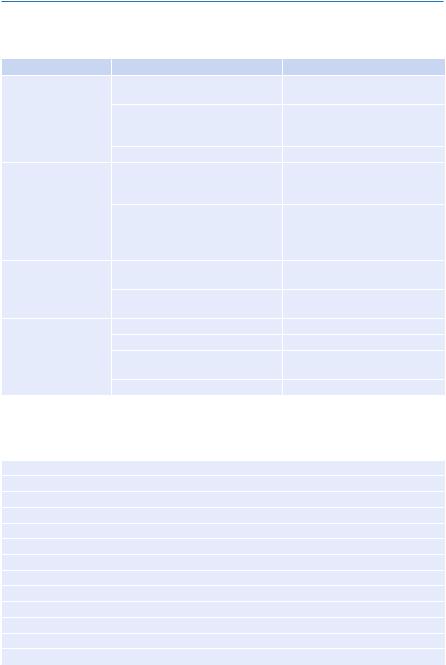
Step 5: Manage complications (Table 99.3)
Table 99.3 Management of complications |
|
|
|
Complications |
Prevention/treatment |
Structural damage |
Cardiac puncture with |
Careful procedure, urgent |
|
hemopericardium |
thoracotomy, and repair |
|
Coronary artery laceration |
Careful procedure, urgent |
|
(hemopericardium or myocardial |
thoracotomy, and repair |
|
infarction) |
|
|
Fistula formation |
Surgical correction |
Rhythm disturbance |
Arrhythmias, bradycardia, |
Often spontaneously revert, may |
|
ventricular tachycardia/ventricular |
need cardioversion/defibrillation/ |
|
fibrillation |
cardiopulmonary resuscitation |
|
Cardiac arrest (precipitated by |
Cardiopulmonary resuscitation |
|
pulseless electrical activity, |
according to ACLS protocol |
|
tachyarrhythmia, or |
|
|
bradyarrhythmia) |
|
Dysfunction |
Transient biventricular dysfunction |
Often reverts, vasopressors, and |
(cardiopulmonary) |
|
inotropes |
|
Pulmonary edema |
Manage according to standard |
|
|
practice |
Extracardiac |
Hemothorax |
Intercostal tube drainage (ICD) |
|
Pneumothorax |
ICD insertion |
|
Trauma to abdominal organs (liver, |
Careful procedure, better to do |
|
gastrointestinal tract) |
under sonological guidance |
|
Infection |
Standard therapy |
Step 6: Send investigations of pericardial fluid
Investigations
Hematocrit
White blood cell count with differential count
Glucose, protein, cholesterol, triglyceride
Amylase, lactate dehydrogenase
Gram’s stain
Routine aerobic and anaerobic cultures
Smear and culture for acid-fast bacilli
Cytology
Special cultures (viral, parasite, fungal)
Antinuclear antibody
Rheumatoid factor
Total complement, C3
