
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index

Pulse Oximetry and Capnography |
15 |
|
|
Deepak Govil and Sachin Gupta |
|
A 50-year-old male patient, a known case of chronic obstructive pulmonary disease (COPD), was admitted to the hospital with acute exacerbation. He was drowsy and cyanotic. His respiratory rate was 26/min. He was admitted for the management of COPD.
Pulse oximetry and capnography are essential components of respiratory monitoring in the intensive care unit.
Step 1: Examine the patient in detail and do pulse oximetry
•Presence of nonspecific symptoms and signs, which are suggestive of hypoxia, should be evaluated with objective measurements of oxygenation.
•Standard blood gas analyzer calculates oxygen saturation by partial pressure of oxygen plotted against the oxyhemoglobin dissociation curve for varying pH. Blood gas analyzer fitted with CO-oximeter directly measures oxygen saturation in the arterial blood sample (SaO2).
•The pulse oximeter is a medical device that indirectly monitors the oxygen saturation of patients’ blood and the changes in blood volume in the skin, producing a photoplethysmograph (SpO2).
Step 2: Understand the principle of pulse oximetry
•The fundamental physical property that allows the pulse oximeter to measure the oxygen saturation of hemoglobin is based on Beer–Lambert law, which relates to the concentration of a solute to the intensity of light transmitted through a solution.
D. Govil, M.D., F.C.C.M. (*) • S. Gupta, M.D.
Medanta Institute of Critical Care, Medanta – The Medicity Hospital, Gurgaon, India
e-mail: drdeepak_govil@yahoo.co.in
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
113 |
DOI 10.1007/978-81-322-0535-7_15, © Springer India 2012 |
|
114 |
D. Govil and S. Gupta |
|
|
•The pulse oximetry is based on two physical principles:
–The light absorbance of the oxygenated hemoglobin is different from that of the reduced hemoglobin, at the oximeter’s two wavelengths, which include red and near-infrared light.
–The absorbance of both wavelengths has a pulsatile component, which is due to the fluctuations in the volume of arterial blood between the source and the detector.
•Typically, a pulse oximeter has a pair of small light-emitting diodes (LEDs) facing a photodiode through a translucent part of the patient’s body, usually a fingertip or an earlobe.
•One LED is red, with the wavelength of 660 nm, and the other is infrared, with the wavelength of 905, 910, or 940 nm. Absorption at these wavelengths differs significantly between oxyhemoglobin and its deoxygenated form; therefore, the oxy-/deoxyhemoglobin ratio can be calculated from the ratio of the absorption of the red and infrared light.
•The microprocessor filters the extraneous signals or noises so that accurate oxygen saturation can be calculated.
•The arterial signal is pulsatile and it can be distinguished from nonpulsatile signals. The microprocessor can select out the absorbance of the pulsatile fraction of the blood, that is, due to arterial blood (AC), from the constant absorbance by nonpulsatile venous or capillary blood and other tissue pigments (DC), thus eliminating the effect of tissue absorbance to measure the oxygen saturation of arterial blood.
Step 3: Understand pitfalls and limitations
1.Dyshemoglobinopathies
•Pulse oximetry is considered to be accurate when oxygen saturation is between 70% and 100% provided that oxygenated hemoglobin and reduced hemoglobin are the only measured species of hemoglobin. But if methemoglobin and carboxyhemoglobin (COHb) increase in concentration, then the reliability of pulse oximetry becomes doubtful.
•Meth-Hb absorbs equal amount of red and infrared light, and the ratio is equal to 1 at 85% saturation. So even if the patient is hypoxic, the pulse oximeter will read 85%. Vice versa, if oxygen saturation is 100%, then the pulse oximeter will also read 85%.
•COHb absorbs very little light at 940 nm, while at 660 nm, its extinction coefficient is very similar to oxyhemoglobin. Thus, the presence of significant COHb will resemble the curve of oxyhemoglobin in the red range, with no effect on the infrared, and “look like” oxyhemoglobin, causing the pulse oximeter to overread.
•When these dyshemoglobins are suspected, then pulse oximetry should be supplemented by in vitro multiwavelength CO-oximetry.
2.Poor perfusion
•Poor perfusion leads to poor arterial pulse waveform, and so the pulse oximeter fails to detect the correct oxygen saturation. This can happen during
15 Pulse Oximetry and Capnography |
115 |
|
|
cardiopulmonary bypass (CPB), cold extremities, hypovolemia, low cardiac output, and peripheral vascular disease.
3.Arrhythmias
The pulse oximeter may not be able to detect the correct saturation during rapid atrial fibrillation or during intra-aortic balloon pump application.
4.Miscellaneous
•Black, blue, and green nail polishes give lower saturation.
•Values lower than 70% are not considered to be completely accurate.
•The movement of the patient like shivering or seizure will not give accurate measurements as the pulse oximeter fails to detect normal arterial pulsations.
•The hyperemic limb may show lower readings as capillary and venous flow becomes pulsatile.
•It cannot detect hypoventilation or hypercarbia despite good saturation. Despite a few limitations, the pulse oximeter remains a useful tool in the ICU as it can be read continuously and gives a reliable estimation of oxygen saturation of the patient.
Capnography
Step 1: Understand the principle of capnography
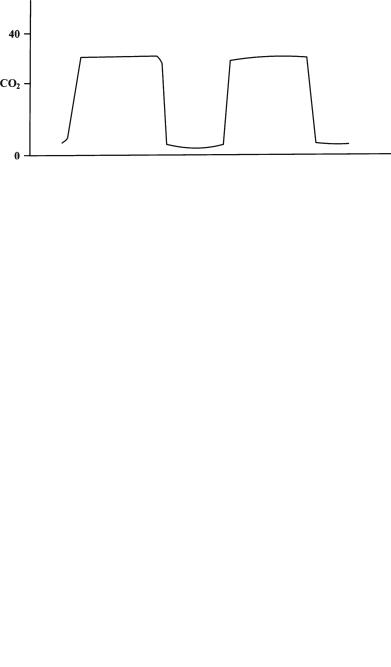
•Capnography is the graphic display of instantaneous CO2 concentration versus time (time capnogram) or expired volume (volume capnogram) during a respiratory cycle.
•The usefulness of capnography lies in checking the position of the endotracheal tube, ventilation, and perfusion status of the lung.
Principle
•The intensity of infrared radiation projected through a gas mixture containing CO2 is diminished by absorption.
•Expired air can be either analyzed as an inline device (mainstream) or sampled outside (sidestream).
Basic Physiology of Capnogram
•Assuming complete inspiration, there will be no CO2 in the large airways at the end of inspiration. As the patient starts exhaling, initially the CO2 sensor will not detect any CO2 as the exhalation comes from dead space.
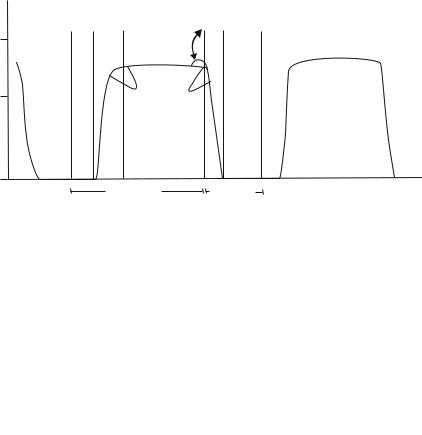
•As the exhalation continues, CO2 increases and reaches its peak and is detected at the sensor. After exhalation, as the patient starts inspiring, CO2 falls back to the zero baseline as he or she inspires CO2-free air. This gives rise to a typical waveform called capnogram (Fig. 15.1).
Phase I: At the start of exhalation, anatomical and physiological dead space is expired, so no CO2
Phase II: Exhalation continues, so CO2 rises Phase III: CO2 plateau
Phase IV: Inspiration
116 |
D. Govil and S. Gupta |
|
|
40
CO2
0
Fig. 15.1
Fig. 15.2
PHASE PHASE |
PHASE |
u |
PHASE |
|
I |
II |
III |
|
IV |
a b
Expiration |
Inspiration |
Normal Capnogram
Capnogram showing obstruction in the respiratory pathway
Step 2: Understand clinical applications of capnography
•Slanting and prolongation of expiratory phase is indicative of obstruction in the respiratory pathway, that is, either obstruction in the endotracheal tube or obstructive lung disease (Fig. 15.2).
•The elevation of the baseline is indicative of rebreathing, insufficient gas flows (Fig. 15.3).
•Contamination of the expired sample by fresh gas flows or sampling site too near to fresh gas (Fig. 15.4).
•Low EtCO2 indicates hyperventilation (Fig. 15.5).
•High EtCO2 indicates hypoventilation (Fig. 15.6).
•Sudden fall in EtCO2 can be due to asystole, hypotension, or massive pulmonary embolism (Fig. 15.7).
•This type of capnogram is observed when sudden CO2 is released after unclamping a major blood vessel or release of tourniquet (Fig. 15.8).
15 Pulse Oximetry and Capnography |
117 |
|
|
Fig. 15.3 Capnogram showing elevation of the baseline is indicative of rebreathing, insufficient gas flows
Fig. 15.4 Capnogram showing contamination of the expired sample by fresh gas flows or sampling site too near to fresh gas
Fig. 15.5 Capnogram showing Low EtCO2 indicates hyperventilation

Fig. 15.6 Capnogram showing high EtCO2 indicates hypoventilation
Fig. 15.7 Capnogram showing sudden fall in EtCO2 can be due to asystole, hypotension, or massive pulmonary embolism
Fig. 15.8 Capnogram showing sudden rise in CO2 after unclamping a major blood vessel or release of tourniquet

15 Pulse Oximetry and Capnography |
119 |
|
|
Fig. 15.9 Capnogram showing sudden fall and rise of EtCO2 is due to small air embolus
Fig. 15.10 Capnogram showing cardiac oscillations due to contraction and relaxation of the heart
• Sudden fall and rise of EtCO2 is due to small air embolus (Fig. 15.9).
• Cardiac oscillations are due to contraction and relaxation of the heart (Fig. 15.10).
•This shows a sedated and inadequately paralyzed patient having spontaneous respiratory efforts (Fig. 15.11).
•This shows respiratory efforts wearing off after giving muscle relaxant, called as curare effect (Fig. 15.12).
•It is helpful in weaning as it shows the return of spontaneous respiration (Fig. 15.13).
