
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index
Echocardiography |
17 |
|
|
Rahul Pandit and Jigeeshu V. Divatia |
|
A 55-year-old male patient was admitted to the intensive care unit (ICU) with a history of shortness of breath for the past 1 day. His pulse rate was 104/min, blood pressure was 80/40 mmHg, and respiratory rate was 32/min. His peripheries were cool. What is the role of bedside echocardiogram in evaluating this patient’s shock state?
Noninvasive, echocardiographic point-of-care monitoring has increasingly been used in ICUs. This has the advantage of easy and quick availability, repeatability, and avoids transportation of an unstable patient.
Intensivists should be familiar with basic echocardiography and use this as a basic screening tool for rapid assessment of the circulation in hemodynamically unstable patients as an extension of clinical examination. Detailed examination should be undertaken by intensivists who have had advanced training in echocardiography. Caution should however be exercised during interpretation of data provided, and patient management should be individualized within the clinical context.
Step 1: Urgent assessment and resuscitation
While resuscitation efforts are under way, a quick assessment with bedside echocardiogram can guide the clinician in rationalizing the use of volume resuscitation, inotropes, and vasopressors. This can be repeated to assess the response to therapy.
R. Pandit, M.D., F.C.I.C.M. (*)
Department of Critical Care, Seven Hills Hospital, Mumbai, India e-mail: dr_rapandit@yahoo.com
J.V. Divatia, M.D., F.I.S.C.C.M.
Department of Anaesthesiology, Critical Care and Pain, Tata Memorial Hospital, Mumbai, India
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
137 |
DOI 10.1007/978-81-322-0535-7_17, © Springer India 2012 |
|
138 |
R. Pandit and J.V. Divatia |
|
|
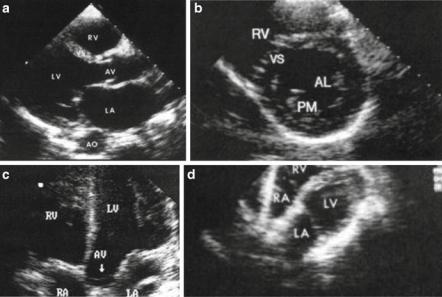
Fig. 17.1 Four basic views: (a) left parasternal long axis, (b) left parasternal short axis, (c) apical four chambers, and (d) subcostal
Using the bedside echocardiogram, one can assess the following:
•Left ventricular (LV) function
•Right ventricular (RV) function
•Presence of pericardial effusion and tamponade
•Preload assessment and fluid responsiveness
•Valve lesions
Step 2: Understand the limitation of bedside echo in the ICU
•ICU echos are often different.
–Patients are often supine, ventilated, and unconscious, leading to limited echo window.
–Other equipment can affect examination.
–The situation may be dynamic with concurrent resuscitation under way.
–Repeated studies may be required to determine the efficacy of treatment.
Step 3: Familiarize with practical aspects of bedside echo (Fig. 17.1a–d)
•Four basic views
1. Parasternal long axis
2. Parasternal short axis (papillary muscle level, mitral level, aortic level, and apex)
3.Apical view—four-chamber, five-chamber, and two-chamber view
4.Subcostal view
17 Echocardiography |
139 |
|
|
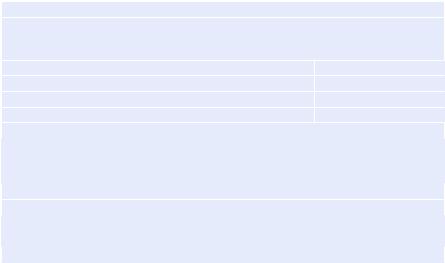
Table 17.1 Normal echo values
Size and wall thickness
M-mode performed in the parasternal long axis measuring perpendicular to LV through the mitral valve leaflet will give a reasonable estimation of LV systolic and diastolic diameter and interventricular septum and LV posterior wall thickness.
Dimensions |
Normal range |
End-diastolic LVID |
40–56 mm |
End-systolic LVID |
20–38 mm |
End-diastolic IVS and PW thickness |
<11 mm |
Left atrium and aortic root |
|
It can be measured by M-mode at the level of aortic valve and will give an estimation of LA size and aortic root.
LA normal range: <40 mm
Aortic root normal range: £25–30 mm
Ejection fraction (EF)
Normal contractility—EF > 50%
Hyperdynamic—EF > 70%
Low—EF < 50%
Step 4: Assess left ventricle (Table 17.1)
•This is best viewed in Parasternal long axis, short axis, and apical views.
•Focused left-sided heart examination
–Cavity size—small, normal, or dilated
–Contractility—normal, decreased, hyperdynamic
–Left ventricular wall thickness
–Aortic valve appearance, mitral valve appearance
–Segmental wall motion abnormality
•Size and wall thickness
–M-mode performed in the parasternal long axis measuring perpendicular to LV through the mitral valve leaflet will give a reasonable estimation of LV systolic and diastolic diameter and interventricular septum and LV posterior wall thickness.
•Left atrium and aortic root
–It is measured by M-mode at the level of the aortic valve. This will give an estimation of left atrium (LA) size and aortic root.
•Left ventricular wall thickness
–Presence of significant left ventricular hypertrophy (LVH) points to likely diastolic dysfunction.
–Systolic wall thickening is a guide to segmental wall motion defects.
•Contractility
–On 2D echo, subjective assessment by “eyeballing” is often used specially in emergency situations. It is useful to look at multiple views to make a reliable conclusion. Formal estimation of ejection fraction by different formulae is time consuming and needs good echo window and some experience.
140 |
R. Pandit and J.V. Divatia |
|
|
–Presence of spontaneous echo contrast (swirly smokelike movement in the ventricle) is an indication of the poor flow state
Step 5: Assess valves
•In the hemodynamically unstable patient, only the gross evaluation of appearance of valves is satisfactory.
Step 6: Assess the right ventricle
•This may be challenging due to the “U” shape of RV. A global assessment is sufficient.
–RV size—small, normal, or dilated
–RV contractility—decreased, normal, hyperdynamic
–Elevated RV pressure
–Tricuspid valve appearance
•RV size and contractility
–Size
•Subjective assessment: Apex of RV should be lower than the apex of LV in apical four-chamber view.
•Objectively, the RV–LV area ratio is estimated in apical four-chamber view. Normal: <0.6; mild to moderate dilatation: 0.6–1.0; major dilatation: >1.0.
–Contractility
•Tricuspid annulus peak systolic excursion calculated in apical four chambers by M-mode at the tricuspid annulus is a good estimation of RV contractility (normal: >20 m).
•Increased RV pressure.
–Dilated right atrium (RA) and RV
–Hyperdynamic RV contraction
–Paradoxical septal motion (Bowing of septum toward left ventricle)
–Pathognomic sign of markedly elevated RV pressures:
•Systolic septal flattening—pressure overload
•Diastolic septal flattening—volume overload
•Fixed septal flattening (bowed to the left, D-shaped LV)—both pressure and volume overload
•Tricuspid valve
–In an emergency situation, appearance with color Doppler for regurgitation is sufficient.
–Pulmonary artery peak pressure can be estimated using continuous wave Doppler in the presence of tricuspid regurgitation.
–4 V2 + CVP (where V is the velocity of regurgitant flow) is equal to pulmonary artery systolic pressure.
Step 7: Assess intravascular volume (preload)
•Care must be taken while estimating the preload as various pathophysiological states, mechanical ventilation, and position of the patient may alter its estimation.
•To assess preload, examine the inferior vena cava, right atrium, right ventricle, and left ventricle.
17 Echocardiography |
141 |
|
|
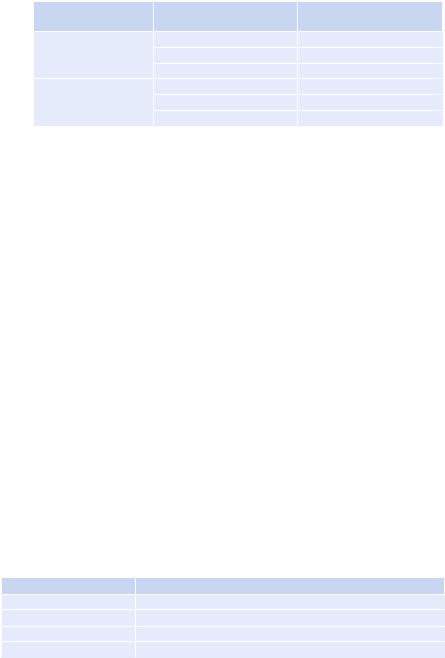
•Inferior vena cava (IVC)
–The IVC is best viewed by the subcostal approach. Measure using M-mode perpendicular to the IVC in subcostal view and look for diameter and collapsibility during inspiration and expiration in spontaneously breathing patients.
|
|
Estimated right atrial pressure |
IVC diameter |
Inspiration collapse (%) |
(RAP) (mmHg) |
Small or normal |
>55 |
0–5 |
(<2.1 cm) |
30–50 |
0–10 |
|
<35 |
Indeterminate |
Large (>2.1 cm) |
>55 |
0–10 |
|
35–55 |
10–15 |
|
<35 |
10–20 |
•This method does not apply to mechanically ventilated patients. In positive-pressure ventilation, IVC size and respiration response have poor correlations with RAP.
•However, an IVC size of more than 12 mm still predicts an RAP of approximately 10 mmHg.
•A large IVC may not necessarily imply elevated RAP. However, if there is IVC collapsibility of more than 35%, then small aliquots of fluid may be given until the collapse reduces.
•Right atrium
–Enlarged RA with persistent leftward septal bowing suggests elevated RAP.
–Enlarged LA with persistent rightward septal bowing suggests elevated left atrial pressure (LAP).
•Left ventricle
–Reduced or obliterated LV diameter in systole is indicative of volume depletion.
–Kissing LV septum and posterior wall is highly indicative of significant volume depletion.
Step 8: Assess pericardium
•Transthoracic echo is highly specific for diagnosing pericardial effusion and tamponade but has poor sensitivity for diagnosing pericardial thickening and constrictive pericarditis.
•The pericardial space is best viewed in the parasternal long axis and subcostal views.
•An echo-free space separating the epicardium and pericardium is suggestive of a pericardial effusion.
•The size of the effusion can be assessed by measuring the largest echo-free space in diastole.
Severity |
Characteristics |
Physiological |
End-systolic separation of epiand pericardium posteriorly |
Small |
Echo-free space of £10 mm |
Moderate |
Echo-free space of 10–20 mm surrounding the entire heart |
Large |
Echo-free space of >20 mm around the entire heart |
