
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index
Acute Febrile Encephalopathy |
32 |
|
|
Jignesh Shah and Shivakumar Iyer |
|
A 40-year-old male patient was admitted to hospital with a 2-day history of fever, headache, and increasing confusional state. On examination, he was disoriented to time and place, was opening eyes on verbal command, had an incomprehensible speech, and was moving all limbs appropriately. His neck was stiff and fundi were normal.
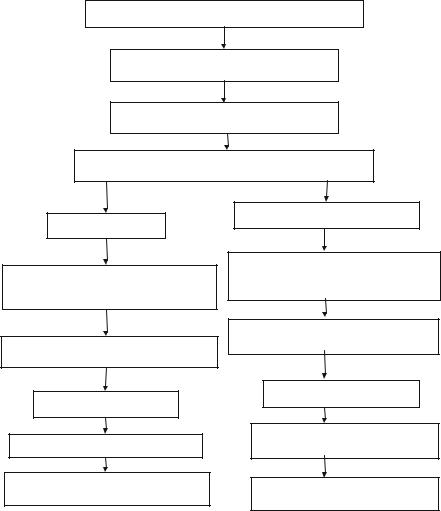
A high index of suspicion should be maintained for a diagnosis of an infection involving the nervous system in any patient with fever and altered mental state. Time is essence in managing these patients as any delay could lead to irreversible brain damage (Fig. 32.1).
Step 1: Initiate resuscitation and assess neurological status
•In neurological problems, assessment of airway and need for intubation is of paramount importance as these patients are at high risk of aspiration.
•Glasgow coma scale (GCS) below 8 usually requires airway protection (see Chap. 78).
Step 2: Take history and perform focused examination
•Patients presenting with fever and altered mental status can be broadly divided into three categories.
1. Primary central nervous system infection such as meningitis, encephalitis, and brain abscess
J. Shah, M.D., E.D.I.C. (*)
Department of Intensive Care Unit, Bharti Vidyapeeth Medical College, Pune, India e-mail: drshahjignesh@rediffmail.com
S. Iyer, M.D., E.D.I.C.
Department of Intensive Care Unit, Sahyadri Specialty Hospital, Pune, India
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
259 |
DOI 10.1007/978-81-322-0535-7_32, © Springer India 2012 |
|
260 |
J. Shah and S. Iyer |
|
|
Approach to the patient with fever and encephalopathy
Initial assessment and management of ABC
Check Blood Sugar, ABG and serum electrolytes
Evaluation for presence of focal neurological deficit
Focal neurological deficit
CT imaging to rule out primary CNS structural lesion or evidence of infective etiology (contrast scan)
LP, if no raised ICP or mass effect, specific CSF studies according to clinical context
No focal neurological deficit
Look for evidence of systemic infection, check WBCs, look for source of infection, procalcitonin/CRP
Appropriate investigations for search of source of sepsis, cultures
Treat accordingly
Prevention and treatment of raised ICP
Prevention of secondary injuries, e.g., aggressive control of fever and hyperglycemia
Treat accordingly
If no infection, review drug chart for drug fever, NMS, serotonergic syndrome
Consider endocrinopathies, malignant hyperthermia in relevant clinical context
Fig. 32.1 Acute febrile encephalopathy management
2.Systemic infection with confusional state
3.Noninfectious causes of fever and encephalopathy
•History and physical examination should be carried out systematically to identify the category in which the patients belong.
– Travel history (malaria, dengue, typhus, arbovirus infection)
– Drug history (steroids, other immunosuppressive)
– Trauma (splenectomy)
– Symptoms of ENT infection
– Neurosurgery

32 Acute Febrile Encephalopathy |
261 |
|
|
–Medical history of immunosuppressive disease, tuberculosis
–History of tuberculosis in close family members
•Neurological examination should be performed.
–Look for papilledema, airway reflexes, focal or lateralizing neurological signs, and neck stiffness.
•Perform systemic examination to look for a source of sepsis.
•Perform general examination for skin rash, eschar, injection marks (intravenous drug abuse).
Step 3: Initiate empirical treatment (Table 32.1)
•In neurological infection, time is of essence, so empirical therapy should be started, pending investigation especially in cases of suspected meningoencephalitis.
•Correct any obvious metabolic causes.
Table 32.1 Therapy for meningoencephalitis
Herpes encephalitis |
Acyclovir 10 mg/kg IV 8 hourly (adjust for renal |
|
impairment) for 2 weeks |
Bacterial meningitis |
|
Empirical (duration of therapy |
Ceftriaxone 2 g IV twice daily plus |
14 days) |
Vancomycin 10–15 mg/kg IV thrice daily |
|
Dexamethasone 0.15 mg/kg IV thrice daily for 4 days |
|
(prior to or concurrently with antibiotics) useful mainly |
|
in pneumococcal infection |
Streptococcus pneumoniae (duration |
Ceftriaxone 2 g IV twice daily or |
of therapy 14 days) |
Ceftriaxone 2 g IV twice daily plus |
|
Vancomycin 10–15 mg/kg IV thrice daily (if MIC of |
|
ceftriaxone >1 mcg/mL) |
Neisseria meningitidis (duration |
Ampicillin 2 g IV 4 hourly or |
of therapy 7 days) |
Ceftriaxone 2 g IV twice daily (if MIC to penicillin |
|
>0.1 mcg/mL) |
Listeria monocytogenes (duration |
Ampicillin 2 g IV 4 hourly or |
of therapy 21 days) |
Trimeth/sulpha 5 mg/kg 8 hourly (if allergic to |
|
penicillin) |
Postneurosurgery (Gram-negative |
Carbapenem + vancomycin |
bacilli and Staphylococcus aureus) |
|
Tubercular meningitis |
INH 5 mg/kg (300 mg in adults) |
|
Rifampicin (RIF) 10 mg/kg (600 mg in adults) |
|
Pyrazinamide (PZA) 15–20 mg/kg (maximum 2 g) |
|
Ethambutol (EMB) (15–25 mg/kg) |
|
Streptomycin (STM) (in selected cases) 15 mg/kg/day |
|
IM (maximum 1 g) |
Duration |
A four-drug regimen that includes INH, RIF, PZA, |
|
and either EMB or STM for 2 months followed by INH |
|
and RIF alone if the isolate is fully susceptible, for an |
|
additional 10 months |

262 |
J. Shah and S. Iyer |
|
|
Step 4: Send basic investigations
•General investigation workup, such as Complete blood count (CBC), blood culture, liver and renal profile, coagulation parameters, electrolyte (e.g., calcium) panel, chest X-ray, echocardiogram (to exclude vegetation), should be performed in all patients.
•Exclude systemic infection.
–In endemic areas, look for malaria (peripheral smear and antigen), leptospira (antibody), enteric fever (blood culture, antibody), dengue (antibody), typhus (antibody), and Japanese B encephalitis (antibody in serum and CSF). These will depend on geographic location of the patient.
Step 5: Send specific investigations
•It should be done expeditiously as time is of essence in these conditions.
•Empirical treatment should be started pending the investigation to prevent further brain damage.
•Neuroimaging
–CT scan/MRI of the brain (with contrast if not contraindicated).
–Care should be taken to transport these patients for neuroimaging, and judicious use of sedation should be done to avoid oversedation while facilitating proper image acquisition.
–If necessary, the patient should be intubated prior to imaging.
–Brain abscess is characterized by ring-enhancing lesion either single (frontal sinus infection), temporal (middle ear infection), or multiple (systemic infection). Herpes encephalitis will show bitemporal involvement.
–Decision for imaging should not delay starting the empirical therapy.
•Cerebrospinal fluid (CSF) study (see Table 32.2) (see Chap. 100)
–CSF examination is essential to diagnose meningoencephalitis.
–Coagulopathic state and thrombocytopenia need to be corrected prior to lumbar puncture (keep international normalized ratio [INR] <1.4 and platelet count >50,000).
–Prior brain imaging is required in patients with papilledema, seizures, or focal neurological signs.
–CSF should be examined immediately.
•Cell count and type
•Protein
•Glucose (simultaneous blood glucose estimation is important; CSF glucose value is normally 60–70% of blood glucose)
Table 32.2 CSF analysis in untreated meningitis |
|
|
||
CSF parameters |
Bacterial |
Tubercular |
Viral |
Fungal |
White cell count |
1,000–10,000 |
100–1,000 |
<300 |
50–200 |
Neutrophil (%) |
>80 |
<10 |
<20 |
<50 |
Protein (mg/dL) |
100–500 |
>250 |
Normal |
Mild rise |
Glucose (mg/dL) |
<40 |
<10 |
>40 |
<40 |
32 Acute Febrile Encephalopathy |
263 |
|
|
•Adenosine deaminase (ADA) (if tuberculosis is suspected)
•Gram stain, culture, and sensitivity
•Acid-fast bacilli (AFB) stain
•India ink for cryptococcal infection
•DNA PCR for herpes virus
•Cryptococcal antigen
•TB PCR and BACTEC TB culture
•Pneumococcal antigen
–A sample of CSF should be preserved by the laboratory for further testing.
–Classical CSF findings may change in partially treated meningoencephalitis.
Step 6: Take isolation precaution
•Proper respiratory isolation precaution should be taken in patients with suspected bacterial meningitis (see Chap. 48).
•The patient should wear mask during transportation.
Step 7: Look for noninfectious causes of fever and neurological features
•Structural brain lesions
–Intracerebral hemorrhage, pontine bleeding, and subarachnoid hemorrhage
•Drugs and toxins
–Organophosphorus, atropine, tricyclic antidepressants, phenothiazines, cocaine, and amphetamines
•Heat stroke
–Take history of exposure to extreme heat and exertion. Look for evidence of rhabdomyolysis.
•Neuroleptic malignant syndrome
–It is caused by central dopamine antagonism.
–Clinical features include hyperpyrexia with “lead-pipe” rigidity, extrapyramidal effects, and seizures.
–Other effects include rhabdomyolysis, renal failure, hepatic failure, and disseminated intravascular coagulation. Metabolic acidosis and elevated transaminases are common.
–Typical agents involved are haloperidol, chlorpromazine, promethazine, and prochlorperazine.
–A few atypical agents such as risperidone, olanzapine, and quetiapine are also responsible.
–Onset of symptoms is usually days to weeks after the inciting agent is started.
–Management includes withdrawal of inciting agents, cooling, dantrolene, and bromocriptine.
•Serotonergic syndrome
–It occurs within minutes to hours of initiating an offending agent.
–Symptoms are hyperreflexia, myoclonus, and hyperthermia.
–Inciting agents are selective serotonin receptor uptake inhibitors (SSRIs), tricyclic antidepressants, and trazodone.
