
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index
Scoring Systems |
84 |
|
|
Jigeeshu V. Divatia |
|
A 60-year-old male patient with cirrhosis of the liver and portal hypertension was admitted to the hospital with pneumonia. He developed septic shock and became encephalopathic and anuric. The family wanted to know the chances of survival. Can a scoring system be used to predict the chances of survival?
The annual mortality in the ICU patients of hospital A is 5% and of hospital B is 15%. Can it be concluded that the ICU patients of hospital B are poorly managed compared to that of hospital A?
Performance measures of ICU care are usually subjective and difficult to compare. An objective measure of the structure, processes, and outcome by prognosticating in a cohort of ICU patients makes it more meaningful and easier to compare. This also helps on rational allocation of resources. A severity scoring system also helps in controlling risk factors in intervention and control groups in clinical trials.
Step 1: Understand the type of scoring systems used in ICU population
•General risk-prognostication scores (severity of illness scores)
–Acute physiology and chronic health evaluation (APACHE II, III, and IV)
–Simplified acute physiology score (SAPS II and III)
–Mortality prediction model (MPM II0 and MPM II24)
•Disease and organ-specific risk-prognostication scores
–Ranson’s score for acute pancreatitis
–RIFLE and AKIN classification for acute kidney injury
–Trauma scores
–Glasgow coma score
J.V. Divatia, M.D., F.I.S.C.C.M. (*)
Department of Anaesthesiology, Critical Care and Pain, Tata Memorial Hospital, Mumbai, India
e-mail: jdivatia@yahoo.com
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
675 |
DOI 10.1007/978-81-322-0535-7_84, © Springer India 2012 |
|
676 |
J.V. Divatia |
|
|
–KILLIP—heart failure
–CURB—pneumonia
–CAM-ICU—delirium
•Organ dysfunction score—sequential organ failure assessment (SOFA)
•Nursing workload measurement—therapeutic intensity scoring systems (TISS)
•Population-specific—pediatrics—APGAR score
•Postoperative—PRISM
Step 2: Understand general ICU scoring systems
•All scoring systems are developed from large databases of ICU patients.
•Statistical modeling is used to determine the variables that are likely to impact survival.
•A summary score is derived from these variables, and the predicted mortality is calculated using predictive equations.
•The performance of the scoring system depends on the size and case mix of patients in the reference database and the methodology used to assign weights to different elements of the scoring system.
•APACHE II and SAPS II scoring systems were derived from datasets of patients in North American and European ICUs in the mid-1980s and early 1990s.
•The APACHE II scoring system assigns points to age, acute physiological observations based on the worst values in the first 24 h after admission for 12 variables, and specified preexisting chronic diseases. It also requires selection of a single diagnostic category for each patient. The predicted mortality is based on the APACHE II score and the diagnostic category (Table 84.1).
•The SAPS scoring system does not require ICU admission diagnosis for calculating the score.
•Both APACHE II and SAPS II did not account for lead-time bias (i.e., the time lag between the onset of critical illness and admission to the ICU).
•APACHE III was developed as a further refinement of APACHE II, but its mortality prediction equations are not in the public domain.
•The APACHE IV system (2006) is based on 110,558 patients in 104 North American intensive care and coronary care units between 2003 and 2004.
•SAPS III, published in 2005, was based on 16,784 patients aged 16 years or more from all continents. Three subscores—namely, patient characteristics before admission (5 variables), circumstances of admission (5 variables), and acute physiology (10 variables)—are summed up to produce the SAPS III score. A diagnostic category is essential for estimating mortality.
•Both APACHE IV and SAPS III account for lead-time bias, but have not been tested and validated as extensively as APACHE II and SAPS II.
•MPM II0, published in 1985, was the first general severity model to assess risk of death based on parameters assessed at ICU admission. Prediction models for assessment at admission and after 24 h (MPM II24) were developed originally. The models consist mainly of dichotomous variables.
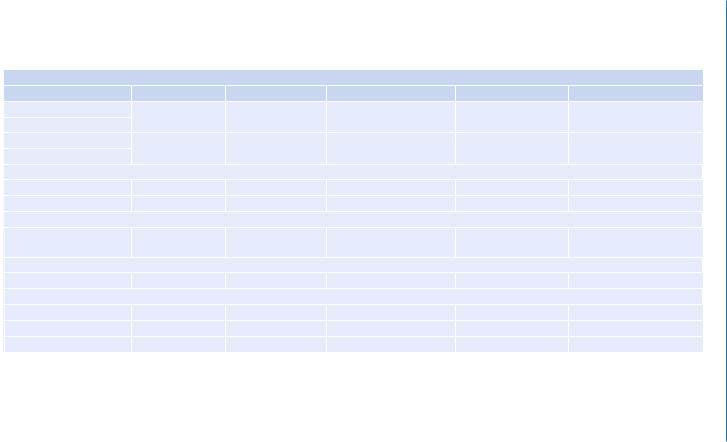
Table 84.1 The SOFA score
SOFA score
|
0 |
1 |
2 |
3 |
4 |
Respiration |
>400 |
£400 |
£300 |
£200 with respiratory |
£100 with respiratory |
PaO2/FiO2 |
|
|
|
support |
support |
Coagulation |
>150 |
£150 |
£100 |
£50 |
£20 |
Platelets (103/mm3) |
|
|
|
|
|
Liver |
|
|
|
|
|
Bilirubin (mg/dL) |
1.2 |
1.2–1.9 |
2.0–5.9 |
6.0–11.9 |
>12.0 |
(mmol/L) |
<20 |
20–32 |
33–101 |
102–204 |
>204 |
Cardiovascular |
|
|
|
|
|
Hypotension |
No hypotension |
MAP <70 mmHg |
Dopamine £5 or |
Dopamine ³5 or epi |
Dopamine >15 or epi 0.1 |
|
|
|
dobutamine (any dose)a |
0.1 (or norepi £0.1)a |
(or norepi ³0.1)a |
Central nervous system |
|
|
|
|
|
Glasgow coma score |
15 |
13–14 |
10–12 |
6–9 |
<6 |
Renal |
|
|
|
|
|
Creatinine (mg/dL) |
<1.2 |
1.2–1.9 |
2.0–3.4 |
3.5–4.9 |
>5.0 |
(mmol/L) |
<110 |
110–170 |
171–299 |
300–400 |
>400 |
or urine output |
|
|
|
or <500 mL/day |
or <200 mL/day |
Epi, epinephrine; norepi, norepinephrine
aAdrenergic agents administered for at least 1 h (doses given are in mg/kg/min)
Systems Scoring 84
677
678 |
J.V. Divatia |
|
|
Step 3: Understand organ failure scoring system
•The SOFA score is a descriptive score that uses routinely collected data for the calculation of a score of 0–4 for each organ, the higher number meaning more severe failure (Table 84.2).
•Daily scoring enables monitoring of the progress of organ dysfunction or failure.
•There are no equations to estimate mortality. However, high initial SOFA scores and worsening of SOFA scores over time correlate with increased mortality.
•The logistic organ dysfunction system (LODS) was developed for the evaluation of organ dysfunction on the first day of the ICU.
•It provides probability of hospital mortality, distinguishing it from merely descriptive models such as SOFA.
Step 4: Evaluate the scoring system
•The ability of the model to distinguish between patients who survive and patients who do not survive is termed discrimination.
•The area under the receiver operating characteristic curve (AUC) is used to give a graphical and numerical estimate of discrimination. If AUC is 0.5, it means the system is only as good as flipping a coin, and if AUC is 1, this indicates excellent discrimination.
•Calibration of a system examines the difference between the observed and expected deaths in patients grouped into different severity of illness.
•This can be evaluated graphically as well as by goodness-of-fit statistics using the Hosmer-Lemeshow test. If the p value is more than 0.05, the model provides a good fit for the data.
•The standardized mortality ratio (SMR=actual mortality/predicted mortality) also takes into account severity of illness and evaluates risk-adjusted ICU performance.
Step 5: Understand limitations of the scoring system
•None of the scoring systems are accurate enough to make predictions in individual patients and hence cannot be used to predict outcomes of individual patients.
•Most systems require data to be collected in the first 24 h after ICU admission; hence, the severity score cannot be used to decide whether to admit a patient to the ICU.
•Erroneous conclusions can be drawn if data are not collected correctly according to the original database and definitions of the scoring system.
•The score cannot be applied to patients excluded from the original database (e.g., patients younger than 16 or 18 years and patients with burns).
•Missing data and interobserver variability can affect accuracy.
•These scores may not be accurate in geographical regions, and case mix significantly different from that in the original database.
•All the scoring systems can only predict the behavior of a group of patients that matches the patients in the original database population.
•The commonly used APACHE II and SAPS II do not account for lead-time bias.
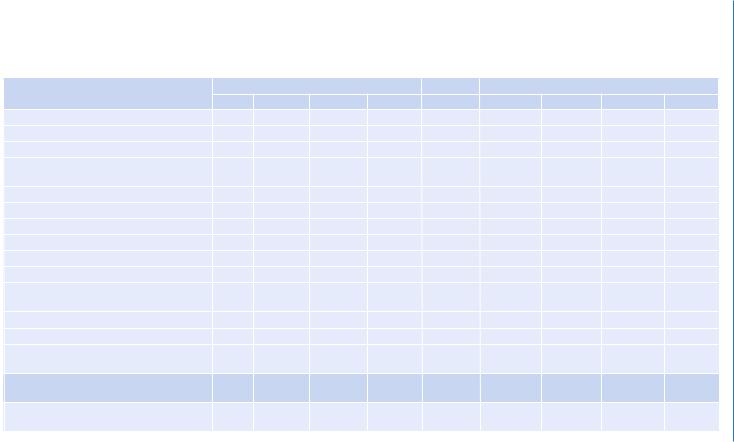
Table 84.2 The APACHE II scoring system |
|
|
|
|
|
|
|
|
|
|
High abnormal range |
|
|
|
Low abnormal range |
|
|
||
Physical variable |
+4 |
+3 |
+2 |
+1 |
0 |
+1 |
+2 |
+3 |
+4 |
Temperature—rectal (°C) |
>4 |
39–40.9 |
|
38.5–38.9 |
36–38.4 |
34–35.9 |
32–33.9 |
30–31.9 |
<29. 9 |
Mean arterial pressure (mmHg) |
³160 |
130–159 |
110–129 |
|
70–109 |
|
50–69 |
|
£49 |
Heart rate (ventricular response) |
³180 |
140–179 |
110–139 |
|
70–109 |
|
55–69 |
40–54 |
£39 |
Respiratory rate (nonventilated or |
³50 |
35–49 |
|
25–34 |
12–24 |
10–11 |
6–9 |
|
£5 |
ventilated) |
|
|
|
|
|
|
|
|
|
Oxygenation: A-aDO2 or PaO2 (mmHg) |
|
|
|
|
|
|
|
|
|
(a) FiO2 ³0.5 record A-aDO2 |
³500 |
350–499 |
200–349 |
|
<200 |
|
|
|
PO2 |
(b) FiO2 <0.5 record PaO2 |
|
|
|
|
PO2 >70 |
PO2 61–70 |
|
PO2 55–60 |
PO2 <55 |
Arterial pH |
³7.7 |
7.6–7.69 |
|
7.5–7.59 |
7.33–7.49 |
|
7.25–7.32 |
7.15–7.24 |
<7.15 |
Serum sodium (mMol/L) |
³180 |
160–179 |
155–159 |
150–154 |
130–149 |
|
120–129 |
111–119 |
£110 |
Serum potassium (mMol/L) |
³7 |
6–6.9 |
|
5.5–5.9 |
3.5–5.4 |
3–3.4 |
2.5–2.9 |
|
<2.5 |
Serum creatinine (mg/100 mL) (double- |
³3.5 |
2–3.4 |
1.5–1.9 |
|
0.6–1.4 |
|
<0.6 |
|
|
point score for acute renal failure) |
|
|
|
|
|
|
|
|
|
Hematocrit (%) |
³60 |
|
50–59.9 |
46–49.9 |
30–45.9 |
|
20–29.9 |
|
<20 |
White blood count (total/mm3) (in 1,000 s) |
³40 |
|
20–39.9 |
15–19.9 |
3–14.9 |
|
1–2.9 |
|
<1 |
Glasgow coma score (GCS) Score = 15 |
|
|
|
|
|
|
|
|
|
minus actual GCS |
|
|
|
|
|
|
|
|
|
[A] Total acute physiology score (APS) |
|
|
|
|
|
|
|
|
|
Sum of the 12 individual variable points |
|
|
|
|
|
|
|
|
|
Serum HCO3 (venous mMol/L) (not |
³52 |
41–51.9 |
|
32–40.9 |
22–31.9 |
|
16–21.9 |
15–17.9 |
£15 |
preferred, use if no ABGs) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
(continued) |
Systems Scoring 84
679
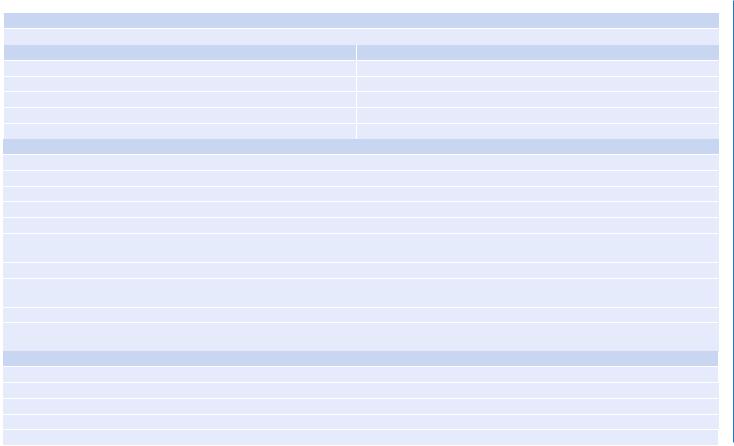
Table 84.2 |
(continued) |
[B] Age points |
|
Assign points to age as follows: |
|
Age (years) |
Points |
£44 |
0 |
45–54 |
2 |
55–64 |
3 |
65–74 |
5 |
³75 |
6 |
[C] Chronic health points
If the patient has a history of severe organ system insufficiency or is immunocompromised, assign points as follows:
(a)For nonoperative or emergency postoperative patients, 5 points
(b)For elective postoperative patients, 2 points
Definitions
Organ insufficiency or immunocompromised state must have been evident prior to this hospital admission and conform to the following criteria:
Liver: Biopsy-proven cirrhosis and documented portal hypertension, episodes of past upper GI bleeding attributed to portal hypertension, or prior episodes of hepatic failure/encephalopathy/coma.
Cardiovascular: New York Heart Association Class IV.
Respiratory: Chronic restrictive, obstructive, or vascular disease resulting in severe exercise restriction (i.e., unable to climb stairs or perform household duties, or documented chronic hypoxia, hypercapnia, secondary polycythemia, severe pulmonary hypertension (>40 mmHg), or respirator dependency).
Renal: Receiving chronic dialysis.
Immunocompromised: The patient has received therapy that suppresses resistance to infection (e.g., immunosuppression, chemotherapy, radiation, long-term or recent high-dose steroids), or has a disease that is sufficiently advanced to suppress resistance to infection (e.g., leukemia, lymphoma, and AIDS).
APACHE II score
Sum of [A] + [B] + [C]
A ASP Points____________________
B Age points____________________
C Chronic health points____________
Total APACHE II___________________
680
Divatia .V.J
