
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index

Acute Respiratory Failure |
2 |
|
|
Randeep Guleria and Jaya Kumar |
|
Case scenario 1
A 30-year-old male patient presented with acute onset of breathlessness, dry cough, fever, myalgia, and malaise for 4 days. On examination, he was found to be febrile and restless, with respiratory rate of 46/min and pulse rate of 124/min. His oxygen saturation was 80% on room air, and chest skiagram showed bilateral parenchymal infiltrate.
Case scenario 2
A 60-year-old male patient with chronic obstructive airway disease presented with increasing shortness of breath, cough, and expectoration for 5 days and drowsiness with confusion for 1 day. On examination, he was found to be drowsy, cyanosed with respiratory rate of 30/min, tachycardia, and flapping tremors. His oxygen saturation was 80% on initial evaluation, and a chest radiograph showed hyperinflated lung fields and right lower zone infiltrates.
Case scenario 3
A 30-year-old female patient with anxiety disorder presented to the emergency department in a comatosed condition with history of ingestion of some unknown tablets. On examination, she was found to be E2M4V1, with pulse rate of 64/ min, respiratory rate of 14/min, and blood pressure of 90/60 mmHg.
R. Guleria, M.D., D.M. (*) • J. Kumar, M.D.
Department of Pulmonary Medicine, All India Institute of Medical Sciences, New Delhi, India
e-mail: randeepg@hotmail.com
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
17 |
DOI 10.1007/978-81-322-0535-7_2, © Springer India 2012 |
|
18 |
R. Guleria and J. Kumar |
|
|
Acute respiratory failure results from the failure of respiratory system in one or both of its gas exchange functions—oxygenation and carbon dioxide elimination. It is a major cause of morbidity and mortality in intensive care units (ICUs). There are two types—type 1 hypoxic respiratory failure and type 2 hypercapnic respiratory failure.
Step 1: Initiate cardiopulmonary resuscitation
All patients should be resuscitated as mentioned in Chap. 78.
•Airway: In all patients with altered sensorium, a secure airway should be the first priority. This includes clearing the upper airway and keeping it patent. If the patient cannot maintain an airway, endotracheal intubation should be performed to keep the airway patent.
•Breathing: Once the airway is patent, the breathing has to be assessed. If it does not result in adequate gas exchange, oxygen supplementation and assisted ventilation may be required.
•Circulation: An intravenous access should be established and intravenous fluids should be started.
Step 2: Clinical assessment including history and detailed physical examination
•Take appropriate history and do detailed examination to distinguish whether the etiology is pulmonary or extrapulmonary and to know whether it is type 1 or type 2 respiratory failure (Tables 2.1 and 2.2). Assess the severity and find out the underlying cause and/or precipitating cause. Specific focus should be on the following:
–A detailed respiratory system and neurological assessment.
–Look for clinical features of hypoxia and hypercapnia (Tables 2.1 and 2.2).
–Signs of pulmonary hypertension and right ventricular failure.
–Clinical features of drug overdose.
–Chest wall deformity, obesity.
Step 3: Check pulse oximetry and do arterial blood gas analysis
Pulse oximetry and arterial blood gases are the mainstay of diagnosis and essential to decide on the therapeutic intervention.
•Oximetry is a rapid technique to know if there is significant hypoxia, but it gives no clue about the presence or absence of hypercapnia. Also, the severity of hypoxia on pulse oximetery should be interpreted cautiously if the patient is already on oxygen.
Table 2.1 Hypoxia-related |
Restlessness, anxiety |
clinical features |
Irritability, impaired intellectual functioning, |
|
|
|
and consciousness |
|
Cyanosis |
|
Tachycardia, hypertension |
|
Bradycardia, arrhythmia |
|
Shock, hypotension |
|
Convulsions, coma, death |
2 Acute Respiratory Failure |
19 |
|
|
Table 2.2 Hypercapniarelated clinical features
Headache
Drowsiness, confusion
Warm extremities, flushing, sweating
Bounding pulse, tachycardia
Tremors, myoclonic jerks, asterixis, seizures
Papilledema, coma
•Arterial blood gas analysis is essential for both diagnostic and therapeutic decisions.
–Type 1 respiratory failure is recognized by hypoxemia (PaO2 < 60 mmHg). With or without widening of alveolar-arterial oxygen gradient, PaCO2 is either low or normal.
–Type 2 respiratory failure is diagnosed when a PaO2 of less than 60 mmHg is associated with a PaCO2 of more than 45 mmHg and respiratory acidosis.
•This needs to be followed by an assessment of the pH and HCO3 to decide whether the type 2 respiratory failure is acute, acute on chronic, or chronic.
•Type II acute respiratory failure presents with low pH, high PaCO2, and normal HCO3; acute on chronic presents with low pH, high PaCO2, and high HCO3; while chronic respiratory failure presents with normal pH along with raised PaCO2 and HCO3.
•This should be followed by an assessment of alveolar-arterial oxygen gradient, which helps to narrow down the cause of respiratory failure (see appendix 2).
PaO2 = PiO2 - PaCO2 / R
Step 4: Differentiate between type 1 and type 2 respiratory failures
Type 1 respiratory failure occurs when the gas exchange is inadequate at rest or during exercise, leading to hypoxemia, and PaO2 is less than 60 mmHg (Table 2.3).
Type 2 respiratory failure occurs as a result of alveolar hypoventilation, which can be due to a pulmonary or extrapulmonary cause. Chronic obstructive pulmonary disease is the commonest cause of type 2 respiratory failure, but various other conditions listed below can also lead to hypercapnia and respiratory failure (Table 2.4).
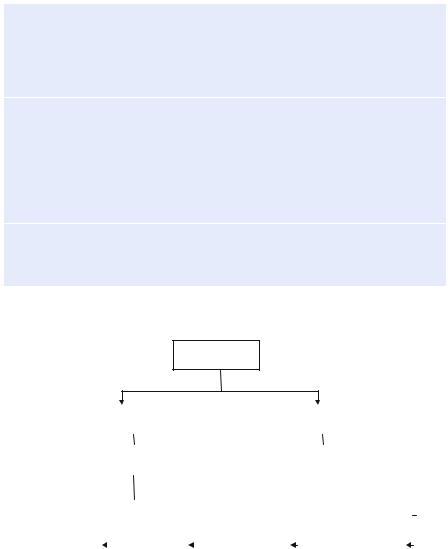
An approach to a patient with acute hypoxemic respiratory failure is summarized in Fig. 2.1.
Step 5: Send investigations
•Complete hemogram and biochemistry
•Lung function tests (if possible) that helps to differentiate between obstructive, restrictive, and mixed ventilatory defects
•Chest radiograph that may help to identify hyperinflation, pulmonary edema, pneumonia, pneumothorax, neoplasm and others to give a clue to the underlying etiology
•Electrocardiogram to identify cardiac disorders
20 |
R. Guleria and J. Kumar |
|
|
Table 2.3 Causes of hypoxemic respiratory failure
1.Ventilation/perfusion mismatch Airways disease
Chronic obstructive pulmonary disease Asthma
Cystic fibrosis Bronchiolitis obliterans
Alveolar filling
Cardiogenic Pulmonary edema Mitral valve stenosis
Acute respiratory distress syndrome Pneumonia
Alveolar hemorrhage Partial atelectasis Alveolar proteinosis
Transfusion related acute lung injury (TRALI) Acute interstitial pneumonia
Cryptogenic organizing pneumonia Aspiration, near-drowning
Pulmonary vascular disease—thromboembolism, fat embolism
2.Shunt
Alveolar filling—see the above causes Atelectasis
Intrapulmonary shunts—pulmonary AVM (Arterio Venous Malformation) Intracardiac shunt—PFO, ASD, VSD
3. Hypoventilation—refer to type 2 respiratory failure for causes of hypoventilation
4. Low inspired pressure of oxygen—high altitude
•Computed tomography (CT) or magnetic resonance imaging (MRI) if indicated for interstitial lung disease, neoplasm, stroke, and other neurological disorders
•Two-dimensional echocardiography for identification of cor pulmonale, intracardiac shunt, patent ductus arteriosus, and pulmonary embolism
Step 6: Initiate specific treatment
The primary aim is to maintain oxygenation and adequate alveolar ventilation and treatment for the underlying etiology. The key principles in the management of respiratory failure are as follows:
•Optimized oxygen therapy
•Identification of the underlying cause and adequate treatment for the same
•Clinical assessment and arterial blood gases to help decide the severity
•Treatment for any precipitating cause
•Appropriate pharmacological treatment
•Ventilatory support—noninvasive and invasive Oxygen therapy (see Chap. 14)
2 Acute Respiratory Failure |
21 |
|
|
Table 2.4 Causes of type 2 respiratory failure
Central nervous system depression/decreased ventilatory drive
Respiratory center (medulla) dysfunction
Drug overdose
Hypothyroidism
Sleep apnea
Central nervous system (CNS) causes— stroke, tumor
Neuromuscular diseases
Guillain–Barré syndrome
Poliomyelitis
Myasthenia gravis
Amyotrophic lateral sclerosis
Cervical cord lesions
Polyneuropathies
Muscle diseases like muscular dystrophy, polymyositis
Chest wall/pleural diseases
Kyphoscoliosis
Morbid obesity
Pneumothorax
Hypoxemic respiratory failure
|
|
Increased A-a |
|
|
|
|
|
|
|
Normal A-a |
|
|
|||||||||||
|
|
|
gradient |
|
|
|
|
|
|
|
|
|
gradient |
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
improvement with |
|
|
|
|
|
|
|
High PaCo2 |
|
|
|||||||||||
|
supplemental oxygen |
|
|
|
|
|
|
|
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Yes |
|
|
|
|
|
|
No |
|
|
|
|
Yes |
|
|
|
|
|
No |
|
||
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
V/Q mismatch |
|
|
|
|
Shunt |
|
|
|
Hypoventilation |
|
|
|
Low inspired O2 |
|
|||||||||
|
|
|
|
|
|
|
|
||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Fig. 2.1 An approach to hypoxemic respiratory failure to know the etiology
•The primary goal is to correct the hypoxemia to maintain adequate tissue oxygenation.
•Oxygen has to be given cautiously with monitoring as uncontrolled high-flow oxygen can lead to respiratory depression and worsening hypercapnia in type 2 respiratory failure. Oxygen saturation around 90% should be maintained.
