
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index

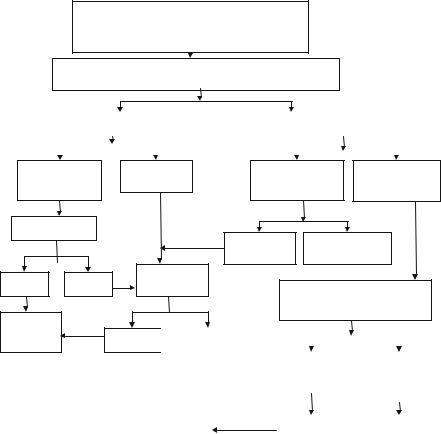
Pulmonary Thromboembolism |
9 |
|
|
Rajesh Chawla and Subhash Todi |
|
A 67-year-old male patient was admitted to hospital with severe communityacquired pneumonia and acute respiratory failure. He was treated with antibiotics and mechanical ventilation. He improved with the treatment and was extubated on day 4. On day 7, he suddenly developed acute severe breathlessness and chest pain.
Pulmonary embolism (PE) is the most common preventable cause of hospital death. PE should be suspected in all patients who present with new or worsening dyspnea, chest pain, or sustained hypotension without any other obvious cause. High index of suspicion and prompt management can improve survival in these patients. Mortality of acute PE is approximately 30%, which can be reduced to 2.5% by appropriate management
Step 1: Initiate resuscitation
•Provide oxygen to maintain saturation at more than 90% in suspected case of PE, and resuscitate as mentioned in Chap. 78.
•If the patient is hypotensive, administer 500–1,000 mL isotonic crystalloid. Any more volume resuscitation should be given with caution as it may increase right ventricle (RV) wall tension and cause ischemia and worsening of shock.
•Record a detailed medical history and perform physical examination.
R. Chawla, M.D., F.C.C.M. (*)
Department of Respiratory, Critical Care & Sleep Medicine, Indraprastha Apollo Hospitals, New Delhi, India
e-mail: drchawla@hotmail.com
S. Todi, M.D., M.R.C.P.
Critical Care & Emergency, A.M.R.I. Hospital, Kolkata, India
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
71 |
DOI 10.1007/978-81-322-0535-7_9, © Springer India 2012 |
|
72 |
R. Chawla and S. Todi |
|
|
Table 9.1 Revised Geneva
Score
The revised Geneva score: Older than 65 years (1 point) Previous DVT or PE (3 points)
Surgery or fracture within 1 month (2 points) Active malignant condition (2 points) Unilateral lower limb pain (3 points) Hemoptysis (2 points)
Heart rate
75–94 beats/min (3 points) or
95 beats/min or more (5 points)
Pain on lower limb deep venous palpation and unilateral edema (4 points)
The probability is assessed as follows:
Low probability (0–3 points)
Intermediate probability (4–10 points)
High probability (³11 points)
Step 2: Assess the risk factors
Assess the risk factors for PE and deep venous thrombosis (DVT) from medical history as mentioned below:
•Prior venous thromboembolism
•Immobility for more than 48 h—congestive heart failure, septic shock, surgery with general anesthesia, mechanical ventilation
•Abdominal or lower extremity surgery or trauma
•Hypercoagulable states
•Malignancy
•Spinal cord injury
•Heparin-induced thrombocytopenia
•Pregnancy or use of oral contraceptives
•Indwelling central venous catheters
•Obesity
•Congestive heart failure
Step 3: Assess clinical probability of PE
Clinical probability of PE is based on either clinical judgment or clinical decision rules (Revised Geneva Score) as mentioned in Table 9.1.
Step 4: Initiate treatment
•While diagnostic confirmation is awaited, anticoagulant treatment with subcutaneous low-molecular-weight heparin (LMWH), fondaparinux, or intravenous unfractionated heparin (UFH) should be initiated as soon as possible in patients with clinical probability of PE, if there are no contraindications.
•UFH is preferred in hemodynamically unstable patients in whom thrombolytic therapy is being planned. Patients are considered to be hemodynamically unstable if they are in shock or have a systolic blood pressure of less than 90 mmHg
9 Pulmonary Thromboembolism |
73 |
|
|
Table 9.2 Weight-based nomogram of heparin infusion |
|
APTT(s) |
Dose change |
<35 (1.2 × control) |
80 U/kg bolus, increase drip by 4 U/kg/h |
35–45 (1.2–1.5 × control) |
40 U/kg bolus, increase drip by 2 U/kg/h |
46–70 (1.5–2.3 × control) |
No change |
71–90 (2.3 × control) |
Reduce drip by 2 U/kg/h |
>90 (>3 × control) |
Hold heparin for 1 h, reduce drip by 3 U/kg/h |
or a drop in systolic pressure of more than 40 mmHg for more than 15 min in the absence of new-onset arrhythmia, hypovolemia, or sepsis.
•UFH is also preferred in the critically ill patients in the intensive care unit (ICU) with PE, requiring numerous procedures or in the patients suffering from renal failure.
•Dose adjustment for LMWH is required for patients with renal failure, obesity, pregnancy, and thrombophilias should ideally be titrated with antifactor Xa levels. Most of the patients with acute PE are candidates for initial anticoagulant
treatment with subcutaneous LMWH or fondaparinux or intravenous UFH. LMWH and fondaparinux are preferred over UFH.
The usual doses of anticoagulation for PE are mentioned below:
A. UFH:
•Give the bolus of 80 units IU/kg or 5,000 IU followed by infusion at 18 units IU/ kg/h, keeping activated partial thromboplastin time (APTT) between 1.5 and 2.5 times normal.
•Obtain stat APTT 6 h after heparin bolus and after 6 h of dose change.
•When two consecutive APTT levels are in therapeutic range, order APTT (and readjust heparin drip as needed) every 24 h.
Adjust heparin infusion based on the sliding scale mentioned in Table 9.2 .
B. Enoxaparin:
• 1 mg/Kg s/c twice a day.
C. Dalteparin 5,000 units s/c twice daily.
D. Fondaparinux:
•Weight <50 kg—5 mg s/c once a day.
•Weight 50–100 kg—7.5 mg s/c once a day.
•Weight >100 kg—10 mg s/c once a day.
Step 5: Order investigations
•Electrocardiogram, X-ray chest (posteroanterior view), and arterial blood gas analysis should be ordered in all these patients. Although these tests are nonspecific, they do increase the index of suspicion.
•Baseline prothrombin time (PT), partial thromboplastin time (PTT), and platelet count.
•Renal functions test.
74 |
R. Chawla and S. Todi |
|
|
•Choice of further investigations will depend on:
(a)Index of suspicion of PTE
(b)Hemodynamic stability of the patient
(c)Availability of tests at the center
(d)Sensitivity, specificity, and positive predictive value of the test
•If the patient has a high probability of PE clinically or on the basis of a high probability score, and can be safely moved to computed tomography (CT) room and is in a position to cooperate with breath holding, he/she should undergo multidetector CT (MDCT) for CT pulmonary angiography, irrespective of his/her hemodynamic status.
•If the patient is hemodynamically unstable and has a high probability of PE clinically or on the basis of a high probability score, and is critically ill and cannot be shifted, he/she should be subjected to echocardiography preferably transesophageal echocardiography (TEE) and lower extremity ultrasonography. His/her blood sample should be sent for a D-dimer level. A negative echo and venous Doppler, however, do not rule out clinically significant PE. Efforts should be made to stabilize the patient hemodynamically, and once the patient stabilizes, he/she should be sent for MDCT pulmonary angiography, if doubt still remains about the diagnosis.
•If the patient is hemodynamically stable and has a low or medium probability score, then order a high-sensitivity D-dimer level (enzyme-linked immunosorbent assay).
•If high-sensitivity D-dimer is positive (level more than 500 ng/mL) in low or medium probability, further testing with MDCT pulmonary angiography is indicated.
•If high-sensitivity D-dimer is negative in low or medium probability, the risk of PTE is very low (0.14%) and no further testing is required.
•Remember that the specificity of an increased D-dimer level is reduced in patients with cancer, in pregnant women, and in hospitalized and elderly patients. A value less than 500 ng/ml is rarely seen in most hospitalized patients in the ICU because they have a high fibrin turnover during critical illness, thus limiting its value in these patients. A negative high-sensitivity D-dimer rules out PE in low and medium probability, and a negative moderate sensitivity D-dimer rules out PE only in low probability cases.
•A ventilation/perfusion scan may be done in patients with a high probability of PE and where there is a contraindication for CT such as renal failure or if CT scan is not available.
•In pregnant women with clinical findings suggestive of PE, an MDCT chest should be done. The concern about radiation is overcome by the hazard of missing a potentially fatal diagnosis or exposing the mother and fetus to unnecessary anticoagulant treatment. MDCT delivers a higher dose of radiation to the mother, but a lower dose to the fetus than ventilation/perfusion scanning. Venous ultrasonography of legs and 2-D echocardiography can be done in these patients before MDCT.

9 Pulmonary Thromboembolism |
75 |
|
|
Table 9.3 Risk stratification of patients with PE also has potential clinical implications for triage
Absence of right ventricular dysfunction and normal troponin level—admit in ward
Hemodynamically stable with right ventricular dysfunction or injury—admit the patient in High Dependency Unit (HDU)
Hemodynamically unstable and right ventricular dysfunction and injury—admit to the ICU
Table 9.4 Thrombolytic therapy regimens for acute PE
Drug |
Protocol |
Streptokinase |
250,000 U IV (loading does during 30 min; then 100,000 |
|
U/h for 24 h) |
Urokinase |
2,000 U/lb IV (loading does during 10 min; then 2,000 |
|
U/lb/h for 12–24 h) |
Tissue-type plasminogen activator |
100 mg IV during 2 h |
Step 6: Identify the risk of adverse outcome for triage
•Risk stratification should be done promptly because fatal PE generally occurs early after hospital admission (Table 9.3).
•It is based on clinical features and markers of myocardial dysfunction or injury.
•If the patient is hemodynamically stable, then order TEE, troponin, and brain natriuretic peptide (BNP) levels.
•Myocardial dysfunction (right ventricular dilatation, hypokinesia, and ventricular septal bowing) based on echo and injury markers (elevated troponin and BNP) is useful and helps decide about thrombolysis, as mentioned below (Table 9.3 ).
The risk of adverse outcome is more in the following situations:
Shock (systolic blood pressure <90 mmHg) and/or BP drop ³40 mmHg for >15 min and sustained hypotension
Immobilization due to neurological disease Age 75 years or more
Cardiac, renal, or respiratory disease or cancer
Step 7: Consider thrombolysis
(a)If the patient is hemodynamically unstable
•Admit to the ICU
•Start anticoagulation, preferably intravenous UFH. Keep APTT time 1.5– 2.5 to normal.
•Administer thrombolytic therapy (Table 9.4) if there are no contraindications (Table 9.5). Discontinue heparin during thrombolysis.
•Give other supportive measures to stabilize the patient.
(b)Hemodynamically stable patients with right myocardial dysfunction and injury suggested by TEE and markers (raised troponin and BNP) may also be considered for thrombolytic therapy if there are no contraindications (Table 9.5).

76 |
R. Chawla and S. Todi |
|
|
Table 9.5 Contraindication for thrombolytic therapy
Absolute contraindications
Prior intracranial hemorrhage
Known structural cerebral vascular lesion Known malignant intracranial neoplasm Ischemic stroke within 3 months Suspected aortic dissection
Active bleeding or bleeding diathesis (excluding menses), significant closed-head trauma or facial trauma within 3 months
Relative contraindications
History of chronic, severe, poorly controlled hypertension
Severe uncontrolled hypertension on presentation (systolic blood pressure >180 mmHg or diastolic blood pressure >110 mmHg)
Traumatic or prolonged (>10 min) CPR or major surgery less than 3 weeks Recent (within 2–4 weeks) internal bleeding
Noncompressible vascular punctures
For streptokinase/anistreplase—prior exposure (more than 5 days ago) or prior allergic reaction to these agents
Pregnancy
Active peptic ulcer
Current use of anticoagulant (e.g., warfarin sodium) that has produced an elevated international normalized ratio (INR) > 1.7 or PT > 15 s
Step 8: Hemodynamically stable patients with PE without myocardial dysfunction or injury
•Admit to the ward.
•Anticoagulate with LMWH or fondaparinux or UFH.
•Closely watch for vitals and respiratory distress. Consider early mobilization.
Step 9: Consider invasive treatment
Patients in whom thrombolytic therapy is contraindicated and whose hemodynamic status does not improve with medical treatment, the following should be considered:
•Percutaneous mechanical thrombectomy (thrombus fragmentation and aspiration)
•Surgical embolectomy
Step 10: Initiate vitamin K antagonist therapy
•Vitamin K antagonist (warfarin) should be initiated as soon as possible, preferably on the first treatment day, and heparin should be continued.
•Heparin should be discontinued when INR reaches a level of 2.0 or higher for at least 24 h. Duration of treatment is usually for 3–6 months.
•LMWH is preferred over warfarin in cancer and in pregnant women for longterm treatment.
9 Pulmonary Thromboembolism |
77 |
|
|
Step 11: Inferior vena caval filters
They are indicated in the following conditions:
•Contraindication to anticoagulation therapy
•Recurrent thromboembolism despite anticoagulant therapy
•Bleeding while on anticoagulants
Step 12: Long-term treatment
Patients should be started on lifelong anticoagulant treatment in the following conditions:
•Recurrent PE
•Cancer
•Suspected Pulmonary Embolism
•Acute dyspnea, chest pain, or sustained hypotension
with no obvious cause
Clinical probability assessment-clinically
or by score - Wells and Revised Geneva Score
|
Hemodynamically stable |
|
Hemodynamically unstable |
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Low/intermediate clinical probability
High density D-
Dimer testing
Normal Elevated
Pulmonary embolism ruled out
High clinical probability
MDCT
Critically ill but can be
Critically ill and
moved to CT room
cannot be moved to CT room
MDCT available MDCT Not available 
Transthoracic or Transesophageal (preferable) echocardiography and compression USG both lower limbs
Negative |
|
Pulmonary |
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
||||
|
embolism |
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
||
|
|
|
confirmed |
|
Right ventricular |
|
No right |
||||
|
|
|
|
|
|
dysfunction and/or |
|
ventricular |
|||
|
|
|
|
|
|
DVT |
|
dysfunction |
|||
|
|
|
|
|
|
|
|
|
|
and DVT |
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
MDCT once stable |
|
|
|
Treat* |
|
Search for |
||||
|
|
|
|
alternative |
|||||||
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
diagnosis |
|
|
|
|
|
|
|
|
|
|
|
|
|
Fig. 9.1 Approach to a patient of suspected acute pulmonary embolism. MDCT Multidetector CT with pulmonary angiography, *Please refer to text
