
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index

Syndromic Approach to Poisoning |
69 |
|
|
Praveen Aggarwal |
|
A 45-year-old male patient presented to the emergency department with altered mental status. According to the relatives, patient had ingested unknown liquid about half an hour ago. His pulse was 110/min, blood pressure was 90/69 mmHg, and pupils were small. His breath had a garlic-like odor. He had profuse sweating and incontinence of urine. Chest auscultation revealed bilateral rhonchi and crepitations.
Toxidromes are constellations of symptoms commonly encountered with certain drug classes. Evaluation of possible poisoning should include laboratory studies with complete metabolic profiles, electrolyte estimation, and liver and renal functions.
Step 1: Initial resuscitation
•The initial approach in any emergency in an unconscious patient includes standard resuscitation with care of circulation, airway and breathing along with cervical spine immobilization (as the patient is in altered mental status, which could be due to trauma).
•High-flow oxygen and intravenous fluids should be administered, and blood should be sent for urgent blood glucose, urea and electrolytes, and arterial blood gases.
•Once the patient has been stabilized, the physician must consider how to minimize the bioavailability of toxin not yet absorbed, which antidotes (if any) to administer, and other measures to enhance elimination.
P. Aggarwal, M.D., D.N.B. (*)
Department of Emergency Medicine, All India Institute of Medical Sciences, New Delhi, India
e-mail: peekay_124@hotmail.com
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
553 |
DOI 10.1007/978-81-322-0535-7_69, © Springer India 2012 |
|
|
|
|
554 |
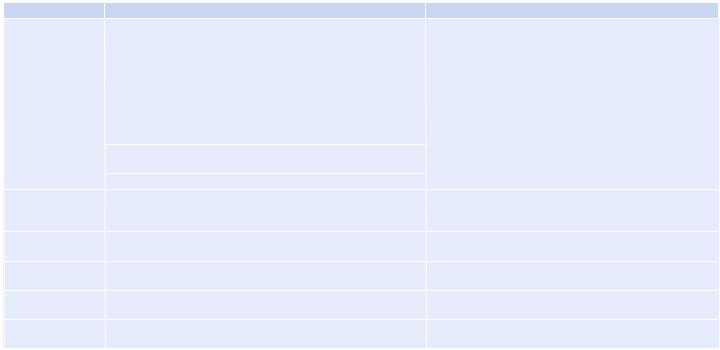
Table 69.1 Toxidromes |
|
|
|
Toxidrome |
Clinical features |
Toxins |
|
Cholinergic |
Muscarinic features (DUMBELS): |
Organophosphate and carbamate insecticides, nerve agents |
|
|
D—diarrhea |
(Soman, Tabun, sarin, VX), nicotine |
|
|
U—urination |
|
|
|
M—miosis |
|
|
|
B—bronchorrhea, bronchoconstriction, bradycardia |
|
|
|
E—emesis |
|
|
|
L—lacrimation |
|
|
|
S—salivation, sweating |
|
|
|
Nicotinic features: mydriasis (uncommon), hypertension, muscle |
|
|
|
weakness, tachycardia, fasciculations |
|
|
|
CNS features: confusion, coma, convulsion |
|
|
Anticholinergic |
Constipation, retention of urine, mydriasis, dry lungs, dry and hot |
Atropine, Datura, antihistamines, tricyclic antidepressants, |
|
|
skin, dry mouth, hypertension, abnormal movements, tachycardia, |
gyromitrin (found in a mushroom) |
|
|
hyperthermia, hallucinations, delirium |
|
|
Opioid |
Coma, pinpoint pupils, respiratory depression, bradycardia, |
Opiates (heroin, pethidine, morphine, dextropropoxyphene, |
|
|
hypotension, hypothermia |
loperamide, opium) |
|
Sympathomimetic |
Sweating, tremors, tachycardia, hypertension, hyperthermia, |
Caffeine, theophylline, amphetamines, cocaine, phencyclidine |
|
|
mydriasis, tachypnea, agitation, hyper-alert, seizures |
(PCP), sedative/hypnotic withdrawal |
|
Hallucinogenic |
Hallucinations, depersonalization, agitation, hyperthermia, |
Lysergic acid diethylamide, PCP, gamma-hydroxybutyrate |
|
|
tachycardia, hypertension, nystagmus, mydriasis |
(GHB), psilocybin (found in a mushroom) |
|
Hypnotic–sedative |
CNS depression, confusion, stupor, coma, bradycardia, hypotension, |
Barbiturates, methaqualone, meprobamate |
|
|
hypopnea, miosis, hyporeflexia |
|
.P |
|
|
Aggarwal |
|
|
|
|
|
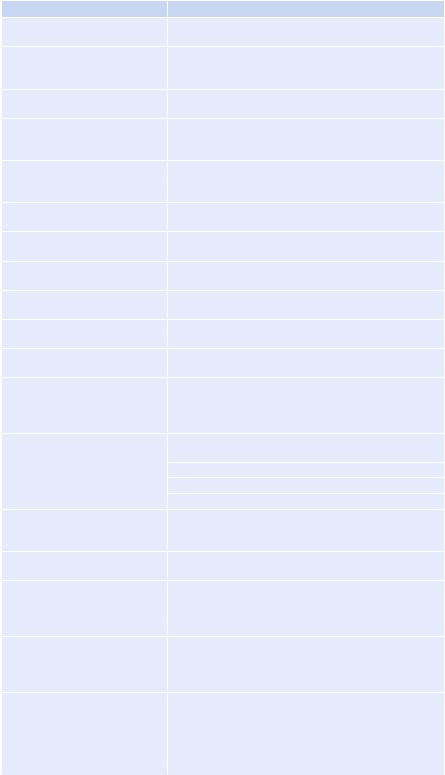
Table 69.2 Commonly encountered features and likely toxins
Features |
Toxins/causes |
Bradycardia |
b-Blockers, cholinergic agents, clonidine, calcium channel |
|
blockers, ethanol, digoxin, opiates, cholinergics |
Tachycardia |
Sympathomimetics (cocaine, caffeine, theophylline, |
|
amphetamines), anticholinergics, reflex tachycardia due to |
|
hypotension |
Hypothermia |
Carbon monoxide, opiates, hypoglycemic agents, alcohol, |
|
sedative hypnotics |
Hyperthermia |
Nicotine, antihistamines, anticholinergics, sympathomi- |
|
metics, aspirin, antidepressants, neuroleptic malignant |
|
syndrome |
Hypotension |
Antihypertensive drugs, aluminum phosphide, cholin- |
|
ergics, digoxin, antidepressants, phenothiazines, sedative |
|
hypnotics, opiates |
Hypertension |
Cocaine, theophylline, sympathomimetics, caffeine, |
|
anticholinergics, nicotine |
Hypoventilation |
Narcotics, sedative hypnotics, alcohol, GHB, botulism, |
|
clonidine |
Hyperventilation |
Salicylates, amphetamines, theophylline, metabolic |
|
acidosis (respiratory compensation) |
Coma |
Sedative hypnotics, opiates, alcohols, clonidine, carbon |
|
monoxide, antidepressants |
Mydriasis |
Sympathomimetics, anticholinergics, antidepressants, |
|
withdrawal (alcohol, opiate, sedative hypnotic) |
Miosis |
Organophosphates and carbamates, clonidine, opiates, |
|
phenothiazines, sedative hypnotics |
Seizures |
Organophosphates, antidepressants, INH, sympathomimetics, |
|
camphor, cocaine, amphetamines, theophylline, PCP, |
|
withdrawal (ethanol, benzodiazepines), lithium, lidocaine, |
|
lead, organochlorines (e.g., lindane, DDT), hypoglycemia |
Breath odor |
Garlic: organophosphate and carbamate insecticides, |
|
aluminum phosphide, arsenic, phosphorus |
|
Rotten eggs: hydrogen sulfide |
|
Moth ball: naphthalene |
|
Bitter almonds: cyanides |
Prolonged QT interval on ECG |
Carbamazepine, propoxyphene, quinidine, procainamide, |
|
terfenadine, astemizole, tricyclic antidepressants, cocaine, |
|
phenothiazines |
Noncardiogenic pulmonary edema |
Opiates, barbiturates, salicylates, irritant gases |
on chest X-ray |
|
Radio-opaque toxins on abdominal |
Chloral hydrate, heavy metals (lead, arsenic, mercury), |
X-ray (absence of radio-opaque |
iron, phenothiazines, body packers, sustained-release |
shadow does not exclude |
medicines |
poisoning by listed toxins) |
|
Elevated anion gap (normal |
Alcoholic ketoacidosis, cyanide, carbon monoxide, aspirin, |
8–12 mEq/L) [Anion |
toluene, methanol, ethylene glycol, metformin, uremia |
gap = Na+–(HCO3 + Cl–)] |
(due to renal toxicity), iron, INH, lactic acidosis (due to |
|
hypotension or hypoxia) |
Elevated osmolar gap |
Ethanol, methanol, ethylene glycol, isopropanol |
(>10 mOsmol/L) |
|
[Osmolar gap = measured |
|
osmolality–calculated osmolarity] |
|
[Calculated osmolarity = |
|
2Na++BUN/2.8 + glucose/18] |
|

556 |
P. Aggarwal |
|
|
Step 2: Diagnosis by toxidromic approach
After initial stabilization, it is important to diagnose the type of poison ingested by the patient. This can be done by detailed history, examination, and simple laboratory tests, which include blood glucose, electrolytes, acid–base analysis, urine exam, and ECG. Based on history and examination, it may be possible to define a constellation of signs and symptoms or toxidromes, which may help in diagnosing the unknown poison. Common toxidromes are listed in Table 69.1. Antidotal and supportive treatment can then be provided.
Step 3: Diagnosis of the type of poison if clinical features not suggestive of a toxidrome
In many cases, a clear-cut toxidrome cannot be defined based on presenting clinical features. In such cases, prominent features may be used to diagnose the type of poison involved. Table 69.2 lists some of the commonly encountered features and the likely toxins.
Step 4: Decontamination, enhancing excretion, antidotal, and supportive treatment
Based on the likely poison, antidotal treatment should be instituted. However, supportive treatment is the most vital treatment in such patients. These topics have been discussed in Chap. 68.
Suggested Reading
1.Hill GE, Ogunnaike B, Nasir D. Patients presenting with acute toxin ingestion. Anesthesiol Clin. 2010;28:117–37.
This review of drug/toxin-induced injury discusses drug or toxin-induced pathology that the clinician may encounter and therapeutic approaches to these syndromes.
2.Frithsen IL, Simpson WM Jr. Recognition and management of acute medication poisoning. Am Fam Physician. 2010;81:316–23.
This article discusses overall management of acute medication poisoning.
3.Holstege CP, Dobmeier SG, Bechtel LK. Critical care toxicology. Emerg Med Clin North Am. 2008;26:715–39.
This article reviews the general approach and management of the critically poisoned patient. Complications of poisoning that may bring a rapid demise of the critically ill poisoned patient are highlighted and the management of those complications is discussed.
4.Tetrault JM, O’Connor PG. Substance abuse and withdrawal in the critical care setting. Crit Care Clin. 2008;24:767–88.
This article reviews the epidemiology of substance use in this population and the treatment of common withdrawal syndromes. The authors stress the importance of long-term planning as part of the overall treatment protocol beyond the acute presentation.
5.Erickson TB, Thompson TM, Lu JJ. An approach to the patient with an unknown overdose. Emerg Clin North Am. 2007;25:249–81.
This article reviews the management of unknown poisoning.
6.Koren G. A primer of paediatric toxic syndromes or ‘toxidromes’. Paediatr Child Health. 2007;12:457–9.
