
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index
Massive Hemoptysis |
8 |
|
|
Avdhesh Bansal and Viny Kantroo |
|
A 36-year-old chronic alcoholic male patient presented to the emergency department with history of a large amount of blood being coughed out for the past 24 h. He had had three such episodes, the last one just about 1 h ago. There was no history of such previous episodes in the past. Although there was no history of fever, he had been feeling weak for the past 2 weeks.
Hemoptysis is defined as coughing of blood from the respiratory system. Hemoptysis is one of the important symptoms of cardiopulmonary disease. It can be mild or severe requiring admission to the intensive care unit (ICU). If massive hemoptysis is not treated aggressively, it is associated with significant mortality.
Step 1: Initiate resuscitation
Take history of the patient and find out the approximate amount of hemoptysis. Severe hemoptysis is defined as hemoptysis of more than 400–600 mL/24 h. After a quick physical examination of the patient, initiate resuscitation.
Airway:
•Maintaining an open airway should be the first priority in the management. The main objective is to prevent asphyxiation.
•Intubate with single-lumen endotracheal tube in cases of severe and diffuse endobronchial bleeding. It may achieve immediate control of the airways to allow
A. Bansal, M.D., F.R.C.P. (*)
Department of Respiratory, Critical Care & Sleep Medicine, Indraprastha Apollo Hospitals, New Delhi, India
e-mail: avdeshb@hotmail.com
V. Kantroo, D.N.B.
Department of Respiratory Medicine & Critical Care, Indraprastha Apollo Hospitals, New Delhi, India
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
65 |
DOI 10.1007/978-81-322-0535-7_8, © Springer India 2012 |
|
66 |
A. Bansal and V. Kantroo |
|
|
adequate suctioning and diagnostic and therapeutic fiber-optic bronchoscopy. It may also be helpful in cases of nonavailability of the double-lumen tube or expertise.
•Double-lumen endotracheal tube can be helpful to isolate and ventilate the lungs separately if the bleeding is lateralized. The double-lumen tubes are, however, easily obstructed by clots and do not permit passage of bronchoscopes of adequate size to allow bronchial toilet under unobstructed vision. It may still, however, be possible to confirm the tube position. Be careful as it can result in tube displacement.
Breathing:
•Large amount of blood in the tracheobronchial tree may be a major impediment to gas exchange. Maintain oxygen saturation above 94% by administering oxygen. Position the patient in lateral decubitus toward the site of bleeding as it spares the contralateral lung from aspiration.
Circulation:
•All patients should be admitted to the intensive care unit. Vital signs should be monitored continuously.
•The intra-arterial line should be inserted for continuous blood pressure monitoring.
•Two large-bore intravenous lines or a central venous catheter should be inserted and intravenous fluids should be started.
•If the condition is rapidly deteriorating, O-positive blood (O-negative in case of women of childbearing age) should be transfused while waiting for blood grouping and crossmatching. Meanwhile, determine the blood type, crossmatch, and request for red cell units, depending on the requirement. Assess the severity of volume loss (see Chap. 64).
Step 2: Clinical assessment and localization of bleeding site
•The first step in diagnosing hemoptysis is to determine the bleeding source: respiratory tract versus a nasopharyngeal or gastrointestinal source. Querying the patient identifies the correct source in 50% of cases.
•Hemoptysis is characterized by cough with frothy sputum, which is alkaline when tested with litmus paper. In contrast, hematemesis is accompanied by nausea and vomiting, and is frequently acidic. Epistaxis is usually traumatic and may be localized by anterior rhinoscopy and examination of the oropharynx. Aspirated blood or swallowed blood from any of the sites can make it difficult to initially identify the origin of bleeding.
Step 3: Find out the etiology
Take a detailed history and perform physical examination, keeping in mind the various causes of severe hemoptysis (Table 8.1).
Physical examination: The amount, color, and character of bleeding should be noted. On examination, look for specific signs that can point to a specific diagnosis as mentioned in Table 8.2.
8 Massive Hemoptysis |
67 |
|
|
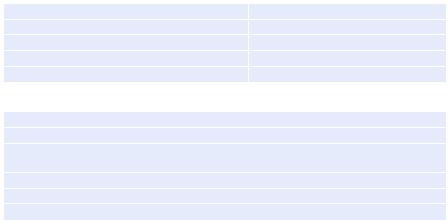
Table 8.1 Causes of severe hemoptysis |
|
Bronchiectasis |
Pulmonary tuberculosis |
Fungal infections in cavities—aspergilloma |
Bronchogenic carcinoma |
Severe mitral stenosis |
Coagulopathies |
Foreign bodies |
Trauma |
Vasculitis |
Pulmonary embolism |
Table 8.2 Focused physical examination |
|
Digital clubbing—bronchiectasis or lung carcinoma |
|
Stridor—tracheal tumors or a foreign body |
|
Oral and aphthous ulcers, genital ulcers, and uveitis—Behcet’s disease in which pulmonary arteriovenous malformations (AVM) are responsible for hemoptysis
Cutaneous purpura or ecchymosis—coagulation disorders
Diastolic murmur—mitral stenosis
Saddle nose with rhinitis and septal perforation—Wegener’s granulomatosis
Step 4: Plan investigations
The following investigations should be ordered in all patients:
•Hemoglobin, hematocrit, platelets count, coagulation studies (prothrombin time including international normalized ratio, partial thromboplastin time).
•Renal function tests.
•Liver function tests.
•Arterial blood gas analysis.
•D-dimer, urinalysis.
•Chest skiagram: Chest radiography helps in localizing the bleeding source in 60% of cases and identifying possible etiology such as a lung mass, cavitary lesion, or alveolar hemorrhage.
•Further investigations will depend on the possible diagnosis.
•Sputum/bronchoalveolar lavage should be tested for bacteria including mycobacteria, fungi, and malignant cells.
•Multidetector computed tomography (MDCT) has proved to be of considerable diagnostic value in localizing the site of bleeding. Contrast-enhanced MDCT produces high-resolution angiographic studies with a combination of multiplanar reformatted images. Therefore, MDCT angiography is able to identify the source of bleeding and underlying pathology with high sensitivity. This is of particular importance to the interventional radiologist planning for arterial embolization.
•If MDCT is not available, contrast-enhanced single-detector spiral CT can be performed to detect bronchial and nonbronchial systemic arterial vascular lesions such as thoracic aneurysm and AV malformation. Except for life-threatening situations, thoracic CT scans should be performed prior to bronchoscopy.
Step 5: Bronchoscopy
•Diagnostic bronchoscopy is the primary method for diagnosis and localization of hemoptysis. Rigid bronchoscopy is ideally recommended in cases of massive hemoptysis because of its ability to maintain airway patency.
68 |
A. Bansal and V. Kantroo |
|
|
•Flexible bronchoscopy (FOB) is used more widely, considering the ease of performance at the patient’s bedside without the use of general anesthetic and operating theatre suite. Vasoactive drugs can be instilled directly into the bleeding source. The overall diagnostic accuracy of bronchoscopy in localizing the site of bleeding is 50%, but it is less useful in identifying the underlying cause. Further disadvantages include nonvisualization during active hemoptysis, and ineffectiveness of endobronchial therapies in most cases. The ideal time for bronchoscopy is controversial, but the consensus is to perform urgent bronchoscopy in patients with massive hemoptysis.
•In case plug of blood clot is seen in a segment, it is recommended not to remove it as it may restart massive hemoptysis.
•Administer local therapy: The following therapeutic measures can be tried through the fiber bronchoscope to control bleeding.
–Iced saline bronchial lavage in the involved lung
–Iced saline lavage of up to 1,000 mL in 50 mL aliquots at the bleeding site
–Administration of topical hemostatic agents, such as epinephrine (1:20,000) or thrombin-fibrinogen
–Tamponade therapy, using oxidized regenerated cellulose mesh
•Another alternative site-specific therapy that can be tried using the flexible bronchoscope includes endobronchial tamponade using a balloon tamponade catheter to prevent aspiration to the unaffected contralateral lung and preserve gas exchange.
•A bronchus-blocking balloon catheter has been designed to be used through the working channel of the flexible bronchoscope which has a second channel that is used to instill vasoactive hemostatic agents, such as iced saline, epinephrine, vasopressin, or thrombin-fibrinogen, to control bleeding.
Step 6: Start pharmacotherapy
•Antibiotics and steroids, depending on the underlying condition, are necessary to control the precipitating cause.
•Intravenous vasopressin has not been shown to improve the outcome, and therapies such as vitamin K supplements and tranexamic acid have a doubtful role.
•Correct coagulation abnormalities with appropriate platelet, fresh frozen plasma, and cryoprecipitate.
•Recombinant activated factor VII (rFVIIa) can be tried as it has been reported as an effective temporizing measure in unstable patients with hemoptysis due to community-acquired pneumonia, when conventional treatment is not immediately available in the setting of a regional hospital.
Step 7: Bronchial artery embolization (BAE)
•Bronchial artery angiography is highly effective in localizing the source of bleeding and identifying a vessel for embolization. The bronchial circulation (a high-pressure circuit with systolic pressure of 120 mmHg) is the most common source of massive hemoptysis, accounting for 95% of all cases. Less than 5% of
8 Massive Hemoptysis |
69 |
|
|
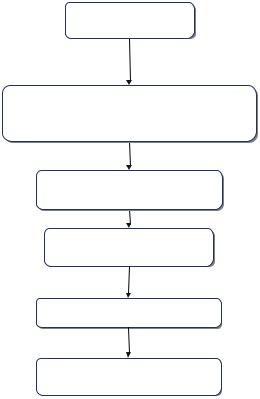
Fig. 8.1 The management of severe hemoptysis
Patient with massive hemoptysis
Initial resuscitation
If required intubation with single-or double-lumen endotracheal tube
Clinical assessment and localization of the site of bleeding
Plan investigations and continue supportive treatment
MDCT and bronchoscopy
Bronchial arterial embolization and/or surgery
bleeding arises from the pulmonary circulation (a low-pressure circuit with a systolic pressure of 15–20 mmHg).
•Once the bleeding bronchial artery is located, particles (polyvinyl alcohol foam, absorbable gelatin, pledgets of Gianturco steel coils) are infused into the artery. BAE achieves immediate control of the bleeding in 75–90% of cases. Postembolization recurrence of hemoptysis has been observed in 20% of cases.
•Remember that this is a temporizing procedure while every effort is being made to make a clear diagnosis and treat accordingly, except in AV malformations in which this could be the definitive treatment.
•If bronchial artery angiography does not reveal a bleeding vessel, a pulmonary angiogram is required to investigate the pulmonary circulation.
Step 8: Surgical resection (segmentectomy, lobectomy, and pneumonectomy)
Surgery is indicated in the following conditions:
•BAE is unavailable or technically unfeasible, or bleeding or aspiration of blood continues despite embolization.
