
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index

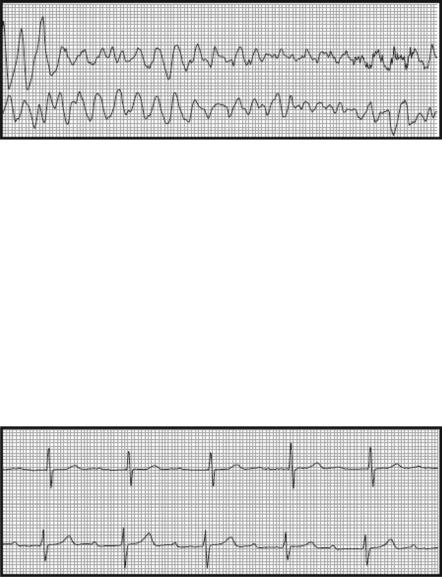
Cardiac Arrhythmias |
22 |
|
Shyam Sunder Tipparaju and Gopinath Ramachandran
A 40-year-old hypertensive diabetic male patient was admitted with the history of dizziness and a sensation of passing out. He had no significant past medical history. On examination he was alert and oriented, with well-perfused extremities, pulse rate of 130/min irregular, BP of 120/70 mmHg (usual BP 150/90 mmHg), and soft systolic murmur on cardiac auscultation.
Cardiac arrhythmias are caused by disorders of impulse formation or disorders of impulse conduction, or both. Arrhythmias in the ICU pose a diagnostic and therapeutic challenge. A systematic approach to interpretation of electrocardiogram, identifying urgency of management, and proper consultation when required is needed for an optimum outcome.
Step 1: Start resuscitation
•Establish an intravenous (IV) access as these patients may deteriorate suddenly.
•In cardiac arrest situations, follow the advanced cardiac life support (ACLS) protocol (see Chap. 19).
Step 2: Urgently cardiovert the hemodynamically unstable patient if indicated (see Chap. 94)
•If the patient is in shock or in severe respiratory distress with atrial or ventricular tachyarrhythmia, immediate synchronized cardioversion is attempted.
S.S. Tipparaju, M.D., P.D.C.C. (*)
Critical Care, Continental Hospitals, Hyderabad, India e-mail: shyamsundert@rediffmail.com
G. Ramachandran, M.D., F.F.A.R.C.S.
Department of Anaesthesiology & Critical Care, Nizam Institute of Medical Sciences, Hyderabad, India
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
173 |
DOI 10.1007/978-81-322-0535-7_22, © Springer India 2012 |
|
174 |
S.S. Tipparaju and G. Ramachandran |
|
|
•In the conscious patient, IV midazolam should be judiciously used in aliquots of 1–2 mg prior to cardioversion.
Step 3: Urgently insert temporary transvenous pacemaker if indicated (see Chap. 95)
•In patients with symptomatic bradycardia not responding to atropine, transvenous pacemaker should be inserted.
•Temporizing measure with the transcutaneous pacemaker may be tried.
Step 4: Take focused history
•Cardiorespiratory symptoms
•Low-output state symptoms such as fatigue, dizziness, syncope, and oliguria
•Past history of cardiac disorders
•History of hypertension, diabetes, hyperlipidemia, or systemic diseases such as thyrotoxicosis
•Alcohol, nicotine, or other substance abuse
•Drug history—antiarrhythmic and antihypertensive
Step 5: Perform focused physical examination
•General physical examination to look for thyroid enlargement, tremor, anemia, pedal edema, and low perfusion state
•Cardiovascular system:
–Listen for gallop rhythm or murmur
–Palpate all peripheral and central pulses
–Take blood pressure in both arms
•Other system examination
Step 6: Send basic investigation
•Complete blood count—anemia
•Trop T/I—raised in myocardial infarction
•Electrolytes (Na, K, Mg, Ca, PO4)
•Arterial blood gas (ABG)—acid–base disorders
•Renal and liver function test
•Echocardiogram—left ventricular function, left atrial size and clot, and valvular disorders
•Chest X-ray—cardiomegaly and the left atrial enlargement
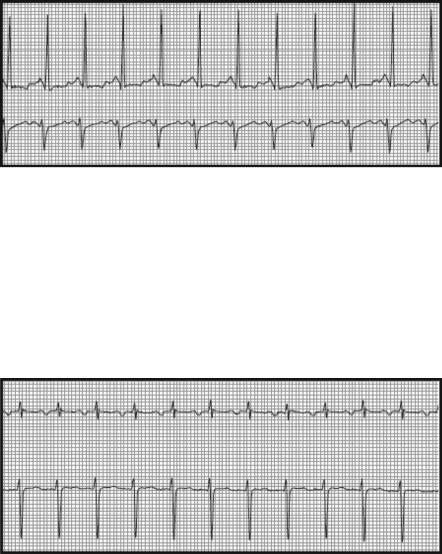
Step 7: Analyze 12-lead electrocardiogram (ECG) (Fig. 22.1)
•Systematically analyze 12-lead ECG.
•Any previous ECG if available should be compared with the present.
•Check the name and the date.
• Check calibration (1 mV deflection for two large squares = 10 mm).
•Check the speed of tracing (25 mm/s).
•Check the correct limb lead placement—P wave inverted in aVR.

22 Cardiac Arrhythmias |
|
175 |
2/S |
.04/S |
1/S |
(1000 m second) |
||
(200 m second) |
(40 m second) |
Paper speed: 25 mm/second |
|
|
|
1 mv |
PR |
QT |
|
Interval |
Interval |
5 mm |
|
R |
|
|
T
1 mv |
P |
J Point |
U |
Q
S
QRS
Duration
Fig. 22.1 Electrocardiogram
Step 8: Calculate the ventricular rate
•One small square = 0.04 s.
•One large square = 0.2 s.
•Measure R–R interval.
•Count the number of small squares in R–R interval and divide into 1,500.
•Or count the number of large squares in R–R interval and divide into 300.
•Or for each big square in R–R interval decremental heart rate of 300, 150, 100, 75, 60, 50 (e.g., for one big square in between R–R interval, heart rate is 300; for two big squares, it is 150; and so on).
•If irregular cardiac rhythm, count the number of beats in 6 s (two 3-s intervals) and multiply by 10.
•Bradycardia is less than 60/min.
•Tachycardia is more than 100/min.
Step 9: Analyze ventricular rhythm
•Check Lead II rhythm strip.
•Check RR interval for regularity.
176 |
S.S. Tipparaju and G. Ramachandran |
|
|
•Mark two consecutive R waves and match the distance with subsequent RR intervals to check for regularity of cardiac rhythm.
Step 10: Identify P waves
•Absent P waves suggest atrial fibrillation, ventricular tachycardia, or rhythms originating from the AV node.
•Look for flutter waves.
Step 11: Examine QRS complex, normal or wide (normal less than 0.08 s)
•Normal—rhythm originates from the AV node or above.
•Wide—rhythm usually originates infranodal or supranodal with aberrant AV conduction.
Step 12: Find out the relationship between the P waves and QRS complexes
•More P waves than QRS complexes
–Secondor third-degree AV block
•More QRS complexes than P waves
–Accelerated junctional rhythm
–Ventricular tachycardia
Step 13: Describe arrhythmias based on
•Rate (bradycardia or tachycardia)
•Rhythm (regular or irregular)
•Origin of impulse (supraventricular, ventricular, or artificial pacemaker)
•Intraventricular conduction (narrow or wide-complex QRS)
Step 14: Investigate and treat the underlying disease
•Clinically, significant tachyor bradyarrhythmias are a reflection of the underlying cardiac disease—ischemic, hypertensive, valvular, or infective—which should be managed concurrently.
•Systemic diseases such as thyroid disorders, electrolyte imbalance, or drugs can also cause significant arrhythmias and should be managed.
•Look for preexcitation syndrome (Wolff–Parkinson–White [WPW] syndrome).
Step 15: Identify and manage precipitating cause
•Precipitating factors, such as fever, acidosis, drugs and alcohol intoxication, should be sought for and managed in all cases of clinically significant arrhythmias.
Step 16: Analyze and manage narrow complex, regular tachycardias
•Sinus tachycardia
–Rate is usually less than 150/min. Maximum sinus heart rate is age-dependent (220 age in years).
–P wave morphology is normal and precedes each QRS complex.
–Treat the underlying cause such as pain, fever, anxiety, hypovolemia, and hypoxia.
22 Cardiac Arrhythmias |
177 |
|
|
•Paroxysmal supraventricular tachycardia
–Ventricular rate 150–250/min
–P waves absent or after QRS.
–Abrupt onset and offset.
–Try vagal maneuvers such as carotid massage and Valsalva to terminate tachycardia.
–Intravenous adenosine 6 mg IV bolus; if ineffective, 12 mg IV bolus twice.
–AV nodal blocking agents like calcium channel blockers, beta-blockers, and digoxin may be tried.
–In patients with WPW syndrome, avoid AV nodal blocker. Cardioversion or amiodarone is preferable.
•Atrial flutter
–Atrial rate usually 300/min, sawtooth pattern.
–Ventricular rate 150 (due to 2:1 conduction).
–Cardiovert if unstable.
–For rate control, AV nodal blocking agents (diltiazem, verapamil, metoprolol, digoxin), amiodarone, or procainamide.
–In patients with ejection fraction of less than 40%, consider digoxin or amiodarone.
178 |
S.S. Tipparaju and G. Ramachandran |
|
|
–For rhythm control, amiodarone, procainamide, ibutilide, flecainide, and propafenone.
–Avoid rhythm control if arrhythmia persists for more than 48 h as conversion to sinus rhythm may cause embolization.
–In WPW syndrome, avoid the AV nodal blocking agent. Consider amiodarone, sotalol, procainamide, flecainide, or propafenone.
–Anticoagulate if arrhythmia persists for more than 48 h or echo shows left atrial clot.
•Ectopic atrial tachycardia
–Rate more than150/min.
–Altered P wave axis.
–P wave precedes each QRS.
–Use AV nodal blocking agents.
Step 17: Analyze and manage narrow complex irregular tachycardia
•Atrial fibrillation
–Absent P waves.
–Ventricular rate variable.
–Manage like atrial flutter (see above).
–Special attention should be given for anticoagulation.
22 Cardiac Arrhythmias |
179 |
|
|
•Multifocal atrial tachycardia (MAT)
–Varying P wave morphology of three or more in the same lead.
–Seen with digitalis toxicity, theophylline toxicity, severe cardiopulmonary disease.
–Treatment is to manage the underlying disease.
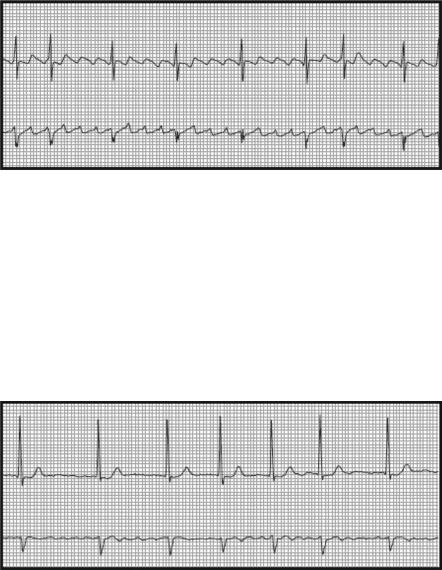
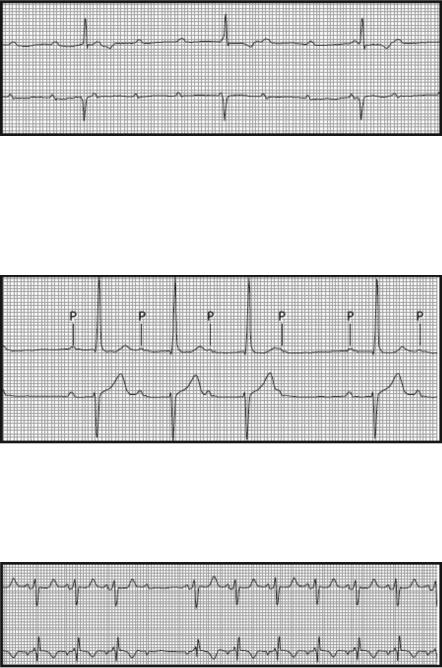
Step 18: Analyze and manage wide-complex regular tachycardia
•Monomorphic ventricular tachycardia
–Ventricular rate 100–200/min
–QRS wide (>0.12 s)
–Nonsustained ventricular tachycardia (NSVT) lasts less than 30 s and carries a better prognosis and usually requires only observation without any intervention.
–Sustained ventricular tachycardia (VT) lasts for more than 30 s and usually requires treatment.
–Symptomatic VT with detectable pulse should be managed with urgent synchronized cardioversion.
–In the hemodynamically stable patient, consider amiodarone, lidocaine, or procainamide.
–For pulseless VT, follow the ACLS protocol (see Chap. 19).
180 |
S.S. Tipparaju and G. Ramachandran |
|
|
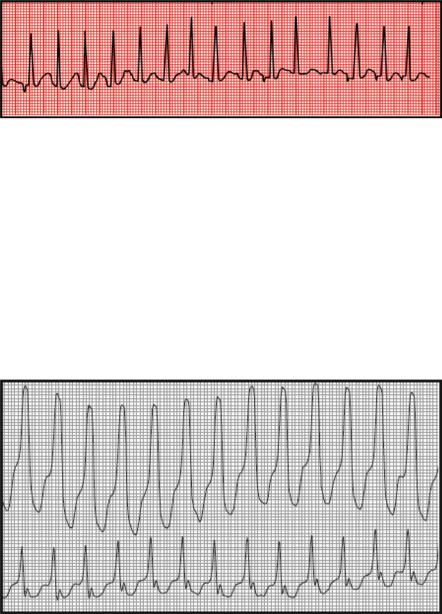
•Polymorphic ventricular tachycardia
–Variable QRS morphology.
–It usually occurs in the setting of acute ischemia or infarction.
–It may be associated with prolonged QT interval (torsades de pointes) as may be seen with electrolyte disorders such as hypokalemia, hypomagnesemia, and drugs (tricyclic antidepressant, macrolide, fluoroquinolone), or it may be congenital.
–Torsades de pointes show twisting of QRS around the baseline in ECG.
–Polymorphic VT should be cardioverted asynchronously as they are usually unstable.
–If stable, manage like monomorphic VT (see above).
–For stable torsades de pointes, give 2 g IV magnesium sulfate.
–Withdraw causative drugs; correct the electrolyte abnormality.
–Torsades is sometimes bradycardia-dependent; isoproterenol infusion or temporary pacemaker may be tried to abort the rhythm.
•Supraventricular tachycardias with aberrant conduction
–Wide-complex tachycardias should be assumed to be VT unless proven otherwise and treated accordingly.
–As all unstable patients require immediate cardioversion, this distinction is academic in such situation.
–Consider VT than aberrant conduction in following ECG findings:
•Change in axis or morphology of QRS from the baseline ECG in sinus rhythm
•AV dissociation (P waves not associated with QRS)
•Beginning of R to the nadir of S wave greater than 0.1 s
•Lack of RS complex V1 till V6
•Fusion beats
•Capture beats
–Look for short PR with delta wave in sinus rhythm favoring WPW syndrome.
Step 19: Analyze and manage wide-complex irregular tachycardia
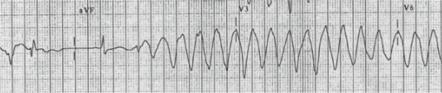
•Ventricular fibrillation
–Chaotic rhythm without any discernible QRS complex.
–Requires immediate defibrillation—follow ACLS protocol (see Chap. 19).
22 Cardiac Arrhythmias |
181 |
|
|
•Atrial fibrillation with aberrant conduction
– Approach is similar to regular tachycardias with aberrant conduction.
Step 20: Analyze narrow complex regular bradycardia
•Sinus bradycardia
–Rate less than 60/min
–May be secondary to a variety of underlying diseases like hypothyroidism, obstructive jaundice, increased intracranial pressure
–Usually asymptomatic and requires treatment of the underlying condition only
–May be associated with brady–tachy syndrome
•First-degree heart block
–Prolonged PR interval (>200 ms)
–Usually asymptomatic and do not require any specific treatment
–May progress to higher degrees of block in some cases, so should be monitored closely
•Third-degree heart block–AV nodal block
–Heart rate varies from 40 to 60 depending on the site of block.
–When the block occurs in the AV node, rate is 40–60 beats/min.
–The patient is usually stable.
182 |
S.S. Tipparaju and G. Ramachandran |
|
|
Step 21: Analyze narrow complex irregular bradycardia
•Second-degree AV block (Mobitz type 1—Wenckebach)
–Progressively prolonged PR followed by a nonconducted atrial beat.
–Escape ventricular rhythm is 40–60/min.
–Usually a hemodynamically stable rhythm.
–Commonly seen with inferior wall infarction and AV nodal blocking agents.
•Second-degree AV block (Mobitz type II)
–Fixed PR interval with one or more nonconducting beats.
–More likely to progress to complete heart block.
–Escape ventricular rate is 25–40/min.
–Unstable rhythm; usually requires treatment.
•Atrial fibrillation, MAT with high-degree AV block
–Usually due to toxicity of AV nodal blocking drugs which are used for rate control.
