
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index
93 Pulmonary Artery Catheterization |
|
|
|
751 |
|||
|
|
|
|
|
|||
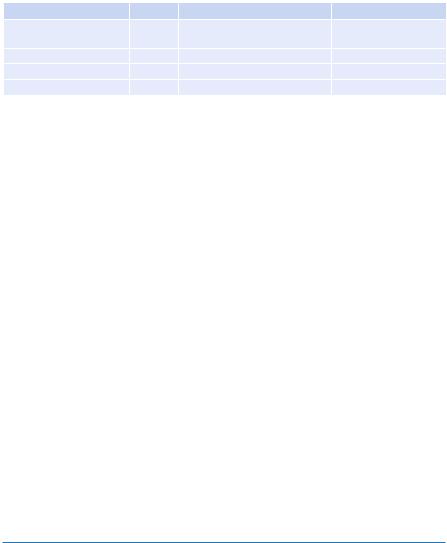
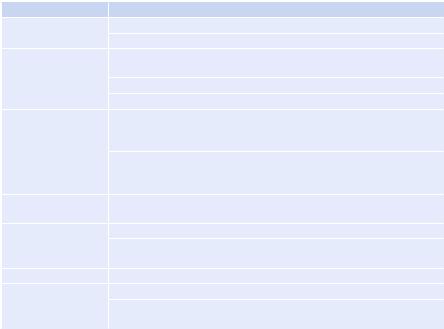
Table 93.4 Oxygen transport parameters |
|
|
|
|
|||
Parameter |
Symbol |
Formula |
|
|
|
Normal value |
|
Mixed venous oxygen |
SvO2 |
|
|
|
|
70–75% |
|
saturation |
|
|
|
|
|
|
|
Oxygen delivery |
DO |
2 |
1.34 × Hb × SaO |
× CO |
|
520–570 mL/min/m2 |
|
|
|
2 |
|
|
|
|
|
Oxygen uptake |
VO |
2 |
1.34 × Hb × (SaO |
− SvO |
) × CO |
110–160 mL/min/m2 |
|
|
|
|
2 |
2 |
|
|
|
Oxygen–extraction ratio |
O2ER |
VO2/DO2 |
|
|
|
20–30% |
|
Checklist to Follow Before PCWP Can Reliably Reßect the LV Filling Pressure
•The tip of the PAC should be in west zone 3 in the lung. The airway pressure fluctuations are minimum in this zone. On the chest X-ray, the tip of the PAC should be below the level of the left atrium within 2 cm of cardiac silhouette.
•Correct pulmonary artery and wedge pressure waveforms: Pulmonary artery pressure upstroke slightly precedes the radial artery pressure upstroke.
•Rule out abnormal waveforms: There should be no air, clots, or motion-related artifacts (distinguished from normal by their shape and timing). If the balloon is overinflated and occludes the lumen orifice or forces the catheter tip against the vessel wall—or if there is distal catheter migration—overwedging may result. Overwedged pressure is devoid of pulsatility and is higher than expected.
•Measure the pressures only at end expiration. This is because end-expiratory pressure is closest to the atmospheric pressure. This is done by freezing the waveform on the monitor and observing the movement of the trace up or down along with the phases of respiration or on a paper printout.
•Wedge pressure will underestimate the left ventricular end-diastolic pressure if the patient has diastolic dysfunction, aortic regurgitation, pulmonary regurgitation, right bundle branch block, or postpneumonectomy.
•Wedge pressure will overestimate the left ventricular end-diastolic pressure if the patient has pulmonary arterial hypertension, pulmonary veno-occlusive disease, tachycardia, mitral stenosis, or mitral regurgitation.
•Always remember that wedge pressure is a reflection of LV end-diastolic pressure, whereas it is the end-diastolic volume that determines preload. The two measurements may not correlate in up to 58% of measurements.
Suggested Reading
1.Friese RS, Shafi S, Gentilello LM. Pulmonary artery catheter use is associated with reduced mortality in severely injured patients: A National Trauma Data Bank analysis of 53,312 patients. Crit Care Med. 2006;34:1597–601.
Patients aged 61Ð90 years, with arrival base deÞcit worse than −11 and injury severity score of 25Ð75, were found to have a decrease in the risk of death with PAC use.
2.Chittock DR, Dhingra VK, Ronco JJ, et al. Severity of illness and risk of death associated with pulmonary artery catheter use. Crit Care Med. 2004;32:911–5.
In critically ill adult patients, logistic regression analysis demonstrated no increased risk of death associated with exposure to the pulmonary artery catheter in the population as a whole.

752 |
R. Chawla et al. |
|
|
3.American Society of Anesthesiologists Task Force on Pulmonary Artery Catheterization. Practice guidelines for pulmonary artery catheterization: an updated report by the American Society of Anesthesiologists Task Force on Pulmonary Artery Catheterization. Anesthesiology. 2003;99:988–1014.
A detailed review of the various aspects of the use of the pulmonary artery catheter along with recommendations and practice guidelines on its management and use.
4.Connors AF Jr, Speroff T, Dawson NV et al. The effectiveness of right heart catheterization in the initial care of critically ill patients. SUPPORT Investigators. JAMA. 1996;276(11):889–97.
PAC use was associated with increased mortality and increased utilization of resources. Subgroup analysis did not reveal any patient group or site for which the PAC was associated with improved outcomes. This study started the outcome controversies on PAC use.
5.Swan HJC, Ganz W, Forrester JS, Marcus H, Diamond G, Chonette D. Catheterization of the heart in man with use of a flow-directed balloon-tipped catheter. N Engl J Med. 1970;283:447–51.
The landmark article that completely changed the way people monitored patients in the ICUs. Since its introduction the catheter has hardly undergone change in size or structure. It was at one time the most widely used equipment in the ICU.
Website
1.www.pacep.org
A free online multiorganization effort to provide educational tools for the use of the pulmonary artery catheter in clinical practice

Defibrillation and Cardioversion |
94 |
|
|
Rajesh Chawla and Sananta K. Dash |
|
A 70-year-old diabetic, hypertensive, and coronary artery disease male patient was admitted to the hospital with acute myocardial infarction. His pulse was 120/min, and blood pressure was 100/60 mmHg. He was on dopamine and dobutamine infusion. He was being prepared for primary angioplasty. While being shifted to the catheterization laboratory, he collapsed. The cardiac monitor showed ventricular fibrillation (VF).
Electrical shock therapies are capable of terminating arrhythmias due to reentry. Reentry is the predominant mechanism of majorities of arrhythmias in ICUs.
Step 1: Be familiar with the device
1.Types of Defibrillators
A. Manual external defibrillators
•These defibrillators have electrocardiogram (ECG) readers, which the health care provider uses to diagnose a cardiac rhythm. The health care provider will then decide what charge (in joules) to use, based on proven guidelines (ACLS) and experience, and will deliver the shock through paddles or pads on the patient’s chest.
•As they require detailed medical knowledge, these units are generally only found in hospitals and on some ambulances.
R. Chawla, M.D., F.C.C.M. (*)
Department of Respiratory, Critical Care & Sleep Medicine, Indraprastha Apollo Hospitals, New Delhi, India
e-mail: drchawla@hotmail.com
S.K. Dash, M.D.
Department of Respiratory & Critical Care Medicine, Indraprastha Apollo Hospitals, New Delhi, India
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
753 |
DOI 10.1007/978-81-322-0535-7_94, © Springer India 2012 |
|
754 |
R. Chawla and S.K. Dash |
|
|
B.Automated external defibrillators (AEDs)
•AEDs are sophisticated, reliable computerized devices that use voice and visual prompt to guide lay users and health care providers to safely defibrillate the appropriate rhythm.
•They are not designed to deliver synchronized shock (i.e., cardioversion of ventricular tachycardia (VT) with pulse). They will rather recommend a nonsynchronized shock for both monomorphic and polymorphic VTs if the rate and morphology exceed the preset value.
•The AEDs take time (~10–20 s) to diagnose the rhythm. On the other hand, a professional can diagnose and treat the condition far more quickly with a manual unit. This valuable time gap between analysis and application of shock, where the chest compression has to be withheld, is unavoidable for the AEDs.
•These time intervals for analysis, which require stopping of chest compressions, have been shown in a number of studies to have a significant negative effect on shock success. This effect led to the change in the AHA defibrillation guideline (calling for 2 min of cardiopulmonary resuscitation (CPR) after each shock without analyzing the cardiac rhythm), and some recommend that AEDs should not be used when manual defibrillators and trained operators are available.
•There are two types of AEDs: fully automated and semiautomated. Most AEDs are semiautomated. A semiautomated AED automatically diagnoses heart rhythms and determines if a shock is necessary. If a shock is advised, the user must then push a button to administer the shock.
•A fully automated AED automatically diagnoses the heart rhythm and advises the user to stand back while the shock is automatically given. Also, some types of AEDs come with advanced features, such as a manual override or an ECG display.
C.Implantable cardioverter defibrillators (ICD)
ICDs analyze the rhythm based on an internal program and shocks appropriately.
2.Types of Shocks
A.Monophasic
A monophasic shock delivers current in one polarity and is classified again according to the rate at which the current pulse decreases to 0.
B.Biphasic shocks
•A biphasic shock delivers current that reverses course during the pulse.
•Defibrillation with biphasic waveform improves short-term outcome of terminating VF.
•It is safe and has equivalent or higher efficacy in terminating VF than the monophasic.
•Recommendation is 120–200 J according to manufacturer’s recommendation. If not known, then defibrillate at the maximum dose.
94 Defibrillation and Cardioversion |
755 |
|
|
|
|
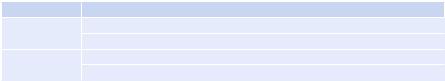
Table 94.1 Indication of cardioversion and defibrillation |
|
|
Type |
Indications |
|
Immediate |
Hemodynamic instability due to tachyarrhythmia of shockable variety |
|
|
Congestive heart failure and angina due to shockable tachyarrhythmia |
|
Elective |
Hemodynamically stable |
|
|
No significant symptoms |
|
Caution: Patients with digitalis toxicity, electrolyte imbalance (more prone to ventricular fibrillation (VF) and ventricular tachycardia (VT) after shock), chronic atrial fibrillation (AF), and atrial flutter (AFL) of more than 48 h who are not adequately anticoagulated
3.The Modes (Defibrillation and Cardioversion)
A.Defibrillation
Defibrillation is a method of introduction of unsynchronized electrical shock that stuns the heart briefly and terminates all electrical activities including VF and rapid VT, and if the heart is still viable then its pacemakers will eventually resume its normal rhythm, which ultimately results in a perfusing rhythm. It is not synchronized with the R wave in ECG.
B.Cardioversion
Here, the shock delivery is synchronized with QRS complexes. It prevents shock delivery during the relative refractory portion of the cardiac cycle (i.e., ventricular vulnerable period, between 60 and 80 ms before and 20–30 ms after peak of the T wave) when shock could produce VF.
4.Electrodes
A.Types
•Handheld paddles (pediatric and adult)
•Self-adhesive pads (pediatric and adult)
B.Size
•8–12 cm for the adult and child (³8 years)
Step 2: Assess the need for cardioversion and defibrillation—indications and contraindications (Tables 94.1, 94.2 and 94.3)
Step 3.1: Method for cardioversion
A.Patient preparation for elective cardioversion
•It should be done in hospital areas equipped with cardiac monitoring, airway management, and cardiopulmonary resuscitation.
•Ensure nil by mouth (NBM) status.
•Patient counseling is required in detail about the procedure.
•Obtain valid informed consent from the patient or legal surrogate.
•Confirm adequacy of anticoagulation in chronic AF.
•If digoxin is given, measure the serum level.
•Consider starting antiarrhythmics 24–48 h preprocedure.
•Preand postprocedure ECG.
756 |
|
R. Chawla and S.K. Dash |
|
|
|
||
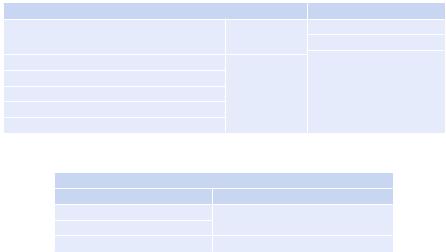
Table 94.2 Tachyarrhythmias responsive to electrical therapy |
|
||
Responsive to cardioversion |
|
Responsive to defibrillation |
|
Supraventricular |
Ventricular |
Pulseless VT |
|
|
|
VF |
|
Atrial fibrillation |
Monomorphic |
Unstable polymorphic VT |
|
with or without pulse |
|||
Atrial flutter |
VT with pulse |
||
|
|||
Sinoatrial nodal reentrant tachycardia |
|
|
|
Atrioventricular nodal reentrant tachycardia |
|
|
|
Atrioventricular reciprocating tachycardia |
|
|
|
Table 94.3 Tachyarrhythmias unresponsive to electrical therapy |
|||
Unresponsive to cardioversion/defibrillation |
|
||
Supraventricular |
Ventricular |
|
|
Sinus tachycardia |
Idiopathic monomorphic VT |
||
Focal atrial tachycardia |
|
|
|
Junctional tachycardia |
Accelerated idioventricular rhythm |
||
B.Preprocedural sedation protocol
•If the patient requires oxygen or is currently receiving oxygen, the delivery of oxygen should be directed away from the chest.
•Continuous monitoring—ECG, SPO2, and noninvasive blood pressure (NIBP).
•Give sedation and analgesia.
–Agents—propofol, midazolam, and etomidate
–Propofol is the best option for its early awakening time and better safety profile. Short-acting agents are preferred.
–Opioid analgesics, such as fentanyl, are used for analgesia.
•Conscious sedation
–Goal—maintain consciousness but in a somnolent state. It can be done by a trained physician without anesthesiologist’s supervision. Midazolam is the preferred agent here.
C.Turn the defibrillator on (monophasic or biphasic shock) It simultaneously switches the monitor on.
D.Suggested electrode position
1. Anterolateral (most common): An anterior paddle is placed in right infraclavicular area, and the lateral paddle is placed lateral to the left breast in longitudinal alignment.
2. Anteroposterior: The anterior paddle is same as before, and the posterior paddle is on the left side of the spine at the level of lower end of the scapula.
• Other two positions include anterior-left infrascapular and anterior-right infrascapular. Anteroposterior placement is found to be more successful in cardioversion of AF with monophasic shock.
• Apply jelly (water-based conducting jelly). Place the negative electrode closer to the heart with both the electrodes adequately separated.
94 Defibrillation and Cardioversion |
|
757 |
|
|
|
|
|
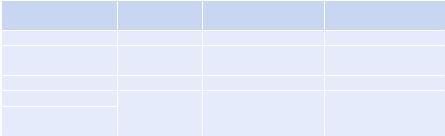
Table 94.4 Specific energy levels |
|
|
|
|
|
Monophasic (initial and |
|
Rhythm |
Mode |
consecutive shocks) |
Biphasic shock |
VF, pulseless VT |
Defibrillation |
360 |
120–200 |
Stable, monomorphic |
Cardioversion |
100, 200, 300, 360 |
70, 120, 150, and 170a |
VT with pulse |
|
|
|
AF |
Cardioversion |
100–200, 300, 360 |
100–120 |
Atrial flutter, |
Cardioversion |
50, 100, 200, 300, 360 |
70, 120, 150, and 170a |
Supravetricular |
|
(MDS) |
|
tachycardia (SVT) |
|
|
|
aThe biphasic waveform using the lower energy level is acceptable if documented to be clinically equivalent or superior to reports of monophasic shock success. Initial biphasic dose of 100–200 J with escalation depending on the need is recommended (evidence extrapolated from cardioversion of atrial fibrillation). For specific recommendation consultation from the device, manufacturer is advised
•The conducting jelly should be restricted to the pad area and should not be spread all over the chest.
E.Synchronization (for synchronized cardioversion)
•The device should be in the synchronized mode as most AEDs have a default unsynchronized mode.
•For each subsequent defibrillation, one needs to reset to synchronized mode. Confirm synchronization by looking at markers on the R wave. It may be necessary to adjust the gain of the monitor to remark the R wave correctly.
F.Announce “charging-stand clear”
G.Charge
Press the charge button (present on the paddle as well as on the monitor) to select the level of charge (Table 94.4). Hear the audible sound/alarm when charging is completed.
H.Clearing
Say “I am going to shock on three; one, I am clear; two, you are clear; three, everybody is clear.” Check and look around after each step and confirm safety.
I.Shock
Check to see the synchronized mode prior to giving a synchronized shock.
Step 3.2: Method for defibrillation
A.Analyze the rhythm
A bedside cardiac monitor or ECG display of the defibrillator is needed, if already attached.
B.Sedation protocol
As most often patients with pulseless VT and VF present in an emergent condition with unstable hemodynamics and impending cardiac arrest, sedation in such cases is not required.
C.Turn the defibrillator on
In most defibrillators, the default mode is the asynchronized mode.
D.Same as step D for cardioversion
758 |
R. Chawla and S.K. Dash |
|
|
Table 94.5 Complications and their prevention/treatment |
|
Complications |
Prevention/treatment |
Thermal burns |
The lowest accepted energy level |
|
Biphasic shock requires less energy |
Thromboembolism |
More common with AF (incidence in 1–7% patients who are not |
|
receiving anticoagulation) |
|
Ensure adequate anticoagulation |
|
Exclude left atrial clots with transesophageal echocardiography |
Arrhythmia |
For expected sinus bradycardia and sinus arrest, prophylactic placement |
|
of the pacemaker (transvenous/transcutaneous) in patients with AF with |
|
slow ventricular rate |
|
VT and VF—in patients with digitalis toxicity or hypokalemia, better to |
|
avoid cardioversion; if necessary to perform, then be prepared for a |
|
more refractory ventricular arrhythmia |
Myocardial damage |
Clinically insignificant but recommended to give two shocks at least |
|
1 min apart |
Loss of airway |
Mostly sedation related |
|
Complications such as aspiration can be reduced by ensuring nil by |
|
mouth (in elective cases), supervised cardioversion preferable |
Pulmonary edema |
Supportive measures and gradual improvement expected |
Fire hazard |
Reported when shock is given in an oxygen-rich environment |
|
Avoid direct blowing of oxygen across the chest in the oxygen-rich |
|
environment |
E.No need for synchronization
F.Same as cardioversion up to step H
G.Shock (asynchronized)
H.Post-shock
Resume CPR for five cycles, check rhythm, and proceed according to ACLS guidelines.
Step 4: Manage complications (Table 94.5)
Step 5: Special circumstances
A.Anticoagulation for reverting atrial fibrillation and flutter
•Anticoagulation is indicated in atrial fibrillation and flutter lasting more than 48–72 h.
•Recommendation is 3–4 weeks of anticoagulation prior to attempt cardioversion. It should be continued for at least 4 weeks post-cardioversion.
•This approach has an inherent risk of increased bleeding. So, in patients at the higher risk of bleeding, transesophageal echocardiography can be performed to exclude intracardiac thrombus and proceed with cardioversion without adequate prior anticoagulation. In any case, at least 4 weeks of anticoagulation is mandatory in post-cardioversion period.
