
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index

72 Heat Stroke and Hypothermia |
577 |
|
|
•Hypotension: To sustain organ perfusion, maintain mean arterial pressure of more than 65 mmHg by fluid administration, consider vasopressors, and monitor central venous pressure.
•Seizures should be controlled by IV benzodiazepines and barbiturates.
•Multiorgan failure: Give supportive therapy until organ function recovers. Stepwise management of hyperthermia is shown in Fig. 72.1.
Step 7: Prevention
•Hyperthermia, caused by physical exertion or hot environment, can be prevented by taking frequent rest breaks and staying hydrated.
•Genetic testing for known mutations of the SKM ryanodine receptor in conjunction with in vitro muscle contracture test can be used to evaluate individual susceptibility in patients from families with a history of malignant hyperthermia.
72.2Hypothermia
An 82-year-old man, a known case of Alzheimer’s disease and hypothyroidism, was found unresponsive on his backyard lawns. He had been taking aspirin, olanzapine, and levothyroxine for the past 3 years. Examination revealed femoral pulse 35/min, blood pressure (BP) unrecordable, Glasgow Coma Scale 3, and temperature 28°C.
Step 1: Initiate resuscitation
Initiate resuscitation as mentioned in Chap. 78:
•The management should start with removal of wet clothing if any and replacing it with warm, dry sheet.
•In severe hypothermia, if indicated, the patient is intubated gently and ventilated with warmed humidified O2 while closely monitoring cardiac rhythm.
•One should be prepared to treat ventricular fibrillation with DC shock (200 J) and cardiopulmonary resuscitation.
•Start IV line and infuse normal saline at 43°C.
Step 2: Diagnose types and severity of hypothermia
Primary
•Normal thermoregulation
•Overwhelming cold exposure
578 |
J. Dureja and H. Singh |
|
|
Table 72.1 Severity of hypothermia |
|
Mild (34–36°C) |
Shivering, amnesia/dysarthria, loss of coordination, tachycardia, |
|
tachypnea, normal BP |
Moderate (30–34°C) |
Absent shivering, bradycardia/atrial fibrillation, ↓ BP, ↓ respiratory |
|
rate, and stupor |
Severe (<30°C) |
Coma, absent corneal and oculocephalic reflexes, ↓↓ BP, ventricular |
|
fibrillation, apnea, areflexia, dilated and fixed pupils, flat EEG, |
|
asystole |
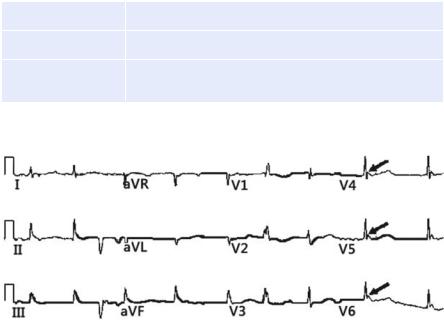
Fig. 72.2 Osborn (J) waves (Marked with arrows)
Secondary
•Abnormal thermogenesis
•Multiple causes (hypothyroidism, burns, hypothalamic abnormalities, sepsis) Hypothermia is defined as temperature less than 36°C.
Severity of hypothermia with presentation is described in Table 72.1.
•ECG may show Osborn (J) waves especially when temperature is less than 33°C (Fig. 72.2).
•It is a positive deflection, and its amplitude is proportional to the degree of hypothermia, usually seen in leads V3–V6 at junction of QRS and ST segment.
Step 3: Manage hypothermia
The patient should be warmed by the following rewarming methods: passive, active external, and active internal.
•Passive rewarming: It allows endogenous heat production to increase the core temperature, but heat conserving mechanisms must be intact (e.g., shivering, metabolic rate, and sympathetic nervous system).
72 Heat Stroke and Hypothermia |
579 |
|
|
It also includes decreasing heat loss by removal from cold environment, removing wet clothes, and providing the blanket. Passive warming increases body temperature by 0.5–2.0°C/h. It is the rewarming method of choice for mild hypothermia and also adjuncts for moderate hypothermia.
•Active external: It transfers exogenous heat to the patient. It can be provided by heating blankets (fluid filled), air blankets, radiant warmers, and immersion in hot bath, water bottles, and heating pads. It is less effective than internal rewarming if the patient is vasoconstricted.
The rewarming rate is 1–2.5°C/h. Although active external warming of extremities can lead to rewarming to some extent, the subsequent vasodilatation of the vessels in the extremities shunts cold blood to the core, resulting in an overall further decrease in body temperature. This paradoxical drop in core temperature is known as the after-drop phenomenon. Circulatory problem may be decreased by applying rewarming devices to trunk only.
Active internal warming: It is done by the following:
•Warm IV fluids
•Humid oxygen
•Peritoneal lavage
•Gastric/esophageal lavage
•Bladder/rectal lavage
•Pleural lavage
•Intermittent hemodialysis
•Extracorporeal circulatory rewarming
•Atrial arrhythmias should be monitored without intervention, as the ventricular response is slow, and unless preexistent, most will convert spontaneously during rewarming. Preexisting ventricular ectopy may be suppressed by hypothermia and can reappear during rewarming. If available, bretylium tosylate, the class III ventricular antiarrhythmic, is the drug of choice.
•Electrolytes and thyroid profile should be assessed and corrected if required.
•Cardiopulmonary bypass is a method of choice used for rewarming patients with cardiac arrest and severe hypothermia. This strategy provides circulation, oxygenation, and ventilation while core body temperature is increased. If cardiopulmonary bypass facilities are not available, a combination of invasive rewarming methods should be used. Once spontaneous circulation is returned, passive or active external rewarming methods can be used. Basic life support should be continued until core temperature is more than 30°C. Cardioactive drugs and further defibrillation should be withheld until this temperature is reached.
Stepwise management of hypothermia is shown in Fig. 72.3.
If core body temperature does not respond to warming efforts, underlying infection or endocrine derangements must be considered.

580 |
J. Dureja and H. Singh |
|
|
•Remove wet cloths (to prevent conductive and convective heat loss)
•Maintain horizontal position
•Protect against heat loss and wind chill (use blanket and insulating material)
•Avoid rough movement, shaking and excessive activity (to prevent arrhythmias) Monitor core temperature and cardiac activity
Assess responsiveness breathing and pulse
|
|
|
Pulse and breathing present |
|
|
Pulse or breathing absent |
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
• |
Start CPR |
|
||||||
|
|
|
|
|
|
|
|
|
|
|
• |
Give one shock |
|
||||||
|
|
Measure core temperature |
|
|
|
|
|
|
• |
Secure the airway |
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
• Ventilate with warm humid O2 |
|
|||||||
|
|
|
|
|
|
|
|
|
|||||||||||
|
|
34–36°C (93.2–96.8°F) |
|
|
|
|
|
• |
(42–46°C) |
|
|||||||||
|
|
|
|
|
|
|
Establish IV access |
|
|||||||||||
|
|
Mild hypothermia |
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
• Infuse warm NS 43°C (109°F) |
|
|||||||||||
|
|
Do passive rewarming and |
|
|
|
|
|
|
|||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
active external rewarming |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Measure core temperature |
|
|||||
30–34°C (86–93.2° F) |
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||
Moderate hypothermia |
|
|
|
|
|
|
|
|
|
|
|
||||||||
Do passive rewarming and active |
|
|
|
|
|
|
|
|
|
|
|
||||||||
external rewarming of truncal areas only |
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
<30°C |
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
<30°C (86.0° F) |
|
|
|
|
|
|
|
|
|
|
|
||||||||
Severe hypothermia |
|
|
|
|
|
|
|
|
|
|
|
||||||||
• |
Active internal warming |
|
|
|
|
|
|
|
|
|
|
|
|||||||
• Infuse warm IV fluids at 43°C |
|
|
|
|
|
|
|
|
|
||||||||||
|
|
|
|
Continue CPR |
|
|
|
||||||||||||
|
|
(109°F) |
|
|
|
|
Withhold IV drugs |
|
|||||||||||
• Warm humid O2 at 42–46°C (108– |
|
|
|
|
1 shock for VF/VT |
|
|||||||||||||
|
|
115°F) |
|
|
|
|
Active internal warming |
|
|||||||||||
• Peritoneal lavage with KCl-free |
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|||||||||
• |
|
fluid |
|
|
|
|
|
|
|
|
|
|
|
||||||
Extracorporeal rewarming |
|
|
|
|
|
|
|
|
|
>30°C |
|||||||||
• |
Esophageal rewarming tubes |
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
Step4 |
|
|
|
|
Continue CPR |
||||||||||
|
|
|
|
Continue internal rewarming until |
|
Give IV medications as indicated but |
|||||||||||||
|
|
|
|
Core temperature >35°C (95°F) OR |
|
space at long interval than standard |
|||||||||||||
|
|
|
|
Return of spontaneous circulation OR |
|
Repeat shock for VF/VT as the core |
|||||||||||||
|
|
|
|
Resuscitative efforts cease |
|
|
|
|
temperature rises |
||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
Rewarm as moderate hypothermia |
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Fig. 72.3 Stepwise management of hypothermia
