
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index
Pulmonary Artery Catheterization |
93 |
|
|
Rajesh Chawla, Vishakh Varma, and Atul Kulkarni |
|
A 65-year-old male patient, a known case of chronic obstructive pulmonary disease with cor pulmonale, hypertension, and coronary artery disease with chronic congestive heart failure, was admitted to the ICU with right lower lobe pneumonia. He was in respiratory failure and in shock. On the second day, he developed renal failure and azotemia. A pulmonary arterial catheter (PAC) was inserted.
The pulmonary artery catheterization (PAC) provides direct pressure measurements from the right atrium, right ventricle, pulmonary artery, and pulmonary artery occlusion pressure. It is also a mean of measuring cardiac output and mixed venous oxygen saturation. Routine use of this should be avoided, but it has still a role in expert hands in cardiac surgery, difficult to treat heart failure, congenital heart disease, and complex fluid management situations.
Step 1: Assess the need for PAC—indications
•PAC is used in situations where right-sided pressures (i.e., central venous pressure [CVP]) may not reflect the changes in pressures in the left side of the heart. Right-sided filling pressures are disproportionately elevated compared to the left-sided filling pressures.
R. Chawla, M.D., F.C.C.M. (*) • V. Varma, M.D.
Department of Respiratory, Critical Care & Sleep Medicine, Indraprastha Apollo Hospitals, New Delhi, India
e-mail: drchawla@hotmail.com
A. Kulkarni, M.D.
Department of Anaesthesia, Critical Care and Pain, Tata Memorial Hospital,
Mumbai, India
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
743 |
DOI 10.1007/978-81-322-0535-7_93, © Springer India 2012 |
|
744 |
R. Chawla et al. |
|
|
•PAC should be used in centers with nursing expertise in the management of catheters and sufficient physician experience in the interpretation of data in the following conditions:
–For management of heart failure
•Patients with refractory shock not responding to noninvasive management
•Patients with significant azotemia on diuretic therapy and are clinically volume overloaded
•As part of workup or bridge to cardiac transplant or the left ventricular assist device
–Complex fluid management (shock, burns, acute renal failure, major surgery) in patients with poor left or right ventricular function
–Cardiac surgery patients on cardiopulmonary bypass or patients with complex cardiac lesions
–High-risk obstetric cases such as severe preeclampsia and abruptio placentae
–Surgical procedures such as liver transplant and aortic cross clamping
Step 2: Check for the contraindications
Relative contraindications are as follows:
•Complete left bundle branch block may convert to complete heart block.
•Wolff–Parkinson–White syndrome and Ebstein’s malformation because of possible tachyarrhythmias. A catheter with pacing capability is preferred in these situations.
•Coagulopathy.
•Severe pulmonary hypertension.
•It should not be used in centers that do not have experience and expertise in its use.
Step 3: Know the PAC
•Circumference should be 7–9 Fr.
•Length is 110 cm, marked at 10 cm intervals.
•The distal port (yellow colored) at the catheter tip is used for monitoring of pulmonary artery pressure.
•The second port (blue colored) is 30 cm proximal from the tip and is used for monitoring of CVP and injecting fluid bolus for computing cardiac output with bolus technique.
•The third lumen (red colored) leads to a balloon near the tip, with a locking port.
•The fourth lumen houses wires for a temperature thermistor, the end of which lies just proximal to the balloon. This attaches to the interface cable from the cardiac output monitor.
•The continuous cardiac output PAC has a copper thermal filament embedded in the catheter at 30 cm. Once inserted and connected to the monitor, this filament heats up every few seconds, warms blood around it, and thermistor in the pulmonary artery detects the change in temperature and calculates cardiac output.
93 Pulmonary Artery Catheterization |
745 |
|
|
The PAC set also contains the following:
•Large-bore introducer sheath with a one-way valve at its outer end and a side arm extension for intravenous access. (The PAC is introduced through the one-way valve. Some sets may not contain this sheath, but is also available separately.)
•Stiff dilator
•Plastic sheath to cover the catheter
•A 1.5-mL syringe for balloon inflation
•Guidewire
•Puncture needles and syringes
•Three ways and connectors
•A disposable knife
Step 4: Obtain informed consent
This has been explained in detail in Chap. 91.
Step 5: Select the appropriate PAC for insertion
•Select the PAC which is appropriate for that patient.
•Catheters are available, which can perform the following additional functions:
–An extra venous infusion port.
–Pacing capability.
–Continuous mixed venous oximetry: Special fiber-optic PACs can be used to
monitor mixed venous oxygen saturation (SvO2) continuously, initially developed as a surrogate for continuous cardiac output.
–An ejection fraction catheter has a faster thermistor response time so that it can calculate RV ejection fraction in addition to the cardiac output.
–Continuous cardiac output.
Step 6: Prerequisites
•Establish monitoring of ECG, noninvasive blood pressure, and pulse oximetry.
•Keep ready all emergency medication and transcutaneous pacing equipment.
•Provide sedation in a conscious patient.
•Supply oxygen through the nasal cannula.
•Secure a peripheral venous access.
•Assemble the pressure transducer and flush it.
•An assistant is needed who can prepare the set and closely monitor the patient.
•The patient should be in supine position with the head slightly down and turned toward the opposite side.
•Make use of maximum sterile barrier precautions, described Chap. 91.
Step 7: Choose the site of insertion
•Generally the right internal jugular vein or left subclavian is selected.
•Alternatively any other site used for central venous cannulation can be selected keeping in mind the distance from the puncture site to the right atrium.
•An extra distance of 5–10 cm from the left internal jugular, 15 cm from the femoral veins, and 30–35 cm from the antecubital veins is required. But accurate placement rates are lower from these sites.
746 |
R. Chawla et al. |
|
|
Step 8: Prepare the cannulation set
With maximum sterile precautions do the following:
•Pass the catheter through the sterile sheet.
•Flush the catheter with heparinized saline.
•Inflate the balloon with 1.5 mL air and check for its shape and any leakage.
•Zero and level the transducer and connect to the saline-filled catheter.
•Place the tip of the catheter at the heart level; pressure on the monitor should read zero.
•Next, raise the catheter tip to 30 cm height; the monitor should show a pressure of 22 mmHg (equivalent to 30 cm H2O).
Step 9: Insertion of PAC through internal jugular vein
•Use maximum sterile barrier precautions.
•Apply generous local anesthesia.
•Locate the internal jugular vein.
•Puncture the vein with the puncture needle preferably under ultrasound guidance.
•Pass the guidewire through the needle and remove the needle.
•Dilate the skin and subcutaneous tissue with the dilator. This is generally done with the dilator loaded inside the introducer sheath. A small incision is often needed.
•Pass the large-bore sheath using Seldinger technique.
•Confirm placement by aspirating blood, flush it, and secure it with stitches.
•Introduce the prepared catheter through the introducer up to a distance of 20 cm with the balloon deflated. Note the waveform on the monitor—CVP tracing should be seen.
•Rotate the catheter so that curvature is at 11 o’clock position from patient’s head end.
•Inflate the balloon gently with 1.5 cc of air and lock it. During pulmonary artery occlusion pressure (PAOP) measurement if the balloon is left inflated, you may cause a pulmonary infarct.
•Advance slowly and keep looking at the monitor for RV waveform with systolic peaks of 25–35 mmHg. Note that the diastolic pressure is close to zero. This is reached at around 30–35 cm length.
•If the RV or PA is difficult to enter:
–Have the patient take deep breath.
–Raise the head end of the bed or tilt the table to left or right.
–Flush the PA port with 1–2 mL cold sterile saline so that the catheter becomes stiff.
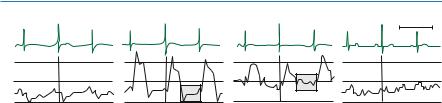
•Keep inserting further; PA is reached at 40–45 cm. At PA, there is an increase in the diastolic pressure (Fig. 93.1).
•Now advance another 5–10 cm or so very gradually keeping an eye on the monitor to look for wedging. When it is wedged, the waveform becomes similar to that of CVP tracing at a pressure near to the PA diastolic pressure. This is the pulmonary artery occlusion pressure PAOP, and it is always lower than the pulmonary artery diastolic pressure (Fig. 93.1).
93 Pulmonary Artery Catheterization |
|
747 |
||
|
|
|
1 sec |
|
30 |
R |
R |
R |
|
R |
||||
|
|
a c |
||
a c v |
|
|
||
|
|
|
||
0 |
|
|
|
|
Right atrium |
Right ventricle |
Pulmonary artery |
Wedge |
|
Fig. 93.1 Pressure tracings recorded from the right atrium, right ventricle, pulmonary catheter, and on pulmonary artery occlusion
•Do not advance any further; deflate the balloon.
•Now inflate the balloon with 0.5 cc increments and look for wedging. If it wedges before 1.5 cc, pull the catheter back 3–4 cm. Do not pull with the inflated balloon.
•Fix the catheter at that length. Note the length of the catheter that led to a good PAOP tracing in the case chart.
•Never keep the PAC wedged continuously; deflate the balloon after taking the readings.
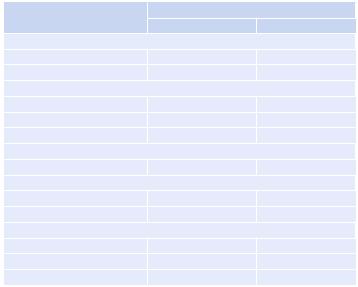
•Measured and derived hemodynamic indices values are mentioned in Tables 93.2 and 93.3.
Step 10: Manage complications
•Minor complications are seen in up to 50% of patients, but major complications are seen in only 0.1–0.5% of patients.
Besides all the complications of insertion and maintenance of central venous
lines, there are a few unique complications of the use of the PAC (Table 93.1).
Step 11: Interpretation of data obtained (Tables 93.2, 93.3 and 93.4)
Measuring Cardiac Output
•Enter the catheter constant into the monitor; this is generally written on the pack of the set or the insert.
•10 mL of cold or room temperature saline is smoothly injected from the proximal (blue) port in the right atrium. In small children or patients with volume overload, smaller volumes (2 and 5 mL) may be used.
•A cable from the cardiac output monitor is dipped into the same bottle saline from which the injectant volume was aspirated.
•The temperature of the blood mixed and cooled with the cold saline is measured at the end of the catheter by a thermistor.
•This produces a thermodilution curve, from which the cardiac output is calculated by the monitor. Usually three measurements are made.
•These measurements may have a variability of up to 10%.
•There are various factors that influence the accuracy that include intracardiac shunts, tricuspid regurgitation, pulmonary valve regurgitation, respiratory cycle influences, and rapid injection of saline.
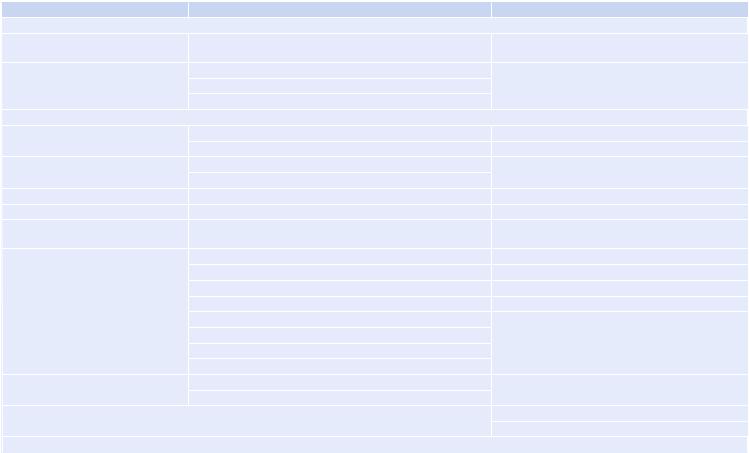
Table 93.1 Complications of the PAC |
|
|
Complication |
Description |
Treatment |
I. Catheterization |
|
|
a. Arrhythmias, ventricular |
Self-limited arrhythmias extremely common during passage |
3.1% of patients require treatment, mostly withdrawal |
fibrillation |
|
of catheter or guidewire |
b. Right bundle branch block, |
Transient during passage in 5% |
May need transcutaneous or transvenous pacing |
complete heart block |
Permanent in 0.9% |
|
|
Should rule out ischemia |
|
II. Catheter resistance |
|
|
a. Mechanical, catheter knots |
Suspect if the catheter is blocked or difficulty in withdrawing |
Radiological maneuver |
|
Confirm on a chest X-ray |
Surgery |
b. Thromboembolism |
Clots seen within hours |
The heparin-coated catheter reduces risk |
|
Thromboembolism rare |
|
c. Pulmonary infarction |
Opacity on a chest X-ray |
Removal of the catheter |
d. Infection, endocarditis |
Significant risk after 72 h especially in septic patients |
Should be removed as soon as feasible |
e. Endocardial damage, cardiac |
53% in autopsy series, but clinically significant regurgitation |
Removal of the catheter |
valve injury |
does not occur |
|
f. Pulmonary artery rupture |
0.02–0.2% of patients |
One-lung ventilation to isolate normal lung |
|
Mortality is 50% |
Positive end-expiratory pressure to the affected lung |
|
Cause: |
Reverse anticoagulation |
|
Excessive insertion depth |
May try to reinflate to cause tamponade |
|
Persistent wedging |
May need surgical intervention |
|
Frequent manipulations |
|
|
Inflation with liquid |
|
|
Presents as hemoptysis and desaturation |
|
g. Pulmonary artery |
Sequelae of PA rupture |
Surgery may be needed |
pseudoaneurysm |
May cause secondary hemorrhage |
|
III. Misinterpretation of data |
|
May be widespread |
|
|
Use requires expertise and experience |
IV. Misuse of equipment |
|
|
93 Pulmonary Artery Catheterization |
|
749 |
|
|
|
Table 93.2 Normal cardiovascular pressures |
|
|
|
Pressure |
|
|
Average (mmHg) |
Range (mmHg) |
Right ventricle |
|
|
Peak systolic |
25 |
15–30 |
End-diastolic |
6 |
1–7 |
Pulmonary artery |
|
|
Peak systolic |
25 |
15–30 |
End-diastolic |
9 |
4–12 |
Mean |
15 |
9–19 |
Pulmonary artery wedge |
|
|
Mean |
9 |
4–12 |
Left ventricle |
|
|
Peak systolic |
130 |
90–140 |
End-diastolic |
8 |
5–12 |
Central aorta |
|
|
Peak systolic |
130 |
90–140 |
End-diastolic |
70 |
60–90 |
Mean |
90 |
70–105 |
Continuous Thermodilution Cardiac Output
•Near-continuous cardiac output can be measured by a specially designed pulmonary artery catheter.
•The RV portion of the catheter has a thermal filament that releases a small amount of heat in a pulsatile manner.
•This temperature variation is measured at the tip of the catheter. It has a measurement delay of 5–15 min, but the measurement is quite reliable.
•Acute changes in cardiac output are detected more slowly, but it has the advantage of ease of operation, minimal handling, and reduced risk of fluid overload.
Pulmonary Capillary Wedge Pressure
•Imagine that the vessel in which the pulmonary artery catheter lies is like a tube connected to the left atrium.
•When there is no flow of blood through the tube, the pressure at the tip of the tube will be the same as the pressure at the left atrium. So, we stop the blood flow by inflating the balloon and measure the pressure at the tip of the pulmonary artery catheter and call it the pulmonary capillary wedge pressure (PCWP), but technically the correct term is pulmonary artery occlusion pressure (PAOP) as PCWP is actually lower than PAOP.
•Pulmonary artery diastolic pressure can be used as an alternative to PCWP to measure left ventricular filling pressure, which we assume predicts left ventricular volume.
750
Table 93.3 Derived hemodynamic indices |
|
|
|
|
Parameter |
Physiologic significance |
Formula |
Normal value |
|
Systemic vascular resistance |
Reflects impedance of the systemic vasculature |
80 |
× (MAP−CVP)/CO |
700–1,600 dyne·s·cm−5 |
Pulmonary vacular resistance |
Reflects impedance of pulmonary circuit |
80 |
× (PAM−PCWP)/CO |
20–130 dynes·cm−5 |
Cardiac index |
Allows for meaningful comparison between patients |
CO/BSA |
2.5–4.2 L·min−1·m−2 |
|
Stroke volume index |
Reflects fluid status and ventricular performance |
CI/HR × 1,000 |
40–60 mL·beat−1·m−2 |
|
Left ventricular stroke work index |
Estimates work of the left ventricle, reflects contractile state |
(MAP − PCWP) × SVI × 0.0136 |
45–60 gm·m−2 |
|
Right ventricular stroke work |
Estimates work done by the right entricle and RV |
(PAM − CVP) × SVI × 0.0136 |
5–10 gm·m−2 |
|
index |
performance |
|
|
|
CI cardiac index, CO cardiac output, CVP central venous pressure, HR heart rate, MAP mean arterial pressure, PAM pulmonary artery mean pressure, PCWP pulmonary capillary wedge pressure, SVI stroke volume index
.al et Chawla .R
