
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index
Severe Preeclampsia |
75 |
|
|
Rajesh Chawla, Prashant Nasa, and Renu Chawla |
|
A 23-year-old female at 30 weeks of pregnancy was admitted to the hospital with an episode of seizure, epigastric pain, and decreased urine output. She had pedal edema, and her blood pressure (BP) on admission was 190/110 mmHg. Her urine output was 300 mL in the past 24 h. Urine examination showed protein 4+ and hemoglobin 8 g%. Liver function test showed elevated aspartate aminotransferase and alanine aminotransferase.
Hypertensive disorders complicate 5–10% of all pregnancies. Preeclampsia either alone or superimposed on chronic hypertension may be associated with adverse outcomes.
Step 1: Initial assessment and resuscitation
•Always anticipate difficult airway in pregnant patients (Table 75.1).
•Endotracheal intubation should be performed by a senior intensivist/ anesthesiologist.
•Difficult airway equipment for airway management must be thoroughly checked before proceeding to intubation, and alternative plan for definitive airway including surgical access should already be identified.
Rajesh Chawla, M.D., F.C.C.M. (*)
Department of Respiratory, Critical Care & Sleep Medicine, Indraprastha Apollo Hospitals, New Delhi, India
e-mail: drchawla@hotmail.com
P. Nasa, M.D., F.N.B.
Department of Critical Care Medicine, Max Superspeciality Hospital, New Delhi, India
Renu Chawla, M.D.
Department of Obstetrics and Gynaecology, Max Super Speciality Hospital,
Patparganj, Delhi, India
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
599 |
DOI 10.1007/978-81-322-0535-7_75, © Springer India 2012 |
|
600 |
R. Chawla et al. |
|
|
Table 75.1 Risk factors for difficult airway during pregnancy
Progesterone-induced airway edema is further exacerbated in pregnancy-induced hypertension (PIH)
Thick neck, large breasts
Increased risk of hypoxemia—decreased cardiopulmonary reserve and increased metabolic requirements
Increased risk of aspiration of gastric contents
•Supplemental oxygen may be required in some patients depending on their oxygen saturation.
•Target SpO2 more than 95% with oxygen or ventilation.
Circulation
•Two large-bore intravenous cannulae (14G or 16G) should be placed to administer fluids.
•The Foley catheter should be placed to monitor urine output.
•Judicious fluid administration is needed to optimize preload and at the same time to avoid overload.
•Nurse in the left lateral position (30° wedge to the right hip) to prevent supine hypotension syndrome.
Disability (neurological)
•Magnesium sulfate is a drug of choice for control of seizures.
•4–6 g is diluted in 100 mL of IV fluid bolus over 20 min.
Step 2: Taking history and physical examination
•Detailed history should be taken about pregnancy, antenatal evaluation, immunization, hypertension, and PIH (pregnancy induced hypertension) during the previous pregnancy.
•Complications and outcome of the previous pregnancy and family history of hypertension should be required.
•History includes symptoms displaying end-organ effects to detect presence of severe preeclampsia:
–Headache
–Visual disturbances—blurred, scintillating scotomas
–Altered mental status
–Blindness
–Dyspnea
–Edema
–Epigastric or right upper quadrant abdominal pain
–Weakness or malaise—may be evidence of hemolytic anemia
•The physical examination includes the evaluation of end-organ dysfunction for diagnosis of severe preeclampsia:
–Altered mental status
–Decreased vision or scotomas
75 Severe Preeclampsia |
601 |
|
|
Table 75.2 Criteria for diagnosing severe preeclampsia
Systolic BP of 160 mmHg or higher or diastolic BP of 110 mmHg or higher on two occasions at least 6 h apart
Proteinuria of more than 5 g in a 24-h collection or more than 3+ on two random urine samples collected at least 4 h apart
Pulmonary edema or cyanosis
Oliguria (<400 mL in 24 h)
Thrombocytopenia, DIC, HELLP
Persistent headaches
Epigastric pain and/or impaired liver function
Oligohydramnios, decreased fetal growth, or placental abruption
–Papilledema
–Epigastric or right upper quadrant abdominal tenderness
–Peripheral edema
–Seizures
–Focal neurologic deficit
•PIH (preeclampsia) is defined as presence of hypertension (BP ³140/90 mmHg) on two occasions, at least 6 h apart in more than 20 weeks’ gestation in women with previously normal BP and who have proteinuria (³0.3 g protein in 24-h urine specimen), with or without pedal edema.
•Severe preeclampsia is defined in Table 75.2.
•Eclampsia is defined as seizures that cannot be attributable to other causes in a woman with preeclampsia.
Step 3: Send investigations
•Complete blood cell count.
•Liver function tests.
•Renal function tests and serum electrolytes.
•Arterial blood gas and blood glucose.
•Coagulation profile (prothrombin time [PT], activated partial thromboplastin time [aPTT], and fibrinogen, international normalized ratio).
•Lactate dehydrogenase.
•Uric acid.
•Urine routine microscopy, 24-h urine protein, and creatinine.
•Additional tests—peripheral smear, serum magnesium levels.
•Ultrasonography is used to assess the status of the fetus as well as to evaluate growth retardation.
•Transthoracic echocardiography.
Step 4: Make a differential diagnosis (Table 75.3)
Step 5: Admit to the ICU and monitor closely
ICU admission is indicated with:
• Obstetric hemorrhage
602 |
R. Chawla et al. |
|
|
Table 75.3 Differential |
Severe preeclampsia (abdominal pain) |
diagnosis |
Abruptio placentae |
|
|
|
Abdominal aneurysm |
|
Acute appendicitis |
|
Blunt abdominal trauma |
|
Cholecystitis and biliary colic |
|
Encephalitis |
|
Hypertensive emergencies |
|
Ovarian torsion |
|
Status epilepticus |
|
Thrombotic thrombocytopenic purpura |
|
Poisoning |
|
Eclampsia (seizure) |
|
Cerebrovascular accidents |
|
Brain tumors |
|
Brain infections—meningitis, encephalitis, abscesses |
|
Thrombotic thrombocytopenic purpura |
|
Metabolic disorders |
|
Hypertensive encephalopathy |
|
Illicit drug use |
|
Postdural puncture syndrome |
|
Epilepsy |
|
Posterior reversible encephalopathy syndrome |
•Placental abruption
•Severe preeclampsia/eclampsia
•Hemolysis, elevated liver enzymes, and low platelet (HELLP) syndrome
•Chorioamnionitis
•Acute pulmonary edema
•Respiratory failure
•Acute respiratory distress syndrome
•Acute renal failure
Maternal monitoring is required with severe preeclampsia:
•Repeated clinical assessment including neurological examination (deep tendon reflexes for magnesium toxicity).
•ECG.
•Arterial BP—noninvasive BP can be tried initially but may be incorrect with inadequate cuff size.
•Pulse oximetry.
•Foley catheterization—urine output monitoring.
•Blood gas monitoring.
•CVP monitoring—infusion of vasopressors.
•Additional—intra-abdominal pressure during resuscitation, serum magnesium levels.
75 Severe Preeclampsia |
603 |
|
|
Step 6: Management of severe preeclampsia
The most important aspect in the management of severe preeclampsia is control of hypertension.
A. BP control
•Arterial pressure greater than 160/110 mmHg in preeclampsia can increase the risk of complication, and it should be controlled.
•BP control should only be done in the ICU, preferably with arterial line monitoring.
•BP control should also be done along with fetal monitoring. Avoid sudden fall in BP as it can result in fetal distress.
•Goal of BP control is 15–25% reduction in the mean arterial pressure, and reduction of pressure to normal levels (<140/90 mmHg) should be avoided as it may compromise placental perfusion.
•Drugs
–Labetalol (IV 20 mg) can be given initially followed by doubling the dose every 10 min to a cumulative dose of 300 mg. This drug can result in severe bradycardia. A continuous infusion of labetalol at a rate of 0.5–2 mg/ min can also be used.
–Hydralazine (5–10 mg) can be given every 20 min (maximum of 40 mg) until BP is controlled.
–Nifedipine or nicardipine can be given (sudden precipitous decrease in BP or bradycardia can occur).
–Intravenous nitroglycerin (10–100 mg/min) or sodium nitroprusside (2–8 mg/ min) can be given. Prolonged use of nitroglycerin may lead to methemoglobinemia. Cyanide toxicity in the mother and fetus may occur with sodium nitroprusside, limiting its use to less than 4 h and only as a last resort.
B.Seizure control
•The initial management of eclampsia includes airway, breathing, and circulation.
•The initial bolus of magnesium (4 g over 20 min) is followed by an infusion of 1–2 g/h.
•The mechanism of action of magnesium is unknown, but magnesium suppresses excitatory neurotransmitter release by replacing calcium at nerve endings.
•Monitor toxicity—loss of deep tendon reflexes; loss of patellar reflex occurs when the plasma magnesium level is more than 10 mg%. Look for respiratory muscle weakness.
•Magnesium has a relatively narrow therapeutic range, and target magnesium serum concentrations are 5–8 mg/dL.
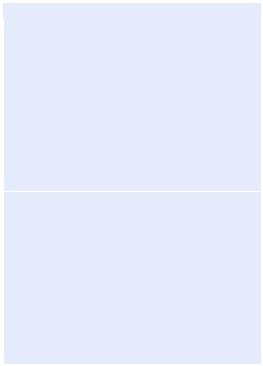
•Infusion dose should be reduced in case of renal dysfunction. Serum magnesium level should be monitored Table 75.4.
•In recurrent seizure, additional 2 g of magnesium sulfate can be given concurrently with the magnesium sulfate infusion.
•If seizures are not controlled by repeat magnesium bolus, then diazepam or lorazepam can be administered (See chap. 28).
•Discontinue magnesium sulfate 24 h after delivery.
604 |
R. Chawla et al. |
|
|
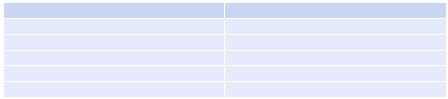
Table 75.4 Clinical manifestations related to serum concentration of Magnesium |
|
Serum magnesium levels (mg/dL) |
Effects |
5–8 |
Therapeutic |
8–12 |
Loss of deep tendon reflexes |
>12 |
Prolonged atrioventricular conduction |
15–17 |
Muscular paralysis and respiratory difficulties |
>20 |
Cardiac arrest |
C.Fluid management
•Despite the peripheral edema, patients with preeclampsia are volume depleted with high peripheral vascular resistance. Diuretics should be avoided.
•Aggressive volume resuscitation, on the other hand may lead to pulmonary edema, which is a common cause of maternal morbidity and mortality. Because volume expansion has no demonstrated benefit, patients should be fluid restricted when possible, at least until the period of postpartum diuresis.
•Central venous or pulmonary artery pressure monitoring or other hemodynamic monitoring modality may be indicated in critical cases.
•Careful measurement of fluid input and output is advisable, particularly in the immediate postpartum period.
D.Delivery
•Women with severe preeclampsia who are managed expectantly must be delivered under the following circumstances:
•Nonreassuring fetal heart status
•Uncontrollable BP
•Oligohydramnios, with amniotic fluid index of less than 5 cm
•Severe intrauterine growth restriction
•Oliguria (<500 mL/24 h)
•Serum creatinine level of at least 1.5 mg/dL
•Pulmonary edema
•Shortness of breath or chest pain with pulse oximetry of <94% on room air
•Headache that is persistent and severe
•Right upper quadrant tenderness with deteriorating liver function test
•Development of HELLP syndrome
Step 7: Watch for complications
•Abruptio placentae
•Disseminated intravascular coagulopathy (DIC)
•Renal insufficiency and acute renal failure
•HELLP syndrome
•Eclampsia
•Cerebral hemorrhage
•Fetal changes—intrauterine growth restriction, abruptio placentae, oligohydramnios
•Intrauterine fetal death
