
- •ICU Protocols
- •Preface
- •Acknowledgments
- •Contents
- •Contributors
- •1: Airway Management
- •Suggested Reading
- •2: Acute Respiratory Failure
- •Suggested Reading
- •Suggested Reading
- •Website
- •4: Basic Mechanical Ventilation
- •Suggested Reading
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Websites
- •7: Weaning
- •Suggested Reading
- •8: Massive Hemoptysis
- •Suggested Reading
- •9: Pulmonary Thromboembolism
- •Suggested Reading
- •Suggested Reading
- •Websites
- •11: Ventilator-Associated Pneumonia
- •Suggested Readings
- •12: Pleural Diseases
- •Suggested Reading
- •Websites
- •13: Sleep-Disordered Breathing
- •Suggested Reading
- •Websites
- •14: Oxygen Therapy
- •Suggested Reading
- •15: Pulse Oximetry and Capnography
- •Conclusion
- •Suggested Reading
- •Websites
- •16: Hemodynamic Monitoring
- •Suggested Reading
- •Websites
- •17: Echocardiography
- •Suggested Readings
- •Websites
- •Suggested Reading
- •Websites
- •19: Cardiorespiratory Arrest
- •Suggested Reading
- •Websites
- •20: Cardiogenic Shock
- •Suggested Reading
- •21: Acute Heart Failure
- •Suggested Reading
- •22: Cardiac Arrhythmias
- •Suggested Reading
- •Website
- •23: Acute Coronary Syndromes
- •Suggested Reading
- •Website
- •Suggested Reading
- •25: Aortic Dissection
- •Suggested Reading
- •26: Cerebrovascular Accident
- •Suggested Reading
- •Websites
- •27: Subarachnoid Hemorrhage
- •Suggested Reading
- •Websites
- •28: Status Epilepticus
- •Suggested Reading
- •29: Acute Flaccid Paralysis
- •Suggested Readings
- •30: Coma
- •Suggested Reading
- •Suggested Reading
- •Websites
- •32: Acute Febrile Encephalopathy
- •Suggested Reading
- •33: Sedation and Analgesia
- •Suggested Reading
- •Websites
- •34: Brain Death
- •Suggested Reading
- •Websites
- •35: Upper Gastrointestinal Bleeding
- •Suggested Reading
- •36: Lower Gastrointestinal Bleeding
- •Suggested Reading
- •37: Acute Diarrhea
- •Suggested Reading
- •38: Acute Abdominal Distension
- •Suggested Reading
- •39: Intra-abdominal Hypertension
- •Suggested Reading
- •Website
- •40: Acute Pancreatitis
- •Suggested Reading
- •Website
- •41: Acute Liver Failure
- •Suggested Reading
- •Suggested Reading
- •Websites
- •43: Nutrition Support
- •Suggested Reading
- •44: Acute Renal Failure
- •Suggested Reading
- •Websites
- •45: Renal Replacement Therapy
- •Suggested Reading
- •Website
- •46: Managing a Patient on Dialysis
- •Suggested Reading
- •Websites
- •47: Drug Dosing
- •Suggested Reading
- •Websites
- •48: General Measures of Infection Control
- •Suggested Reading
- •Websites
- •49: Antibiotic Stewardship
- •Suggested Reading
- •Website
- •50: Septic Shock
- •Suggested Reading
- •51: Severe Tropical Infections
- •Suggested Reading
- •Websites
- •52: New-Onset Fever
- •Suggested Reading
- •Websites
- •53: Fungal Infections
- •Suggested Reading
- •Suggested Reading
- •Website
- •55: Hyponatremia
- •Suggested Reading
- •56: Hypernatremia
- •Suggested Reading
- •57: Hypokalemia and Hyperkalemia
- •57.1 Hyperkalemia
- •Suggested Reading
- •Website
- •58: Arterial Blood Gases
- •Suggested Reading
- •Websites
- •59: Diabetic Emergencies
- •59.1 Hyperglycemic Emergencies
- •59.2 Hypoglycemia
- •Suggested Reading
- •60: Glycemic Control in the ICU
- •Suggested Reading
- •61: Transfusion Practices and Complications
- •Suggested Reading
- •Websites
- •Suggested Reading
- •Website
- •63: Onco-emergencies
- •63.1 Hypercalcemia
- •63.2 ECG Changes in Hypercalcemia
- •63.3 Superior Vena Cava Syndrome
- •63.4 Malignant Spinal Cord Compression
- •Suggested Reading
- •64: General Management of Trauma
- •Suggested Reading
- •65: Severe Head and Spinal Cord Injury
- •Suggested Reading
- •Websites
- •66: Torso Trauma
- •Suggested Reading
- •Websites
- •67: Burn Management
- •Suggested Reading
- •68: General Poisoning Management
- •Suggested Reading
- •69: Syndromic Approach to Poisoning
- •Suggested Reading
- •Websites
- •70: Drug Abuse
- •Suggested Reading
- •71: Snakebite
- •Suggested Reading
- •72: Heat Stroke and Hypothermia
- •72.1 Heat Stroke
- •72.2 Hypothermia
- •Suggested Reading
- •73: Jaundice in Pregnancy
- •Suggested Reading
- •Suggested Reading
- •75: Severe Preeclampsia
- •Suggested Reading
- •76: General Issues in Perioperative Care
- •Suggested Reading
- •Web Site
- •77.1 Cardiac Surgery
- •77.2 Thoracic Surgery
- •77.3 Neurosurgery
- •Suggested Reading
- •78: Initial Assessment and Resuscitation
- •Suggested Reading
- •79: Comprehensive ICU Care
- •Suggested Reading
- •Website
- •80: Quality Control
- •Suggested Reading
- •Websites
- •81: Ethical Principles in End-of-Life Care
- •Suggested Reading
- •82: ICU Organization and Training
- •Suggested Reading
- •Website
- •83: Transportation of Critically Ill Patients
- •83.1 Intrahospital Transport
- •83.2 Interhospital Transport
- •Suggested Reading
- •84: Scoring Systems
- •Suggested Reading
- •Websites
- •85: Mechanical Ventilation
- •Suggested Reading
- •86: Acute Severe Asthma
- •Suggested Reading
- •87: Status Epilepticus
- •Suggested Reading
- •88: Severe Sepsis and Septic Shock
- •Suggested Reading
- •89: Acute Intracranial Hypertension
- •Suggested Reading
- •90: Multiorgan Failure
- •90.1 Concurrent Management of Hepatic Dysfunction
- •Suggested Readings
- •91: Central Line Placement
- •Suggested Reading
- •92: Arterial Catheterization
- •Suggested Reading
- •93: Pulmonary Artery Catheterization
- •Suggested Reading
- •Website
- •Suggested Reading
- •95: Temporary Pacemaker Insertion
- •Suggested Reading
- •96: Percutaneous Tracheostomy
- •Suggested Reading
- •97: Thoracentesis
- •Suggested Reading
- •98: Chest Tube Placement
- •Suggested Reading
- •99: Pericardiocentesis
- •Suggested Reading
- •100: Lumbar Puncture
- •Suggested Reading
- •Website
- •101: Intra-aortic Balloon Pump
- •Suggested Reading
- •Appendices
- •Appendix A
- •Appendix B
- •Common ICU Formulae
- •Appendix C
- •Appendix D: Syllabus for ICU Training
- •Index
Basic Mechanical Ventilation |
4 |
|
|
Gopi Chand Khilnani and Vijay Hadda |
|
A 30-year-old male patient came to the emergency department with history of fever, shortness of breath for 3 days, and alteration in sensorium since morning. He was in respiratory distress with respiratory rate of 34/min. He was drowsy (Glasgow coma score 8) and febrile (102°F). His pulse was 110/min, blood pressure was 116/78 mmHg, and JVP was normal. He was immediately intubated and put on assisted ventilation.
Mechanical ventilation is indicated in patients with acute respiratory failure when they are unable to maintain adequate oxygenation and / or remove carbon dioxide. None of the ventilatory mode can cure the disease process. However, it supports ventilation till you address the reversible primary problem. Mechanical ventilation should not be started without thoughtful consideration as tracheal intubation and ventilation are associated with significant complications.
Step 1: Initial resuscitation (refer to Chap. 78)
•Any patient coming to the emergency department should be examined quickly to assess oxygenation and hemodynamic status. Resuscitation should be started without delay.
•All patients with respiratory distress require immediate attention to airway.
•They should be put on high-flow oxygen except patients with chronic obstructive pulmonary disease where low flow oxygen can be started to increase SpO2 to
G.C. Khilnani, M.D., F.C.C.P. (*)
Department of Medicine, All India Institute of Medical Sciences, New Delhi, India e-mail: gckhil@hotmail.com
V. Hadda, M.D.
Department of Medicine, Postgraduate Institute of Medical Education & Research,
Chandigarh, India
R. Chawla and S. Todi (eds.), ICU Protocols: A stepwise approach, |
31 |
DOI 10.1007/978-81-322-0535-7_4, © Springer India 2012 |
|
32 |
G.C. Khilnani and V. Hadda |
|
|
Table 4.1 Indications and objectives of mechanical ventilation
To overcome the mechanical problem
Rest/unloading of the fatigued/overloaded inspiratory muscles
Prevention or treatment of the lung atelectasis
An adjunct to anesthetic or neuromuscular blockade
Treatment for flail chest
To regulate gas exchange
Reverse hypoxemia in patients with respiratory failure
Keep PaCO2 lower than normal in patients with raised intracranial pressure Normalize the PaCO2 in patients with muscle fatigue or neuromuscular disease
To increase the lung volume
During end inspiration—minimize V/Q mismatch and intrapulmonary shunting, improve hypoxemia, and treat atelectasis
During end expiration (positive end-expiratory pressure [PEEP]), keep alveoli open at the end of expiration and improve gas exchange in acute respiratory distress syndrome (ARDS) and other causes of alveolar collapse
90%. If the patient requires assisted ventilation, he/she should be intubated and ventilated (Table 4.1).
•Circulation needs to be maintained by fluid infusion. If clinically evidence of cardiac impairment is present, fluids should be given cautiously.
Step 2: Choose the mode of mechanical ventilation
•Once it has been decided that patient requires mechanical ventilation, the next step is to choose the appropriate mode of mechanical ventilation.
•The characteristics of commonly used modes of mechanical ventilation are summarized in Table 4.2. Assist-control mechanical ventilation (ACMV) is the most widely used method.
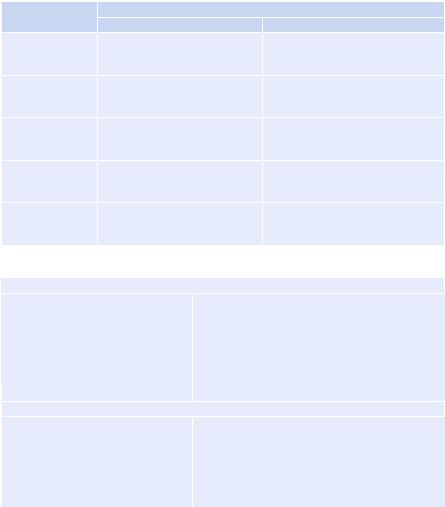
•Assist-control mode can be volume-controlled (more commonly used) or pres- sure-controlled. The differences between two are summarized in Table 4.3.
•The ventilatory support can be controlled mandatory ventilation (CMV) or assisted controlled mandatory ventilation (ACMV) depending on the use of patients’ effort for triggering the ventilator.
•The patient’s ventilation is totally controlled by the ventilator and the patient cannot trigger the ventilator during CMV, while ACMV delivers controlled breaths as well as assists patient-triggered breath.
•ACMV is the most commonly used mode of mechanical ventilation and can be used to deliver either volume-preset or pressure-preset ventilation.
•In volume-preset ACMV, a preset tidal volume (VT) is delivered, irrespective of inspiratory pressure.
•In pressure-preset ACMV, a fixed inspiratory pressure (Pinsp) is applied to the respiratory system. The VT is determined by lung and chest wall compliance and airway resistance.
•Although both volume-set and pressure-set ACMVs can achieve the same levels of ventilation, volume-preset ACMV is more frequently used.
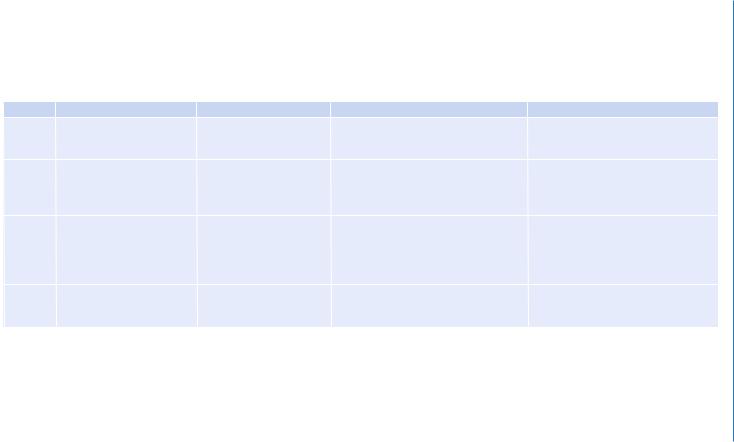
Table 4.2 Characteristics of commonly used modes of mechanical ventilation |
|
|||
Mode |
Type of breath |
Triggering mechanism |
Cycling mechanism |
Comments |
CMV |
Each breath delivers a preset |
Time |
Inspiration is terminated by delivery |
Used in patients who have no |
|
mechanical tidal volume or |
|
of preset tidal volume or by time in |
respiratory effort |
|
pressure |
|
pressure-controlled |
|
ACMV |
Each breath, assist or |
Either patient-triggered |
Inspiration is terminated either by |
Alveolar hyperventilation may be a |
|
control, delivers a preset |
(assist) or time-triggered |
delivery of preset tidal volume (volume |
potential hazard |
|
mechanical tidal volume or |
(controlled) |
controlled) or by high pressure limit or |
|
|
pressure |
|
by time in pressure-controlled |
|
SIMV |
Mechanical tidal breath at |
Mandatory breath may be |
Mandatory breaths are volumeor |
It provides an interval (synchronization |
|
preset rate and the patient |
time-triggered or patient- |
time-cycled; patient controls spontaneous |
window) just prior to triggering during |
|
may breathe spontaneously |
triggered |
rate and volume |
which the ventilator is responsive |
|
between mandatory breaths |
|
|
to patient’s effort and supports |
|
|
|
|
spontaneous breath |
PSV |
Pressure-support breaths are |
Patient-triggered |
The breaths are flow cycled by a set |
This a commonly used mode for |
|
considered as spontaneous |
|
flow threshold, which is generated |
weaning |
|
|
|
by the patient |
|
CMV controlled mandatory ventilation, ACMV assist-control mechanical ventilation, IMV intermittent mandatory ventilation, SIMV synchronized intermittent mandatory ventilation, PSV pressure-support ventilation
Ventilation Mechanical Basic 4
33
34 |
|
G.C. Khilnani and V. Hadda |
|
||
Table 4.3 Comparison between volume-controlled and pressure-controlled breaths |
||
|
Type of breath |
|
Variable |
Volume-controlled |
Pressure-controlled |
Tidal volume |
Set by the operator; remains |
Variable with changes in patients’ |
|
constant |
effort and respiratory system |
|
|
impedance |
Peak inspiratory |
Variable with changes in patients’ |
Set by the operator; remains constant |
pressure |
effort and respiratory system |
|
|
impedance |
|
Inspiratory time |
Set by the operator or as a |
Set by the operator; remains constant |
|
function of respiratory rate and |
|
|
flow settings |
|
Inspiratory flow |
Set by the operator or as a |
Variable with changes in patients’ |
|
function of respiratory rate and |
effort and respiratory system |
|
tidal volume |
impedance |
Inspiratory flow |
Set by the operator; remains |
Flow waves are always decelerating |
waveforms |
constant; can use constant, sine, or |
|
|
decelerating flow waveforms |
|
Table 4.4 Initial ventilatory setting |
|
|
Mode—assist/control (volume or pressure) |
|
|
Plateau pressure |
<30 cm H2O |
|
Tidal volume |
8 mL/Kg ideal body weight (see formula in |
|
|
Appendix 2) |
|
Inspiratory time |
0.7–1.2 s |
|
Rate |
10–12 breaths/min |
|
PEEP |
4 cm H2O |
|
FiO2 |
1.0 |
|
Once the patient is stabilized |
|
|
FiO2 |
To maintain PaO2 more than 60 mmHg |
|
PEEP |
Set according to FiO2 requirements (predetermined |
|
|
according to the degree of hypoxemia) |
|
Plateau pressure |
Recheck in an attempt to keep plateau pressure |
|
|
below 30 cm H2O |
|
Tidal volume |
Maintain 6 mL per kg of ideal body weight |
|
Step 3: Set the ventilator setting
The various initial ventilatory settings for a patient with the normal lung are given in Table 4.4.
Step 4: Set alarms
The following alarms need to be set:
•Peak pressure—high/low—10–15 cm above or below the peak inspiratory pressure generated on constant basis
•Minute ventilation—high/low—50% above or below the set volume
•Low exhaled tidal volume—50% of the delivered tidal volume
•High respiratory rate
•Set apnea ventilation parameters
4 Basic Mechanical Ventilation |
35 |
|
|
Step 5: Connect the ventilator to the patient
• Connect the patient to the ventilator.
Step 6: Monitoring and adjustments during mechanical ventilation
•Patients should be closely monitored. Plateau pressure should be measured at least every 4 h and after any changes in tidal volume and PEEP.
•The ventilatory setting should be adjusted as described in mechanical ventilation in ARDS and obstructive airway diseases in Chaps. 5 and 6.
•A few patients are difficult to rest on the ventilator and continue to demonstrate a high work of breathing.
•Auto-PEEP may be responsible for this, and addition of extrinsic PEEP to nearly counterbalance the auto-PEEP improves the patient’s comfort dramatically. The external PEEP should be set approximately 80% of auto-PEEP.
•Another approach is to increase minute ventilation though this worsens autoPEEP and bicarbonate loss.
•If the problem still persists, then a careful search should be made for processes that might drive the patient to a respiratory rate higher than is desirable (e.g., hypoperfusion, pleural effusion, and pain).
•If the patient continues to make significant inspiratory efforts after these, then judicious sedation is advised.
•If there is frequent high-pressure alarm, then look for bronchospasm, pneumothorax, atelectasis, blockade of endotracheal tube with secretions, right main bronchus intubation, etc.
•Once the patient improves and the respiratory muscles are adequately rested, the patient should assume some of the work of breathing and be evaluated for weaning from the mechanical ventilation. The patients fulfilling the weaning criteria are extubated.
Step 7: Monitor and manage complications
Ventilation is never without complications. They should be diagnosed and managed (Table 4.5).
Step 8: Weaning from the ventilator (Chap. 7)
•Patients who have recovered considerably from the underlying diseases should be assessed daily for readiness of weaning (Table 4.6), and those satisfying criteria should be given a spontaneous breathing trial (SBT).
•Patients may be given SBT for 30–120 min and patients are monitored for signs of SBT failure (Table 4.7). Those who successfully tolerate this can be extubated.
Step 9: Monitoring during postextubation period
•Once the patient is extubated, he/she should be monitored for any appearance of respiratory distress/failure because some patients may develop weaning failure and may require reintubation.

36 G.C. Khilnani and V. Hadda
Table 4.5 Complications of intubation and mechanical ventilation
Equipment
Malfunction or disconnection
Incorrect settings
Pulmonary
Airway intubation (e.g., damage to teeth, vocal cords, and trachea) Ventilator-associated pneumonia (e.g., reduced lung defense)
Ventilator-associated lung injury (e.g., diffuse lung injury due to regional overdistension or tidal recruitment of alveoli)
Overt barotraumas (e.g., pneumothorax) O2 toxicity
Patient–ventilator asynchrony
Circulation
↓ Right ventricular preload → ↓ cardiac output
↑ Right ventricular afterload (if the lung is overdistended)
↓ Splanchnic blood flow with high levels of PEEP or mean Paw ↑ Intracranial pressure with high levels of PEEP or mean Paw Fluid retention due to ↓ cardiac output → ↓ renal blood flow
Other
Gut distension (air swallowing, hypomotility) Mucosal ulceration and bleeding
Peripheral and respiratory muscle weakness
Sleep disturbance, agitation, and fear (which may be prolonged after recovery) Neuropsychiatric complications
Table 4.6 Criteria for assessing readiness of patients for weaning
Some evidence of reversal of the underlying cause of respiratory failure
Adequate oxygenation (e.g., PaO2/FiO2 > 200, requiring PEEP < 5–8 cm H2O, FiO2 < 0.4–0.5, and pH > 7.25)
Hemodynamic stability, no active myocardial ischemia, no clinically significant hypotension or use of vasopressors (dopamine or dobutamine in a lower dose, <5 mg/kg/min, acceptable)
The capability to initiate an inspiratory effort
Table 4.7 Criteria for defining failure of SBT— various parameters monitored during SBT
SpO2 £ 90% and/or PaO2 £ 60 mmHg
Spontaneous tidal volume £4 mL/kg ideal body weight
Respiratory rate ³35/min
pH £ 7.30 if measured
Respiratory distress
Two or more of the following:
Heart rate ³120/min or ³20% increase from the baseline
Marked use of accessory muscles
Abdominal paradox
Diaphoresis
Marked subjective dyspnea
