
- •Preface to the 3rd edition
- •General Pharmacology
- •Systems Pharmacology
- •Therapy of Selected Diseases
- •Subject Index
- •Abbreviations
- •General Pharmacology
- •History of Pharmacology
- •Drug and Active Principle
- •The Aims of Isolating Active Principles
- •European Plants as Sources of Effective Medicines
- •Drug Development
- •Congeneric Drugs and Name Diversity
- •Oral Dosage Forms
- •Drug Administration by Inhalation
- •Dermatological Agents
- •From Application to Distribution in the Body
- •Potential Targets of Drug Action
- •External Barriers of the Body
- •Blood–Tissue Barriers
- •Membrane Permeation
- •Binding to Plasma Proteins
- •The Liver as an Excretory Organ
- •Biotransformation of Drugs
- •Drug Metabolism by Cytochrome P450
- •The Kidney as an Excretory Organ
- •Presystemic Elimination
- •Drug Concentration in the Body as a Function of Time—First Order (Exponential) Rate Processes
- •Time Course of Drug Concentration in Plasma
- •Time Course of Drug Plasma Levels during Repeated Dosing (A)
- •Time Course of Drug Plasma Levels during Irregular Intake (B)
- •Accumulation: Dose, Dose Interval, and Plasma Level Fluctuation (A)
- •Dose–Response Relationship
- •Concentration–Effect Curves (B)
- •Concentration–Binding Curves
- •Types of Binding Forces
- •Agonists—Antagonists
- •Other Forms of Antagonism
- •Enantioselectivity of Drug Action
- •Receptor Types
- •Undesirable Drug Effects, Side Effects
- •Drug Allergy
- •Cutaneous Reactions
- •Drug Toxicity in Pregnancy and Lactation
- •Pharmacogenetics
- •Placebo (A)
- •Systems Pharmacology
- •Sympathetic Nervous System
- •Structure of the Sympathetic Nervous System
- •Adrenergic Synapse
- •Adrenoceptor Subtypes and Catecholamine Actions
- •Smooth Muscle Effects
- •Cardiostimulation
- •Metabolic Effects
- •Structure–Activity Relationships of Sympathomimetics
- •Indirect Sympathomimetics
- •Types of
- •Antiadrenergics
- •Parasympathetic Nervous System
- •Cholinergic Synapse
- •Parasympathomimetics
- •Parasympatholytics
- •Actions of Nicotine
- •Localization of Nicotinic ACh Receptors
- •Effects of Nicotine on Body Function
- •Aids for Smoking Cessation
- •Consequences of Tobacco Smoking
- •Dopamine
- •Histamine Effects and Their Pharmacological Properties
- •Serotonin
- •Vasodilators—Overview
- •Organic Nitrates
- •Calcium Antagonists
- •ACE Inhibitors
- •Drugs Used to Influence Smooth Muscle Organs
- •Cardiac Drugs
- •Cardiac Glycosides
- •Antiarrhythmic Drugs
- •Drugs for the Treatment of Anemias
- •Iron Compounds
- •Prophylaxis and Therapy of Thromboses
- •Possibilities for Interference (B)
- •Heparin (A)
- •Hirudin and Derivatives (B)
- •Fibrinolytics
- •Intra-arterial Thrombus Formation (A)
- •Formation, Activation, and Aggregation of Platelets (B)
- •Inhibitors of Platelet Aggregation (A)
- •Presystemic Effect of ASA
- •Plasma Volume Expanders
- •Lipid-lowering Agents
- •Diuretics—An Overview
- •NaCl Reabsorption in the Kidney (A)
- •Aquaporins (AQP)
- •Osmotic Diuretics (B)
- •Diuretics of the Sulfonamide Type
- •Potassium-sparing Diuretics (A)
- •Vasopressin and Derivatives (B)
- •Drugs for Gastric and Duodenal Ulcers
- •Laxatives
- •Antidiarrheal Agents
- •Drugs Affecting Motor Function
- •Muscle Relaxants
- •Nondepolarizing Muscle Relaxants
- •Depolarizing Muscle Relaxants
- •Antiparkinsonian Drugs
- •Antiepileptics
- •Pain Mechanisms and Pathways
- •Eicosanoids
- •Antipyretic Analgesics
- •Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- •Cyclooxygenase (COX) Inhibitors
- •Local Anesthetics
- •Opioid Analgesics—Morphine Type
- •General Anesthesia and General Anesthetic Drugs
- •Inhalational Anesthetics
- •Injectable Anesthetics
- •Sedatives, Hypnotics
- •Benzodiazepines
- •Pharmacokinetics of Benzodiazepines
- •Therapy of Depressive Illness
- •Mania
- •Therapy of Schizophrenia
- •Psychotomimetics (Psychedelics, Hallucinogens)
- •Hypothalamic and Hypophyseal Hormones
- •Thyroid Hormone Therapy
- •Glucocorticoid Therapy
- •Follicular Growth and Ovulation, Estrogen and Progestin Production
- •Oral Contraceptives
- •Antiestrogen and Antiprogestin Active Principles
- •Aromatase Inhibitors
- •Insulin Formulations
- •Treatment of Insulin-dependent Diabetes Mellitus
- •Treatment of Maturity-Onset (Type II) Diabetes Mellitus
- •Oral Antidiabetics
- •Drugs for Maintaining Calcium Homeostasis
- •Drugs for Treating Bacterial Infections
- •Inhibitors of Cell Wall Synthesis
- •Inhibitors of Tetrahydrofolate Synthesis
- •Inhibitors of DNA Function
- •Inhibitors of Protein Synthesis
- •Drugs for Treating Mycobacterial Infections
- •Drugs Used in the Treatment of Fungal Infections
- •Chemotherapy of Viral Infections
- •Drugs for the Treatment of AIDS
- •Drugs for Treating Endoparasitic and Ectoparasitic Infestations
- •Antimalarials
- •Other Tropical Diseases
- •Chemotherapy of Malignant Tumors
- •Targeting of Antineoplastic Drug Action (A)
- •Mechanisms of Resistance to Cytostatics (B)
- •Inhibition of Immune Responses
- •Antidotes and Treatment of Poisonings
- •Therapy of Selected Diseases
- •Hypertension
- •Angina Pectoris
- •Antianginal Drugs
- •Acute Coronary Syndrome— Myocardial Infarction
- •Congestive Heart Failure
- •Hypotension
- •Gout
- •Obesity—Sequelae and Therapeutic Approaches
- •Osteoporosis
- •Rheumatoid Arthritis
- •Migraine
- •Common Cold
- •Atopy and Antiallergic Therapy
- •Bronchial Asthma
- •Emesis
- •Alcohol Abuse
- •Local Treatment of Glaucoma
- •Further Reading
- •Further Reading
- •Picture Credits
- •Drug Indexes
330 Therapy of Selected Diseases
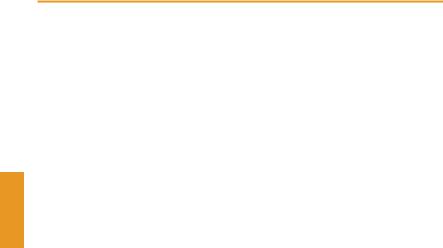
Osteoporosis
Osteoporosis is defined as a generalized decrease in bone mass (osteopenia) that equally affects bone matrix and mineral content and is associated with a change in spongiosal architecture. This condition predisposes to collapse of vertebral bodies and bone fractures with trivial trauma (e.g., hip fractures).
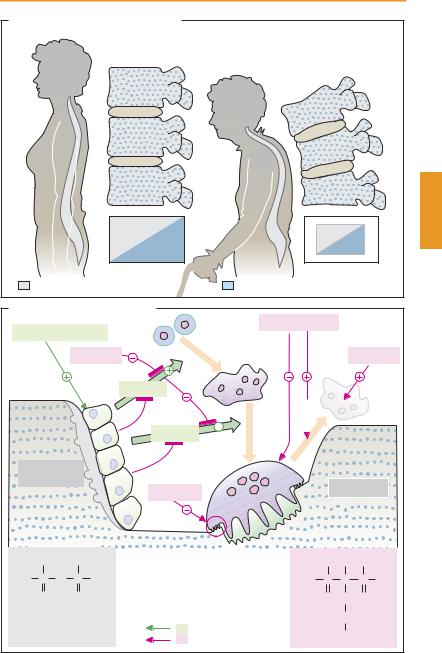
Bone substance is subject to continual remodeling. The equilibrium between bone formation and bone resorption is regulated in a complex manner: a remodeling cycle is initiated by osteoblasts when these stimulate uninucleated osteoclast precursor cells to fuse into large multinucleated cells. Stimulation occurs by direct cell-to-cell contact between osteoblasts and osteoclast precursor cells and is mediated by the RANK ligand on the surface of osteoblasts and its receptor on the osteoclasts (or their precursors), as well as cytokines secreted by osteoblasts. These processes are inhibited by estrogens and a protein secreted by osteoblasts (osteoprotegerin). The osteoclast creates an acidic milieu, enabling minerals to be solubilized, and then phagocytoses the organic matrix. Hormones regulate these events.
In hypocalcemia, the parathyroid increases its secretion of parathormone, resulting in enhanced liberation of Ca2+. Calcitonin transfers active osteoclasts into a resting state. Calcitonin given therapeutically relieves pain associated with neoplastic bone metastases and vertebral body collapse. Estrogens diminish bone resorption by (a) inhibiting activation of osteoclasts by osteoblasts and (b) promoting apoptosis of osteoclasts.
Idiopathic osteoporosis cannot be prevented by prophylactic therapy, but its development can be delayed. This requires: a healthy lifestyle with plenty of physical exercise (sports, hiking), daily intake of calcium (1000 mg/day Ca2+) and of vitamin D (1000 IU/day). The same principle holds for postmenopausal osteoporosis. Hormone
replacement therapy in postmenopausal women has not been successful because of an increased incidence of breast cancers, thromboembolism, and other adverse effects (p. 250). Long-term hormone replacement therapy should no longer be carried out.
If osteoporosis has become clinically manifest, attempts can be made at improving the condition by means of drugs, or at least slowing down further deterioration. Besides administration of calcium and vitamin D, the following options are available.
Bisphosphonates (N-containing) structurally mimic endogenous pyrophosphate (see formulae), and like the latter are incorporated into the mineral substance of bone. During phagocytosis of the bone matrix, they are taken up by osteoclasts. There, the N- containing bisphosphonates inhibit prenylation of G-proteins and thus damage the cells. Accordingly, osteoclast activity levels are lowered by alendronate and risedronate, while osteoclast apoptosis is promoted. The result is a reduction in bone resorption and a decreased risk of bone fractures.
Raloxifene exerts an estrogen-like effect on bone, while acting as an estrogen antagonist in the uterus and breast tissue (p. 254). In terms of fracture prophylaxis, its effectiveness appears inferior to that of bisphosphonates. Thromboembolism and edema are reported as adverse effects.
It should also be mentioned that intermittent slight elevation in the plasma concentration of parathormone leads to increased formation of bone substance. The likely explanation is that, under this condition, stimulation of osteoblasts is suf cient to induce synthesis of bone matrix but not strong enough to activate osteoclasts. This strategy is applied therapeutically by administration of a fragment (amino acids 1–34) of recombinant human parathormone (teriparatide, s.c.).
|
Osteoporosis |
331 |
A. Bone: normal state and osteoporosis |
|
|
Normal state |
Osteoporosis |
|
Organic bone matrix |
Bone mineral: hydroxyapatite |
|
B. Regulation of bone remodeling |
|
|
|
|
|
|||||
|
|
|
|
|
Progenitor |
Biphosphonates |
|
|
|
|
Parathyroid hormone |
cells |
|
|
|
|
|
||||
|
|
|
Estrogens |
Fusion |
|
|
|
Estrogens |
||
|
|
|
|
|
|
|
||||
|
|
|
|
|
RANKL |
|
|
|
Apoptosis |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
OPG |
|
|
|
|
|
|
|
|
|
|
RANKL |
|
|
|
|
|
|
|
|
|
|
Activation |
|
|
|
|
|
(Pre)Osteo- |
|
|
OPG |
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|||
blasts |
|
|
|
|
|
|
Osteoclasts |
|||
|
|
|
|
|
Calcitonin |
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
OH |
|
OH |
|
RANK = receptor activating NF-Κ |
-B |
OH OH OH |
|
||
|
|
|
|
|
|
|
|
|
||
HO |
P |
O |
P |
OH |
RANKL = RANK-Ligand |
HO |
P |
C |
P |
OH |
|
O |
|
O |
|
OPG = Osteoprotegerin |
|
O |
CH2 O |
|
|
Pyrophosphate |
|
Bone resorption |
|
|
(CH2)2 |
|
||||
|
Stimulation |
Alendronate |
|
|
||||||
|
|
|
|
|
Inhibition |
|
|
NH2 |
|
|
332 Therapy of Selected Diseases
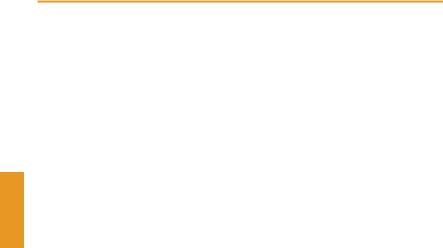
Rheumatoid Arthritis
Rheumatoid arthritis or chronic polyarthritis (A)isaprogressiveinflammatoryjoint disease that intermittently attacks more and more joints, predominantly those of the fingers and toes. The probable cause of rheumatoid arthritis is a pathological reaction of the immunesystem.Thismalfunctioncanbepromoted or triggered by various conditions, including genetic disposition, age-related wear and tear, hypothermia, and infection. An initialnoxiousstimuluselicitsan inflammation of synovial membranes that, in turn, leads to release of antigens through which the inflammatory process is maintained.
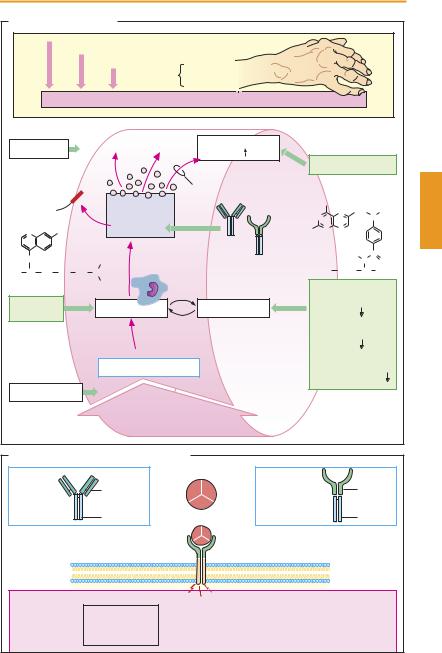
The antigen is taken up by synovial anti- gen-presenting cells; lymphocytes, including T-helper cells (p. 304), are activated and start to proliferate. In the process of interaction between lymphocytes and macrophages, the intensity of inflammation increases. Macrophages release proinflammatory messengers; among these, interleukin-1 and tumor necrosis factor α (TNFα) are important. TNFαis able to elicit a multiplicity of proinflammatory actions (B) that benefit defense against infectious pathogens but are detrimental in rheumatoid arthritis. The cytokines stimulate gene expression for COX- 2; inflammation-promoting prostanoids are produced. The inflammatory reaction increases activity of lymphocytes and macrophages, initiating a vicious circle. Synovial fibroblasts proliferate and release destructive enzymes; the inflamed characteristic pannus tissue develops and destructively invades joint cartilage and subjacent bone. Ultimately, ankylosis (loss of joint motion or bone fusion) with connective tissue scar formation occurs. Concomitant extra-articular disease may be superimposed. The disease process is associated with strong pain and restriction of mobility.
Pharmacotherapy. Acute relief of inflammatory symptoms can be achieved by prostaglandin synthase inhibitors (p. 200; nonse-
lective COX inhibitors or COX-2 inhibitors) and by glucocorticoids (p. 244). The inevitably chronic use of both groups of substances is likely to cause significant adverse effects. Neither can halt the progressive destruction of joints.
Substances that are able to reduce the requirement for nonsteroidal anti-inflam- matory drugs and to slow disease progression are labeled disease-modifying agents. Early use of these drugs is recommended. Their effect develops only after treatment for several weeks. Proliferation of lympho-
cytes can be slowed by |
methotrexate |
(p. 304) and leflunomide, |
which reduces |
the availability of pyrimidine nucleotides in lymphocytes (via inhibition of dihydroorotate dehydrogenase). For ciclosporin, see p. 306. In addition, use is made of immune suppressants such as azathioprine and cyclophosphamide. Intralysosomal accumulation and impaired phagocytic function may be involved in the action of chloroquine or hydroxychloroquine, as well as gold compounds (i.m.: aurothioglucose or aurothiomalate; oral: auranofin, less effective). The antibodies, infliximab and adalimumab, as well as the fusion protein etanercept intercept TNF-αmolecules, preventing them from interacting with membrane receptors of target cells. Anakinra is a recombinant analogue of the endogenous interleukin-1 antagonist. The mechanisms of action of D-pen- icillamine and sulfasalazine are unknown. Same of the drugs mentioned possess considerable potential for adverse effects. Sulfasalazine and methotrexate exhibit a relatively favorable risk–benefit ratio. Combination of disease-modifying drugs is possible.
Surgical removal of the inflamed synovial membrane (synovectomy) frequently provides long-term relief. If feasible, this approach is preferred because all pharmacotherapeutic measures entail significant adverse effects.
|
|
|
|
Rheumatoid Arthritis |
|
|
333 |
|||
A. Rheumatoid Arthritis |
|
|
|
|
|
|
|
|||
|
Genetic predisposition |
|
|
|
|
|
|
|
||
|
|
|
Environmental factors |
|
|
|
|
|
|
|
|
|
|
Precipitating |
Infection |
|
|
|
|
|
|
|
|
|
causes |
Trauma |
|
|
|
|
|
|
|
|
|
Immune system: reactive against autologous joint tissue |
|
|
|
|
|
||
Sulfasalazine |
|
? |
Prostaglandin |
|
|
|
|
|
||
|
synthesis |
|
|
|
|
|
|
|||
|
|
|
|
|
|
COX inhibitors |
||||
IL-1 receptor |
|
|
Cox-2 |
|
|
|
|
|
|
|
Anakinra |
|
|
Cytokines, etc. |
|
|
NH2 |
|
|
|
|
|
|
|
|
|
N |
CH2 N |
CH3 |
|||
|
|
|
IL-1, TNFα |
|
N |
|
||||
N |
Cl |
|
Infliximab |
H2N |
N |
N |
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
Methotrexate |
|
|
||||
|
|
|
|
|
|
|
||||
NH |
|
|
|
Etanercept |
|
|
H |
C |
|
|
|
|
C2H5 |
|
|
|
N |
O |
|||
H3C CH CH2 CH2 CH2 N |
|
HOOC |
(CH2)2 |
CH |
COOH |
|||||
Chloroquine |
|
|
C2H5 |
|
ÐMethotrexate |
|||||
|
|
|
|
|
||||||
Gold, |
|
? |
Macrophages |
Lymphocytes |
(purine |
|
|
|
||
|
synthesis |
) |
|
|||||||
chloroquine |
|
|||||||||
|
|
|
ÐLeflunomide |
|
||||||
|
|
|
|
|
|
|||||
|
|
|
|
|
|
(pyrimidine |
|
|||
|
|
|
|
|
|
synthesis |
) |
|
||
|
|
|
|
|
ÐCiclosporin |
|
||||
|
|
|
Antigen (unknown) |
|
|
(IL-2 synthesis |
||||
|
|
|
|
|
|
in T-helper cells ) |
||||
D-Penicillamine |
|
? |
|
|
|
|
|
|
|
|
B. Tumor necrosis factor α and inhibitors |
|
|
|
|
|
|
||||
|
|
|
Homotrimer |
|
|
|
|
TNF α |
|
|
|
|
|
Murine |
|
|
|
|
|
|
|
Infliximab |
|
|
portion (Fab) |
TNF α |
Etanercept |
|
|
|
receptor- |
|
|
|
|
|
|
|
parts |
||||
(chimeric |
|
|
Human |
|
(fusion protein) |
|
|
|
||
|
|
|
|
|
|
|
|
|||
IgG antibody) |
|
|
|
|
|
|
|
|
||
|
portion (Fc) |
|
|
|
|
|
Fc portion |
|||
|
|
|
|
|
|
|
|
|||
|
|
|
|
TNF α |
|
|
|
|
|
|
|
|
|
|
receptor |
|
|
|
|
|
|
|
|
|
Activation |
|
|
|
|
|
|
|
|
|
Vessels: |
|
|
|
|
|
|
Tumor cells |
|
Ð Proliferation |
|
Macrophages: |
|
Synovial membrane: |
|
Bone: |
|
|
Ð Activation |
|
Ð Proliferation |
|
|||
Ð Lysis |
|
Ð Adhesion of |
|
|
|
Ð Resorption |
||
|
|
Ð Chemotaxis |
|
Ð Pannus formation |
|
|||
|
|
blood cells |
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
