
- •Preface to the 3rd edition
- •General Pharmacology
- •Systems Pharmacology
- •Therapy of Selected Diseases
- •Subject Index
- •Abbreviations
- •General Pharmacology
- •History of Pharmacology
- •Drug and Active Principle
- •The Aims of Isolating Active Principles
- •European Plants as Sources of Effective Medicines
- •Drug Development
- •Congeneric Drugs and Name Diversity
- •Oral Dosage Forms
- •Drug Administration by Inhalation
- •Dermatological Agents
- •From Application to Distribution in the Body
- •Potential Targets of Drug Action
- •External Barriers of the Body
- •Blood–Tissue Barriers
- •Membrane Permeation
- •Binding to Plasma Proteins
- •The Liver as an Excretory Organ
- •Biotransformation of Drugs
- •Drug Metabolism by Cytochrome P450
- •The Kidney as an Excretory Organ
- •Presystemic Elimination
- •Drug Concentration in the Body as a Function of Time—First Order (Exponential) Rate Processes
- •Time Course of Drug Concentration in Plasma
- •Time Course of Drug Plasma Levels during Repeated Dosing (A)
- •Time Course of Drug Plasma Levels during Irregular Intake (B)
- •Accumulation: Dose, Dose Interval, and Plasma Level Fluctuation (A)
- •Dose–Response Relationship
- •Concentration–Effect Curves (B)
- •Concentration–Binding Curves
- •Types of Binding Forces
- •Agonists—Antagonists
- •Other Forms of Antagonism
- •Enantioselectivity of Drug Action
- •Receptor Types
- •Undesirable Drug Effects, Side Effects
- •Drug Allergy
- •Cutaneous Reactions
- •Drug Toxicity in Pregnancy and Lactation
- •Pharmacogenetics
- •Placebo (A)
- •Systems Pharmacology
- •Sympathetic Nervous System
- •Structure of the Sympathetic Nervous System
- •Adrenergic Synapse
- •Adrenoceptor Subtypes and Catecholamine Actions
- •Smooth Muscle Effects
- •Cardiostimulation
- •Metabolic Effects
- •Structure–Activity Relationships of Sympathomimetics
- •Indirect Sympathomimetics
- •Types of
- •Antiadrenergics
- •Parasympathetic Nervous System
- •Cholinergic Synapse
- •Parasympathomimetics
- •Parasympatholytics
- •Actions of Nicotine
- •Localization of Nicotinic ACh Receptors
- •Effects of Nicotine on Body Function
- •Aids for Smoking Cessation
- •Consequences of Tobacco Smoking
- •Dopamine
- •Histamine Effects and Their Pharmacological Properties
- •Serotonin
- •Vasodilators—Overview
- •Organic Nitrates
- •Calcium Antagonists
- •ACE Inhibitors
- •Drugs Used to Influence Smooth Muscle Organs
- •Cardiac Drugs
- •Cardiac Glycosides
- •Antiarrhythmic Drugs
- •Drugs for the Treatment of Anemias
- •Iron Compounds
- •Prophylaxis and Therapy of Thromboses
- •Possibilities for Interference (B)
- •Heparin (A)
- •Hirudin and Derivatives (B)
- •Fibrinolytics
- •Intra-arterial Thrombus Formation (A)
- •Formation, Activation, and Aggregation of Platelets (B)
- •Inhibitors of Platelet Aggregation (A)
- •Presystemic Effect of ASA
- •Plasma Volume Expanders
- •Lipid-lowering Agents
- •Diuretics—An Overview
- •NaCl Reabsorption in the Kidney (A)
- •Aquaporins (AQP)
- •Osmotic Diuretics (B)
- •Diuretics of the Sulfonamide Type
- •Potassium-sparing Diuretics (A)
- •Vasopressin and Derivatives (B)
- •Drugs for Gastric and Duodenal Ulcers
- •Laxatives
- •Antidiarrheal Agents
- •Drugs Affecting Motor Function
- •Muscle Relaxants
- •Nondepolarizing Muscle Relaxants
- •Depolarizing Muscle Relaxants
- •Antiparkinsonian Drugs
- •Antiepileptics
- •Pain Mechanisms and Pathways
- •Eicosanoids
- •Antipyretic Analgesics
- •Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- •Cyclooxygenase (COX) Inhibitors
- •Local Anesthetics
- •Opioid Analgesics—Morphine Type
- •General Anesthesia and General Anesthetic Drugs
- •Inhalational Anesthetics
- •Injectable Anesthetics
- •Sedatives, Hypnotics
- •Benzodiazepines
- •Pharmacokinetics of Benzodiazepines
- •Therapy of Depressive Illness
- •Mania
- •Therapy of Schizophrenia
- •Psychotomimetics (Psychedelics, Hallucinogens)
- •Hypothalamic and Hypophyseal Hormones
- •Thyroid Hormone Therapy
- •Glucocorticoid Therapy
- •Follicular Growth and Ovulation, Estrogen and Progestin Production
- •Oral Contraceptives
- •Antiestrogen and Antiprogestin Active Principles
- •Aromatase Inhibitors
- •Insulin Formulations
- •Treatment of Insulin-dependent Diabetes Mellitus
- •Treatment of Maturity-Onset (Type II) Diabetes Mellitus
- •Oral Antidiabetics
- •Drugs for Maintaining Calcium Homeostasis
- •Drugs for Treating Bacterial Infections
- •Inhibitors of Cell Wall Synthesis
- •Inhibitors of Tetrahydrofolate Synthesis
- •Inhibitors of DNA Function
- •Inhibitors of Protein Synthesis
- •Drugs for Treating Mycobacterial Infections
- •Drugs Used in the Treatment of Fungal Infections
- •Chemotherapy of Viral Infections
- •Drugs for the Treatment of AIDS
- •Drugs for Treating Endoparasitic and Ectoparasitic Infestations
- •Antimalarials
- •Other Tropical Diseases
- •Chemotherapy of Malignant Tumors
- •Targeting of Antineoplastic Drug Action (A)
- •Mechanisms of Resistance to Cytostatics (B)
- •Inhibition of Immune Responses
- •Antidotes and Treatment of Poisonings
- •Therapy of Selected Diseases
- •Hypertension
- •Angina Pectoris
- •Antianginal Drugs
- •Acute Coronary Syndrome— Myocardial Infarction
- •Congestive Heart Failure
- •Hypotension
- •Gout
- •Obesity—Sequelae and Therapeutic Approaches
- •Osteoporosis
- •Rheumatoid Arthritis
- •Migraine
- •Common Cold
- •Atopy and Antiallergic Therapy
- •Bronchial Asthma
- •Emesis
- •Alcohol Abuse
- •Local Treatment of Glaucoma
- •Further Reading
- •Further Reading
- •Picture Credits
- •Drug Indexes

244 Hormones
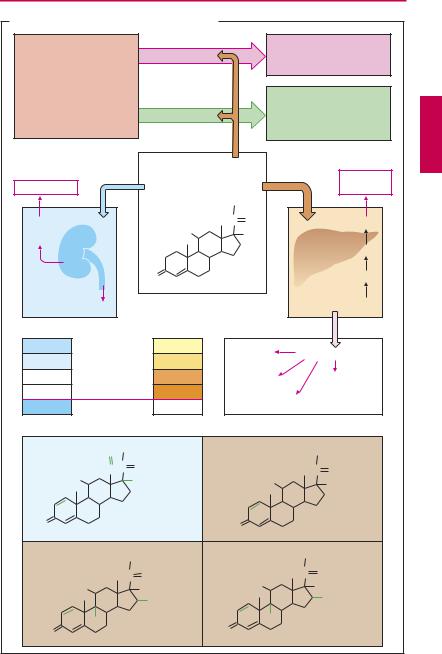
Glucocorticoid Therapy
I. Replacement Therapy
The adrenal cortex (AC) produces the glucocorticoid cortisol (hydrocortisone) in the zona fasciculata and the mineralocorticoid aldosterone in the zona glomerulosa. Both steroid hormones are vitally important in adaptation responses to stress situations, such as disease, trauma, or surgery. Cortisol secretion is stimulated by hypophyseal ACTH; aldosterone secretion by angiotensin II in particular (p.128). In AC failure (primary adrenocortical insuf ciency; Addison disease), both cortisol and aldosterone must be replaced; when ACTH production is deficient (secondary adrenocortical insuf ciency), cortisol alone needs to be replaced. Cortisol is effective when given orally (30 mg/day, 2/3 a.m., 1/3 p.m.). Instresssituations,thedoseis raised 5- to 10-fold. Aldosterone is poorly effective via the oral route; instead, the mineralocorticoid fludrocortisone (0.1 mg/day) is given.
II. Pharmacodynamic Therapy with Glucocorticoids (A)
In unphysiologically high concentrations, cortisol or other glucocorticoids suppress all phases (exudation, proliferation, scar formation) of the inflammatory reaction, i.e., the organism’s defensive measures against foreign or noxious matter. This effect is mediated by multiple components, all of which involve alterations in gene transcription (p.64) Thus, synthesis of the anti-in- flammatory protein lipocortin (macrocortin) is stimulated. Lipocortin inhibits the enzyme phospholipase A2. Consequently, release of arachidonic acid is diminished, along with the formation of inflammatory mediators of the prostaglandin and leukotriene series (pp.196, 200). Conversely, glucocorticoids inhibit synthesis of several proteins that participate in the inflammatory process, including interleukins (p.304) and other cytokines, phospholipase A2 (p.196), and cyclooxyge- nase-2 (p.200). At very high dosage, non-
genomic effects via membrane-bound receptors may also contribute.
Desired effects. As antiallergics, immunosuppressants, or anti-inflammatory drugs, glucocorticoids display excellent ef cacy against “undesired” inflammatory reactions, such as allergy, rheumatoid arthritis, etc.
Unwanted effects. With short-term use, glucocorticoids are practically free of adverse effects, even at the highest dosage. Longterm use islikelytocausechangesmimicking thesignsofCushing syndrome (endogenous overproduction of cortisol). Sequelae of the anti-inflammatory action are lowered resistancetoinfectionanddelayedwoundhealing. Sequelaeofexaggeratedglucocorticoidaction are(a)increasedgluconeogenesisandrelease of glucose, insulin-dependent conversion of glucosetotriglycerides(adipositymainlynoticeableintheface,neck,andtrunk),and“ste- roid-diabetes”ifinsulinreleaseisinsuf cient; (b)increasedproteincatabolismwithatrophy ofskeletalmusculature(thinextremities),osteoporosis,growthretardationininfants,and skin atrophy. Sequelae of the intrinsically weak, but now manifest, mineralocorticoid action of cortisol are salt and fluid retention, hypertension, edema; and KCl loss with danger of hypokalemia. Psychic changes, chiefly intheformofeuphoricormanicmoodswings, also need to be taken into account during chronic intakeofglucocorticoids.
Measures for attenuating or preventing drug-induced Cushing syndrome. (a) Use of cortisol derivatives with less (e.g., prednisolone) or negligible mineralocorticoid activity (e.g., triamcinolone, dexamethasone). Glucocorticoid activity of these congeners is more pronounced. Glucocorticoid, anti-inflammatory, and feedback-inhibitory (p.246) actions on the hypophysis are correlated. An exclusively anti-inflammatory congener does not exist. The “glucocorti- coid”-related Cushinglike symptoms cannot be avoided. The table opposite lists relative
|
|
|
|
|
|
|
Glucocorticoid Therapy |
245 |
||||
A. Glucocorticoids: principal and adverse effects |
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
e.g., allergy |
|
||
|
Inflammation |
|
Unwanted |
|
|
|
autoimmune disease, |
|
||||
|
|
|
|
|
|
|
|
|
transplant rejection |
|
||
|
redness, |
|
|
|
|
|
|
|
|
|
|
|
|
swelling heat, |
|
|
|
|
|
|
|
|
|
|
|
|
pain; |
|
|
|
|
|
|
|
Healing of |
|
||
|
scar |
|
|
Wanted |
|
|
|
tissue injury |
|
|||
|
|
|
|
|
|
|
due to bacteria, |
|
||||
|
|
|
|
|
|
|
|
|
viruses, fungi, trauma |
|
||
|
|
Mineralocorticoid |
|
|
|
|
|
Glucocorticoid |
|
|||
|
|
action |
|
|
Unphysiologically |
|
|
|
action |
|
|
|
|
|
|
|
|
high concentration |
|
|
|
|
Diabetes |
|
|
|
Hypertension |
|
|
|
|
|
|
|
|
mellitus |
|
|
|
|
|
|
|
Cortisol |
|
CH2OH |
|
|
|
|
|
|
Na+ |
|
|
|
HO |
|
C |
O |
|
|
Glucose |
|
|
H2O |
|
|
|
|
|
OH |
|
|
|
|
|
|
|
|
|
|
|
|
|
Gluconeogenesis |
|
|||
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
O |
|
|
|
|
|
Amino acids |
|
|
|
K+ |
|
|
|
|
|
|
Protein catabolism |
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1 |
Cortisol |
|
1 |
|
Muscle |
Tissue atrophy |
|
||||
|
0.8 |
Prednisolone |
|
4 |
|
weakness |
|
|||||
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
||||
Potency |
0 |
Triamcinolone |
|
7.5 |
|
Osteo- |
|
|
Skin |
|
||
0 |
Dexamethasone |
30 |
|
porosis |
|
|
atrophy |
|
||||
|
|
|
|
|
|
|
||||||
3000 |
Aldosterone |
|
0.3 |
|
Growth inhibition |
|
|
|
||||
|
|
O CH2OH |
|
|
|
|
|
CH2OH |
|
|||
|
|
HC C |
O |
|
|
|
|
|
|
C |
O |
|
|
|
HO |
H |
|
|
|
|
HO |
|
OH |
|
|
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
O |
|
Aldosterone |
|
O |
|
|
|
Prednisolone |
|
||
|
|
|
|
|
|
|
|
|||||
|
|
|
CH2OH |
|
|
|
CH2OH |
|
||||
|
|
|
C |
O |
|
|
|
C |
O |
|
||
|
|
|
|
|
HO |
|
|
|
|
|||
|
|
HO |
OH |
|
|
|
OH |
|
||||
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
CH3 |
|
|||
|
|
|
|
|
OH |
|
|
|
|
|
|
|
|
|
F |
|
|
|
|
|
F |
|
|
|
|
|
|
|
|
|
O |
|
|
|
|
|
|
|
|
O |
|
Triamcinolone |
|
|
|
Dexamethasone |
|
||||
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|||||

246 Hormones
activity (potency) with reference to cortisol, whose mineralocorticoid and glucocorticoid activities are assigned a value of 1.0. All listed glucocorticoids are effective orally.
(b) Local application. This enables therapeutically effective concentrations to be built up at the site of application without a correspondingsystemicexposure. Glucocorticoids that are subject to rapid biotransformation and inactivation following diffusion from the site of action are the preferred choice. Thus, inhalational administration employs glucocorticoids with a high presystemic elimination such as beclomethasone dipropionate, budesonide, flunisolide, or fluticasonepropionate(p.14).Adverseeffects,however,alsooccurlocally:e.g.,withinhalational use, oropharyngeal candidiasis (thrush) and hoarseness; with cutaneous use, skin atrophy, striae, telangiectasias and steroid acne; and with ocular use, cataracts and increased intraocular pressure (glaucoma).
(c) Lowest dosage possible. For long-term medication, a just-suf cient dose should be given. However, in attempting to lower the dose to the minimally effective level, it is necessary to take into account that administration of exogenous glucocorticoids will suppress production of endogenous cortisol owing to activation of an inhibitory feedback mechanism. In this manner, a very low dose could be “buffered,” so that unphysiologically high glucocorticoid activity and the anti-inflammatoryeffect arebothprevented.
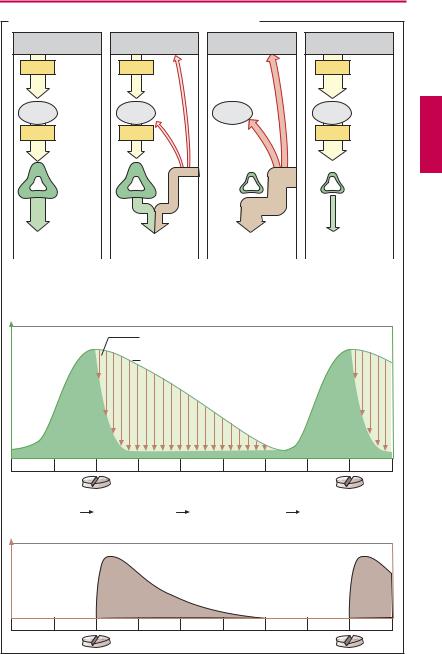
Effect of glucocorticoid administration on adrenocortical cortisol production (A). Release of cortisol depends on stimulation by hypophyseal ACTH, which in turn is controlled by hypothalamic corticotropin-re- leasing hormone (CRH). In both in the hypophysis and hypothalamus there are cortisol receptors through which cortisol can exert a feedback inhibition of ACTH or CRH release. By means of these cortisol “sensors,” the regulatory centers can monitor whether the actual blood level of the hormone corresponds to the “set-point.” If the blood level
exceeds the set-point, ACTH output is decreased and thus also the cortisol production. In this way, cortisol level is maintained within the required range. The regulatory centers respond to synthetic glucocorticoids as they do to cortisol. Administration of exogenous cortisol or any other glucocorticoid reduces the amount of endogenous cortisol needed to maintain homeostasis. Release of CRH and ACTH declines (“inhibition of higher centers by exogenous glucocorticoid”) and, hence, cortisol secretion (“adrenocortical suppression”). After weeks of exposure tounphysiologically high glucocorticoid doses, the cortisol-producing portions of the adrenal cortex shrink (“adrenocortical atrophy”). Aldosterone-synthesizing capacity remains unaffected, however. When glucocorticoid medication is suddenly withheld, the atrophic cortex is unable to produce suf cient cortisol and a potentially lifethreatening cortisol deficiency may develop. Therefore, glucocorticoid therapy should always be tapered off by gradual reduction of the dosage.
Regimens for prevention of adrenocortical atrophy. Cortisol secretion is high in the early morning and low in the late evening (circadian rhythm). Accordingly, sensitivity to feedback inhibition must be high in the late evening.
(a)Circadian administration: The daily dose of glucocorticoid is given in the morning. Endogenous cortisol production will already have begun, the regulatory centers being relatively insensitive to inhibition. In theearlymorning hoursof thenextday, CRF/ ACTH release and adrenocortical stimulation will resume.
(b)Alternate day therapy: Twice the daily dose is given on alternate mornings. On the “off” day, endogenous cortisol production is allowed to occur.
The disadvantage with either regimen is a recrudescence of disease symptoms during the glucocorticoid-free interval.
|
|
|
|
|
Glucocorticoid Therapy |
|
247 |
||
A. Cortisol release and its modification by glucocorticoids |
|
|
|
|
|||||
Hypothalamus |
|
|
|
|
|
|
|
|
|
CRH |
|
|
|
|
|
|
|
|
|
|
Hypo- |
|
|
|
|
|
|
|
|
|
physis |
|
|
|
|
|
|
|
|
ACTH |
|
|
|
|
Adreno- |
|
|
|
|
|
|
|
|
|
cortical |
|
|
|
|
|
|
|
|
|
atrophy |
|
|
|
|
|
Adrenal |
|
|
|
|
|
|
|
|
|
cortex |
|
|
|
|
|
|
|
|
Cortisol |
|
|
|
Exogenous |
|
|
|
|
|
|
|
|
admini- |
|
|
|
|
|
|
30 mg/day |
|
|
stration |
|
|
|
|
|
|
Cortisol |
|
|
Decrease in |
|
Cessation of |
|
Cortisol deficiency |
||
production under |
|
cortisol production |
cortisol production |
after abrupt |
|
||||
normal |
|
|
with cortisol dose |
with cortisol dose |
cessation of |
|
|
||
conditions |
|
|
< daily production |
> daily production |
administration |
|
|||
Cortisol |
|
|
Glucocorticoid-induced |
|
|
|
|
||
concentration |
|
inhibition of cortisol production |
|
|
|
|
|||
|
|
|
normal circadian time-course |
|
|
|
|
||
0 |
4 |
8 |
12 |
16 |
20 |
24 |
4 |
8 |
h |
Morning dose |
Inhibition of |
|
Elimination of |
|
Start of early |
|
|||
|
|
endogenous |
|
exogenous |
|
morning |
|
|
|
|
|
cortisol |
|
glucocorticoid |
|
cortisol |
|
|
|
|
|
production |
|
during daytime |
|
production |
|
|
|
Glucocorticoid |
|
|
|
|
|
|
|
|
|
concentration |
|
|
|
|
|
|
|
|
|
0 |
4 |
8 |
12 |
16 |
20 |
24 |
4 |
8 |
h |

248 Hormones
|
Androgens, Anabolic Steroids, |
|
Orally active mesterolone is 1-α-methyldi- |
||
|
Antiandrogens |
|
|
|
hydrotestosterone. |
|
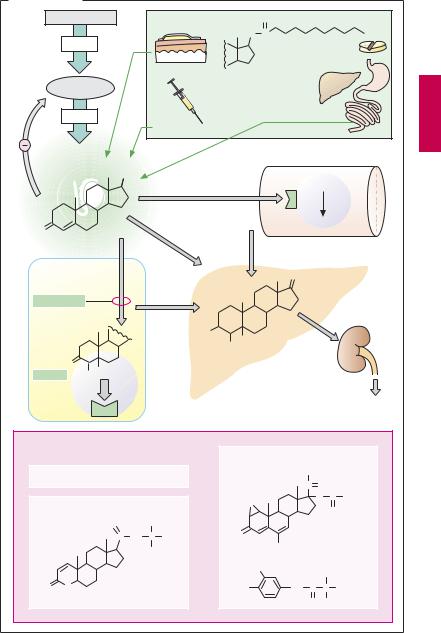
Androgens are masculinizing substances. |
Indication: for hormone replacement in |
|||
|
deficiency of endogenous T. production. |
||||
|
The endogenous male gonadal hormone is |
||||
|
Anabolics are testosterone derivatives |
||||
|
the steroid testosterone from the interstitial |
||||
|
(e.g.,clostebol,metenolone,nandrolone,sta- |
||||
|
Leydig cells of the testis. Testosterone secre- |
||||
|
nozolol) that are used in debilitated patients, |
||||
|
tion is stimulated by hypophyseal luteinizing |
||||
|
and are misused by athletes, because of their |
||||
|
hormone (LH), whose release is controlled |
||||
|
protein anabolic effect. They act via stimula- |
||||
|
by hypothalamic |
GnRH |
(gonadorelin, |
||
|
tion of androgen receptors and, thus, also |
||||
|
p.238). Release of both hormones is subject |
||||
|
display androgenic actions (e.g., virilization |
||||
|
to feedback inhibition by circulating testo- |
||||
|
in females, suppression of spermatogenesis). |
||||
|
sterone. Reduction of testosterone to dihy- |
||||
|
|
||||
|
drotestosterone occurs in most target organs |
Inhibitory Principles |
|||
|
(e.g., the prostate gland); |
the latter |
pos- |
||
|
GnRH superagonists (p.238), such as buser- |
||||
|
sesses higher af nity for androgen receptors. |
||||
|
elin, leuprolin, goserelin, and triptorelin, are |
||||
|
Rapid intrahepatic |
degradation (plasma |
|||
|
|
||||
t½~ 15 minutes) yields androsterone among |
used in patients with metastasizing prostate |
|
cancer to inhibit production of testosterone |
||
other metabolites (17-ketosteroids) that are |
||
which promotes tumor growth. Following a |
||
eliminated as conjugates in the urine. Be- |
||
transient stimulation, gonadotropin release |
||
cause of rapid hepatic metabolism, testoster- |
||
subsides within a few days and testosterone |
||
one is unsuitable for oral use. Although it is |
||
levels fall as low as after surgical removal of |
||
well absorbed, it undergoes virtually com- |
||
the testes. |
||
plete presystemic elimination. |
||
|
Testosterone (T.) derivatives for clinical use. Because of its good tissue penetrability, testosterone is well suited for percutaneous administration in the form of a patch (transdermal delivery system, p.18). T. esters for i. m. depot injection are T. propionate and T. heptanoate (or enanthate). These are given in oily solution by deep intramuscular injection. Upon diffusion of the ester from the depot, esterases quickly split off the acyl residue to yield free T. With increasing lipophilicity, esters will tend to remain in the depot, and the duration of action therefore lengthens. A T. ester for oral use is the undecanoate. Owing to the fatty acid nature of undecanoic acid, this ester is absorbed into the lymph, enabling itto bypass the liver and enter the general circulation via the thoracic duct. 17-α Methyltestosterone is effective by the oral route owing to its increased metabolic stability, but because of the hepatotoxicityof C17-alkylated androgens(cholestasis, tumors) its use should be avoided.
Androgen receptor antagonists. The antiandrogen cyproterone is a competitive antagonist of testosterone. By virtue of an additional progestin action, it decreases secretion of gonadotropins. Indications: in the male, dampening of sexual drive in hypersexuality, prostatic cancer; in the female, treatment of virilization phenomena, if necessary, with concomitant utilization of the gestagen contraceptive effect.
Flutamide and bicalutamide are structurally different androgen receptor antagonists lacking progestin activity.
Finasteride and dutasteride inhibit 5α- reductase, the enzyme responsible for converting T. to dihydrotestosterone (DHT). Thus, androgenic stimulation is reduced in those tissues where DHT is the active species (e.g., the prostate). T.-dependent tissues and functions are not or hardly affected: e.g., skeletal musculature, feedback inhibition of gonadotropin release, or libido. Both can be used in benign prostatic hyperplasia to shrink the gland and to improve micturition.
Androgens, Anabolic Steroids, Antiandrogens |
249 |
A. Testosterone |
|
|
|
|
|
|
|
|
|
|
Hypothalamus |
|
|
Substitution |
|
|
O |
|
|
|
|
|
|
|
|
|
|
O |
C |
|
|
|
|
GnRH |
|
|
|
|
|
Testosterone |
|
p.o. |
|
|
|
|
|
|
|
|
undecanoate |
|
|
|
|
|
|
|
transdermal |
|
|
|
|
|
|
Hypophysis |
|
|
|
|
|
|
|
|
|
|
|
LH |
|
|
i.m. |
|
|
Intestinal lymph |
|||
|
|
|
|
Testosterone ester |
|
|
|
|
|
|
Testosterone |
|
|
|
|
|
e.g., skeletal muscle fiber |
||||
|
|
|
|
|
|
|
|
|
||
|
OH |
|
|
|
|
Androgen receptor |
||||
|
|
|
|
|
|
|
||||
O |
|
|
|
|
|
|
Gene expression |
|||
|
|
|
|
|
|
|
|
|
|
|
e.g., Prostatic |
|
|
|
|
|
O |
|
|
|
|
gland cell |
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
Conjugation with |
|||
|
|
|
|
|
|
|
|
|
||
5α -Reductase |
|
|
|
|
|
|
|
sulfate, glucuronate |
||
|
|
|
|
HO |
|
H |
|
|
|
|
|
|
|
|
|
H |
|
|
|
|
|
|
O |
|
|
|
Androsterone |
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
Dihydro- |
H H |
|
|
|
|
|
|
|
|
|
testosterone |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
17-Keto- |
|
|
|
|
|
|
|
|
|
|
steroid |
I n h i b i t o r y P r i n c i p l e s |
|
Receptor antagonists |
||||||||
|
|
|
|
|
|
|||||
|
GnRH superagonists |
|
|
|
|
|
CH3 |
|
||
|
|
|
|
|
|
C |
O |
|
||
|
|
|
|
|
|
|
|
|
||
5α -Reductase inhibitor |
|
|
H2C |
|
|
O C |
CH3 |
|||
|
|
|
|
O |
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
O |
|
CH3 |
|
|
|
Cyproterone |
|||
|
C |
NH |
C |
CH3 |
|
O |
|
|||
|
|
Cl |
acetate |
|||||||
|
|
|
CH3 |
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
F3C |
Flutamide |
CH3 |
||
|
|
|
|
|
|
|
|
|
||
O |
N |
Finasteride |
O2N |
NH |
C |
C |
H |
|||
|
H |
|
|
|
O |
CH3 |
||||
|
|
|
|
|
|
|
|
|||
