
- •Preface to the 3rd edition
- •General Pharmacology
- •Systems Pharmacology
- •Therapy of Selected Diseases
- •Subject Index
- •Abbreviations
- •General Pharmacology
- •History of Pharmacology
- •Drug and Active Principle
- •The Aims of Isolating Active Principles
- •European Plants as Sources of Effective Medicines
- •Drug Development
- •Congeneric Drugs and Name Diversity
- •Oral Dosage Forms
- •Drug Administration by Inhalation
- •Dermatological Agents
- •From Application to Distribution in the Body
- •Potential Targets of Drug Action
- •External Barriers of the Body
- •Blood–Tissue Barriers
- •Membrane Permeation
- •Binding to Plasma Proteins
- •The Liver as an Excretory Organ
- •Biotransformation of Drugs
- •Drug Metabolism by Cytochrome P450
- •The Kidney as an Excretory Organ
- •Presystemic Elimination
- •Drug Concentration in the Body as a Function of Time—First Order (Exponential) Rate Processes
- •Time Course of Drug Concentration in Plasma
- •Time Course of Drug Plasma Levels during Repeated Dosing (A)
- •Time Course of Drug Plasma Levels during Irregular Intake (B)
- •Accumulation: Dose, Dose Interval, and Plasma Level Fluctuation (A)
- •Dose–Response Relationship
- •Concentration–Effect Curves (B)
- •Concentration–Binding Curves
- •Types of Binding Forces
- •Agonists—Antagonists
- •Other Forms of Antagonism
- •Enantioselectivity of Drug Action
- •Receptor Types
- •Undesirable Drug Effects, Side Effects
- •Drug Allergy
- •Cutaneous Reactions
- •Drug Toxicity in Pregnancy and Lactation
- •Pharmacogenetics
- •Placebo (A)
- •Systems Pharmacology
- •Sympathetic Nervous System
- •Structure of the Sympathetic Nervous System
- •Adrenergic Synapse
- •Adrenoceptor Subtypes and Catecholamine Actions
- •Smooth Muscle Effects
- •Cardiostimulation
- •Metabolic Effects
- •Structure–Activity Relationships of Sympathomimetics
- •Indirect Sympathomimetics
- •Types of
- •Antiadrenergics
- •Parasympathetic Nervous System
- •Cholinergic Synapse
- •Parasympathomimetics
- •Parasympatholytics
- •Actions of Nicotine
- •Localization of Nicotinic ACh Receptors
- •Effects of Nicotine on Body Function
- •Aids for Smoking Cessation
- •Consequences of Tobacco Smoking
- •Dopamine
- •Histamine Effects and Their Pharmacological Properties
- •Serotonin
- •Vasodilators—Overview
- •Organic Nitrates
- •Calcium Antagonists
- •ACE Inhibitors
- •Drugs Used to Influence Smooth Muscle Organs
- •Cardiac Drugs
- •Cardiac Glycosides
- •Antiarrhythmic Drugs
- •Drugs for the Treatment of Anemias
- •Iron Compounds
- •Prophylaxis and Therapy of Thromboses
- •Possibilities for Interference (B)
- •Heparin (A)
- •Hirudin and Derivatives (B)
- •Fibrinolytics
- •Intra-arterial Thrombus Formation (A)
- •Formation, Activation, and Aggregation of Platelets (B)
- •Inhibitors of Platelet Aggregation (A)
- •Presystemic Effect of ASA
- •Plasma Volume Expanders
- •Lipid-lowering Agents
- •Diuretics—An Overview
- •NaCl Reabsorption in the Kidney (A)
- •Aquaporins (AQP)
- •Osmotic Diuretics (B)
- •Diuretics of the Sulfonamide Type
- •Potassium-sparing Diuretics (A)
- •Vasopressin and Derivatives (B)
- •Drugs for Gastric and Duodenal Ulcers
- •Laxatives
- •Antidiarrheal Agents
- •Drugs Affecting Motor Function
- •Muscle Relaxants
- •Nondepolarizing Muscle Relaxants
- •Depolarizing Muscle Relaxants
- •Antiparkinsonian Drugs
- •Antiepileptics
- •Pain Mechanisms and Pathways
- •Eicosanoids
- •Antipyretic Analgesics
- •Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- •Cyclooxygenase (COX) Inhibitors
- •Local Anesthetics
- •Opioid Analgesics—Morphine Type
- •General Anesthesia and General Anesthetic Drugs
- •Inhalational Anesthetics
- •Injectable Anesthetics
- •Sedatives, Hypnotics
- •Benzodiazepines
- •Pharmacokinetics of Benzodiazepines
- •Therapy of Depressive Illness
- •Mania
- •Therapy of Schizophrenia
- •Psychotomimetics (Psychedelics, Hallucinogens)
- •Hypothalamic and Hypophyseal Hormones
- •Thyroid Hormone Therapy
- •Glucocorticoid Therapy
- •Follicular Growth and Ovulation, Estrogen and Progestin Production
- •Oral Contraceptives
- •Antiestrogen and Antiprogestin Active Principles
- •Aromatase Inhibitors
- •Insulin Formulations
- •Treatment of Insulin-dependent Diabetes Mellitus
- •Treatment of Maturity-Onset (Type II) Diabetes Mellitus
- •Oral Antidiabetics
- •Drugs for Maintaining Calcium Homeostasis
- •Drugs for Treating Bacterial Infections
- •Inhibitors of Cell Wall Synthesis
- •Inhibitors of Tetrahydrofolate Synthesis
- •Inhibitors of DNA Function
- •Inhibitors of Protein Synthesis
- •Drugs for Treating Mycobacterial Infections
- •Drugs Used in the Treatment of Fungal Infections
- •Chemotherapy of Viral Infections
- •Drugs for the Treatment of AIDS
- •Drugs for Treating Endoparasitic and Ectoparasitic Infestations
- •Antimalarials
- •Other Tropical Diseases
- •Chemotherapy of Malignant Tumors
- •Targeting of Antineoplastic Drug Action (A)
- •Mechanisms of Resistance to Cytostatics (B)
- •Inhibition of Immune Responses
- •Antidotes and Treatment of Poisonings
- •Therapy of Selected Diseases
- •Hypertension
- •Angina Pectoris
- •Antianginal Drugs
- •Acute Coronary Syndrome— Myocardial Infarction
- •Congestive Heart Failure
- •Hypotension
- •Gout
- •Obesity—Sequelae and Therapeutic Approaches
- •Osteoporosis
- •Rheumatoid Arthritis
- •Migraine
- •Common Cold
- •Atopy and Antiallergic Therapy
- •Bronchial Asthma
- •Emesis
- •Alcohol Abuse
- •Local Treatment of Glaucoma
- •Further Reading
- •Further Reading
- •Picture Credits
- •Drug Indexes

152 Antithrombotics
Intra-arterial Thrombus Formation (A)
Activation of platelets, e.g., upon contact with collagen of the extracellular matrix after injury to the vascular wall, constitutes the immediate and decisive step in initiating the process of primary hemostasis, i.e., cessation of bleeding. However in the absence of vascular injury, platelets can be activated as a result of damage to the endothelial cell lining of blood vessels. Among the multiple functions of the endothelium, the production of prostacyclin and nitric oxide (NO) plays an important role because both substances inhibit the tendency of platelets to adhere to the endothelial surface. Impairment of endothelial function, e.g., due to chronic hypertension, chronic elevation of plasma LDL levels or of blood glucose, and cigarette smoking, increases the probability of adhesion between thrombocytes and endothelium. The deceleration of fast flowing platelets occurs through an interaction between the glycoprotein Ibα (GP I) in the platelet membrane and von Willebrand factor in the endothelium and basal membrane (denuded after endothelial injury). For the proper activation of the platelet, interaction with subendothelial collagen of an additional platelet glycoprotein (GP IV) is necessary. As soon as platelets are activated (see p.154), they change their shape and gain af nity for fibrinogen. Thisresultsfromaconformational change of glycoprotein IIb/IIIa in the platelet membrane. Platelets can now be linked to each other via fibrinogen bridges (A).
Platelet aggregation proceeds like an avalanche because, once activated, one platelet can activate other platelets. On the injured endothelial cell a thrombus is formed, which obstructs blood flow. Ultimately, the vascular lumen is occluded by the thrombusasthe latter is solidified by vasoconstriction promoted by the release of serotonin and thromboxane A2 from the aggregated platelets and by locally activated thrombin. Thrombin plays a twofold part in thrombus
formation: as a protease, thrombin cleaves fibrinogen and thus initiates the formation of fibrin clot (blood coagulation, p.144). The effects of thrombin on platelets and endothelial cells, however, involve a proteolytic activation of receptorscoupled to G-proteins (so-called protease-activated receptors). When these events occur in a larger, functionally important artery, myocardial infarction or stroke may be the result.
Von Willebrand factor plays a key role in thrombogenesis. Lack of this factor is the cause of thrombasthenia, the inability to staunch bleeding by platelet aggregation. A relative deficiency of von Willebrand factor can be transiently relieved by injection of the vasopressin analogue desmopressin, because this substance makes factor available from stored supplies.
Formation, Activation, and Aggregation of Platelets (B)
Platelets are fragments of multicellular megakaryocytes. They constitute the smallest formed elements of blood (diameter 1–4 µm) and, devoid of a cell nucleus, are no longer capable of protein synthesis. Platelets can be activated by various stimuli, leading to:
Change in shape
Conversion of integrin GP IIb/IIIa into its active conformation
Release of active substances such as serotonin, platelet-activating factor (PAF), ADP, and thromboxane A2. All these substances activate other platelets.

Intra-arterial Thrombus Formation |
153 |
A. Thrombogenesis |
|
|
|
|
|
1. Adhesion |
2. Activation |
3. Aggregation |
|||
|
Endothelial defect |
|
|
||
Platelet |
Activated |
von Willebrand |
Collagen |
Fibrinogen |
|
not activated |
platelet |
factor |
|||
|
|
||||
B. Aggregation of platelets by the integrin GPIIb/IIIa |
|
Megakaryocyte |
|
|
Contact with |
|
collagen |
Activation |
ADP |
Thrombin |
|
|
Thromboxane A2 |
|
Serotonin |
Glyco- |
|
protein |
|
IIb/IIIa |
|
Platelet |
|
|
Platelet |
Fibrinogen |
Glycoprotein |
|
IIb/IIIa |
|
Fibrinogen- |
|
binding: |
|
impossible |
Aggregation |
possible |

154 Antithrombotics
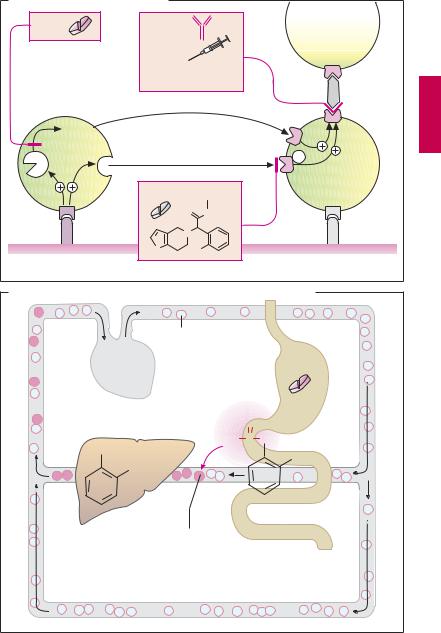
Inhibitors of Platelet Aggregation (A)
Collagen, thrombin, ADP, and thromboxane A2 are the most important mediators that induce maximal activation and aggregation of platelets. The first essential step in platelet activation is mediated by direct contact with collagen, which can bind to different proteins in the platelet membrane. The most important “collagen receptor” in the platelet membrane is glycoprotein VI (GP VI). Activation induces a change in platelet shape and triggers secretion of substances stored in intracellular platelet granula (e.g., ADP, serotonin). In addition, GP VI stimulates cyclooxygenase (COX-1), causing thromboxane A2 to be produced and released from arachidonic acid (p.196).
The propensity of platelets to aggregate can be inhibited by various pharmacological interventions.
Acetylsalicylic acid (ASA) prevents COX- 1-mediated synthesis of thromboxane. Low daily doses (75–100 mg) may be suf cient. Indications include prophylaxis of re-infarc- tion after myocardial infarction and of stroke. Despite the low dosage, adverse effects such as gastric mucosal damage or provocation of asthma attacks cannot be ruled out.
Available alternatives to ASA are the ADP receptor antagonists ticlopidine and clopidrogel, which can also be given orally. Similarly to ASA, ticlopidine and clopidrogel cause an irreversible inhibition of platelet function. Both substances are inactive precursors that are converted by hepatic cytochrome P450 to an active metabolite that binds covalently to a subtype (P2Y12) of ADP receptors on platelets. Consequently, ADP-mediated platelet aggregation is inhibited for the duration of the platelet life cycle (~ 7–10 days). Ticlopidine may cause serious adverse effects, including neutropenia and thrombopenia. The successor substance, clopidrogel, is better tolerated.
Antagonists at the integrin glycoprotein IIb/IIIa. Available agents are suitable only for parenteral administration and, in clinical settings, are used in percutaneous coronary balloon distension or in unstable angina pectoris. They block the fibrinogen cross-linking protein and thus decrease fibrinogen-medi- ated meshing of platelets independently of the precipitating cause. Abciximab is a chimeric Fab-antibody fragment directed against GP IIb/IIIa protein. Tirofiban and eptifibatide act as competitive antagonists at the fibrinogen binding site. Because abciximab adheres to GPIIb/IIIa for a long time, 24–48 hours are required after injection of the drug before platelet aggregation again becomes possible. The effects of eptifibatide and tirofiban dissipate within a few hours. Because GP IIb/IIIa antagonists inhibit the common final pathway in platelet activation, they pose a risk of bleeding during treatment.
Presystemic Effect of ASA
The inhibition of platelet aggregation by ASA results from acetylation and blockade of platelet COX-1 (B). The specificity of this reaction is achieved in the following manner: irreversible acetylation of the enzyme already occurs in the blood of the splanchnic region, that is, before the liver is reached. Since ASAissubjecttoextensive presystemic deacetylation,cyclooxygenases located posthepatically (e.g., in endothelial cells) are hardly affected. Confinement of COX-1 inhibition to platelets is further accentuated because enzyme can be re-synthesized in normal cells having a nucleus but not in the anuclear platelets.
Inhibitors of Platelet Aggregation |
155 |
A. Inhibitors of platelet aggregation |
|
|
||
ASA |
|
Abciximab |
|
|
|
|
|
|
|
Acetylsalicylic acid |
Eptifibatide, |
|
||
|
|
a peptide |
|
|
|
|
Tirofiban, |
|
|
|
|
nonpeptide |
|
Fibrinogen |
|
|
|
|
|
|
|
GPIIb/IIIa antagonists |
||
|
|
|
|
GPIIb/IIIa |
|
Throm- |
|
|
TP |
|
boxane A2 |
|
|
|
Cox1 |
Secretion |
ADP |
Gi |
|
|
|
|
|
P2Y12 |
|
|
Clopidogrel |
|
CH3 |
|
|
|
|
|
GPVI |
|
O |
|
O |
|
|
|
|
|
|
|
N |
|
|
|
|
S |
Cl |
|
Collagen |
|
ADP-receptor antagonists |
||
|
|
|||
B. Presystemic inhibition of platelet aggregation by acetylsalicylic acid |
||
Platelets |
|
|
|
Low dose |
|
O |
Acetylsalicylic |
|
H3C C O |
acid |
|
|
||
OH |
COOH |
|
COOH |
||
|
||
Acetylation of |
|
|
COX in platelets |
|
|
