
- •Preface to the 3rd edition
- •General Pharmacology
- •Systems Pharmacology
- •Therapy of Selected Diseases
- •Subject Index
- •Abbreviations
- •General Pharmacology
- •History of Pharmacology
- •Drug and Active Principle
- •The Aims of Isolating Active Principles
- •European Plants as Sources of Effective Medicines
- •Drug Development
- •Congeneric Drugs and Name Diversity
- •Oral Dosage Forms
- •Drug Administration by Inhalation
- •Dermatological Agents
- •From Application to Distribution in the Body
- •Potential Targets of Drug Action
- •External Barriers of the Body
- •Blood–Tissue Barriers
- •Membrane Permeation
- •Binding to Plasma Proteins
- •The Liver as an Excretory Organ
- •Biotransformation of Drugs
- •Drug Metabolism by Cytochrome P450
- •The Kidney as an Excretory Organ
- •Presystemic Elimination
- •Drug Concentration in the Body as a Function of Time—First Order (Exponential) Rate Processes
- •Time Course of Drug Concentration in Plasma
- •Time Course of Drug Plasma Levels during Repeated Dosing (A)
- •Time Course of Drug Plasma Levels during Irregular Intake (B)
- •Accumulation: Dose, Dose Interval, and Plasma Level Fluctuation (A)
- •Dose–Response Relationship
- •Concentration–Effect Curves (B)
- •Concentration–Binding Curves
- •Types of Binding Forces
- •Agonists—Antagonists
- •Other Forms of Antagonism
- •Enantioselectivity of Drug Action
- •Receptor Types
- •Undesirable Drug Effects, Side Effects
- •Drug Allergy
- •Cutaneous Reactions
- •Drug Toxicity in Pregnancy and Lactation
- •Pharmacogenetics
- •Placebo (A)
- •Systems Pharmacology
- •Sympathetic Nervous System
- •Structure of the Sympathetic Nervous System
- •Adrenergic Synapse
- •Adrenoceptor Subtypes and Catecholamine Actions
- •Smooth Muscle Effects
- •Cardiostimulation
- •Metabolic Effects
- •Structure–Activity Relationships of Sympathomimetics
- •Indirect Sympathomimetics
- •Types of
- •Antiadrenergics
- •Parasympathetic Nervous System
- •Cholinergic Synapse
- •Parasympathomimetics
- •Parasympatholytics
- •Actions of Nicotine
- •Localization of Nicotinic ACh Receptors
- •Effects of Nicotine on Body Function
- •Aids for Smoking Cessation
- •Consequences of Tobacco Smoking
- •Dopamine
- •Histamine Effects and Their Pharmacological Properties
- •Serotonin
- •Vasodilators—Overview
- •Organic Nitrates
- •Calcium Antagonists
- •ACE Inhibitors
- •Drugs Used to Influence Smooth Muscle Organs
- •Cardiac Drugs
- •Cardiac Glycosides
- •Antiarrhythmic Drugs
- •Drugs for the Treatment of Anemias
- •Iron Compounds
- •Prophylaxis and Therapy of Thromboses
- •Possibilities for Interference (B)
- •Heparin (A)
- •Hirudin and Derivatives (B)
- •Fibrinolytics
- •Intra-arterial Thrombus Formation (A)
- •Formation, Activation, and Aggregation of Platelets (B)
- •Inhibitors of Platelet Aggregation (A)
- •Presystemic Effect of ASA
- •Plasma Volume Expanders
- •Lipid-lowering Agents
- •Diuretics—An Overview
- •NaCl Reabsorption in the Kidney (A)
- •Aquaporins (AQP)
- •Osmotic Diuretics (B)
- •Diuretics of the Sulfonamide Type
- •Potassium-sparing Diuretics (A)
- •Vasopressin and Derivatives (B)
- •Drugs for Gastric and Duodenal Ulcers
- •Laxatives
- •Antidiarrheal Agents
- •Drugs Affecting Motor Function
- •Muscle Relaxants
- •Nondepolarizing Muscle Relaxants
- •Depolarizing Muscle Relaxants
- •Antiparkinsonian Drugs
- •Antiepileptics
- •Pain Mechanisms and Pathways
- •Eicosanoids
- •Antipyretic Analgesics
- •Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- •Cyclooxygenase (COX) Inhibitors
- •Local Anesthetics
- •Opioid Analgesics—Morphine Type
- •General Anesthesia and General Anesthetic Drugs
- •Inhalational Anesthetics
- •Injectable Anesthetics
- •Sedatives, Hypnotics
- •Benzodiazepines
- •Pharmacokinetics of Benzodiazepines
- •Therapy of Depressive Illness
- •Mania
- •Therapy of Schizophrenia
- •Psychotomimetics (Psychedelics, Hallucinogens)
- •Hypothalamic and Hypophyseal Hormones
- •Thyroid Hormone Therapy
- •Glucocorticoid Therapy
- •Follicular Growth and Ovulation, Estrogen and Progestin Production
- •Oral Contraceptives
- •Antiestrogen and Antiprogestin Active Principles
- •Aromatase Inhibitors
- •Insulin Formulations
- •Treatment of Insulin-dependent Diabetes Mellitus
- •Treatment of Maturity-Onset (Type II) Diabetes Mellitus
- •Oral Antidiabetics
- •Drugs for Maintaining Calcium Homeostasis
- •Drugs for Treating Bacterial Infections
- •Inhibitors of Cell Wall Synthesis
- •Inhibitors of Tetrahydrofolate Synthesis
- •Inhibitors of DNA Function
- •Inhibitors of Protein Synthesis
- •Drugs for Treating Mycobacterial Infections
- •Drugs Used in the Treatment of Fungal Infections
- •Chemotherapy of Viral Infections
- •Drugs for the Treatment of AIDS
- •Drugs for Treating Endoparasitic and Ectoparasitic Infestations
- •Antimalarials
- •Other Tropical Diseases
- •Chemotherapy of Malignant Tumors
- •Targeting of Antineoplastic Drug Action (A)
- •Mechanisms of Resistance to Cytostatics (B)
- •Inhibition of Immune Responses
- •Antidotes and Treatment of Poisonings
- •Therapy of Selected Diseases
- •Hypertension
- •Angina Pectoris
- •Antianginal Drugs
- •Acute Coronary Syndrome— Myocardial Infarction
- •Congestive Heart Failure
- •Hypotension
- •Gout
- •Obesity—Sequelae and Therapeutic Approaches
- •Osteoporosis
- •Rheumatoid Arthritis
- •Migraine
- •Common Cold
- •Atopy and Antiallergic Therapy
- •Bronchial Asthma
- •Emesis
- •Alcohol Abuse
- •Local Treatment of Glaucoma
- •Further Reading
- •Further Reading
- •Picture Credits
- •Drug Indexes

136 Cardiac Drugs
Antiarrhythmic Drugs
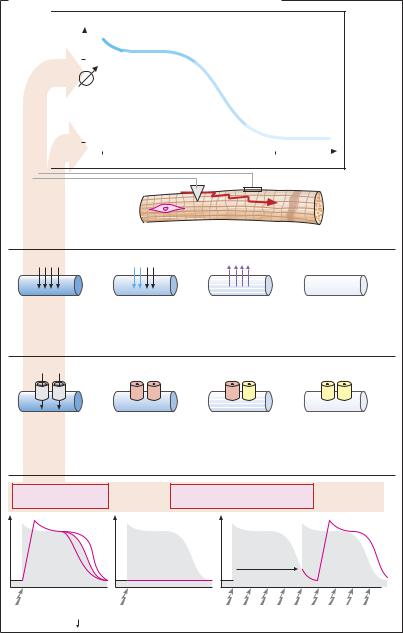
The electrical impulse for contraction (propagated action potential; p.138) originates in pacemaker cells of the sinoatrial node and spreads through the atria, atrioventricular (AV) node, and adjoining parts of the His–Purkinje fiber system to the ventricles (A). Irregularities of heart rhythm can interfere dangerously with cardiac pumping function.
I. Drugs for Selective Control of Sinoatrial and AV Nodes
In some forms of arrhythmia, certain drugs can be used that are capable of selectively facilitating and inhibiting (green and red arrows, respectively) the pacemaker function of sinoatrial or atrioventricular cells.
Sinus bradycardia. An abnormally low sinoatrial impulse rate (< 60/min) can be raised by parasympatholytics. The quaternary ipratropium is preferable to atropine, because it lacks CNS penetrability (p.108). Sympathomimetics also exert a positive chronotropic action; they have the disadvantage of increasing myocardial excitability (and automaticity) and, thus, promoting ectopic impulse generation (tendency to extrasystolic beats). In cardiac arrest, epinephrine, given by intrabronchial instillation or intracardiac injection, can be used to reinitiate heart beat.
Sinus tachycardia (resting rate > 100 beats/ min). β-Blockers eliminate sympatho-excita- tion and lower cardiac rate. Sotalol is noteworthy because of its good antiarrhythmic action (caution: QT-prolongation)
Atrial flutter or fibrillation. An excessive ventricular rate can be decreased by verapamil (p.126) or cardiac glycosides (p.134). These drugs inhibit impulse propagation through the AV node, so that fewer impulses reach the ventricles.
II. Nonspecific Drug Actions on Impulse Generation and Propagation
In some types of rhythm disorders, antiarrhythmics of the local anesthetic, Na+- channel blocking type are used for both prophylaxis and therapy. These substances block the Na+ channel responsible for the fast depolarization of nerve and muscle tissues. Therefore, the elicitation of action potentials is impeded and impulse conduction is delayed. This effect may exert a favorable influence in some forms of arrhythmia, but can itself act arrhythmogenically. Unfortunately, antiarrhythmics of the local anesthetic, Na+-channel blocking type lack suf - cient specificity in two respects: (1) other ion channels of cardiomyocytes, such as K+ and Ca+ channels, are also affected (abnormal QT prolongation); and (2) their action is not restricted to cardiac muscle tissue but also impacts on neural tissues and brain cells. Adverse effects on the heart include production of arrhythmias and lowering of heart rate, AV conduction, and systolic force. CNS side effects are manifested by vertigo, giddiness, disorientation, confusion, motor disturbances, etc.
Some antiarrhythmics are rapidly degraded in the body by cleavage (see arrows in B); these substances are not suitable for oral administration but must be given intravenously (e.g., lidocaine).
Irrespective of the cause underlying atrial fibrillation, formation of a thrombus may occur in the atria, because blood stagnates in the auricles. From such a thrombus an embolus may be dislodged and carried into the arterial supply of the brain, precipitating a stroke. Itistherefore imperative toinstitute anticoagulant therapy in atrial fibrillation. For immediate effect, heparin preparations are indicated; subsequently, changeover to vitamin K antagonists (e.g., phenprocoumon) may be made. As long as episodes of arrhythmia occur, therapy must be continued.

|
Antiarrhythmic Drugs |
137 |
A. Cardiac impulse generation and conduction |
|
|
Sinus node |
|
|
|
Para- |
|
Atrium |
sympatholytics |
|
β -Sympatho- |
|
|
|
|
|
|
mimetics |
|
AV-node |
|
|
Bundle of His |
|
|
Tawara (AV node) |
β -Blocker |
|
Verapamil |
|
|
bundle branches |
|
|
Purkinje |
Cardiac |
|
glycoside |
|
|
fibers |
|
|
Ventricle |
Vagal |
|
|
stimulation |
|
B. Antiarrhythmics of the Na+-channel blocking type
Main effect
Antiarrhythmic effect
Adverse effects
CNS disturbances
Arrhythmia
Cardiodepression
Antiarrhythmics of the local anesthetic (Na+-channel blocking) type:
Inhibition of impulse generation and conduction
Esterases |
|
|
|
|
|
|
|
|
|
Procaine |
|
|
O |
|
|
|
|
|
|
C2H5 |
|||
|
|
|
|
|
|
+ |
|||||
H2N |
C |
|
|
O |
|
CH2 |
|
CH2 |
|
NH |
|
|
|
|
|
|
|
|
|
|
|
|
C2H5 |
|
|
|
|
|
|
Procainamide |
|||
|
O |
|
|
|
|
|
C2H5 |
||
|
|
|
|
+ |
|||||
H2N |
C |
|
N |
|
CH2 |
|
CH2 |
|
NH |
|
|
|
H |
|
|
|
|
|
C2H5 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
CH3 |
|
O |
Lidocaine |
|
|
C2H5 |
|
|
|
|
+ |
N C |
CH2 NH |
||
H |
|
|
|
C2H5
CH3
CH3 |
H |
Mexiletine |
|
|
|
O CH2 |
+ |
|
CH NH |
|
|
|
H |
|
CH3 |
CH3 |
|
|
|

138 Cardiac Drugs
Electrophysiological Actions of Antiarrhythmics of the Na+-Channel Blocking Type
Action potential and ionic currents. The transmembrane electrical potential of cardiomyocytes can be recorded through an intracellular microelectrode. Upon electrical excitation, the resting potential shows a characteristic change—the action potential (AP). Its underlying cause is a sequence of transient ionic currents. During rapid depolarization (phase 0), there is a short-lived influx of Na+ through the membrane. A subsequent transient influx of Ca2+ (as well as of Na+) maintains the depolarization (phase 2, plateau of AP). A delayed ef ux of K+ returns the membrane potential (phase 3, repolarization) to its resting value (phase 4). The velocity of depolarization determines the speed at which the AP propagates through the myocardial syncytium.
The transmembrane ionic currents involve proteinaceous membrane pores: Na+, Ca2+, and K+ channels. In (A), the phasic change in the functional state of Na+ channels during an action potential is illustrated.
Na+-channel blocking antiarrhythmics reduce the probability of Na+ channels to open upon membrane depolarization (“membrane stabilization”). The potential consequences are (A, bottom): (1) A reduction in the velocity of depolarization and a decrease in the speed of impulse propagation; aberrant impulse propagation is impeded. (2)
Depolarization is entirely absent; pathological impulse generation, e.g., in the marginal zone of an infarction, is suppressed. (3) The time required until a new depolarization can be elicited, i.e., the refractory period, is increased; prolongation of the AP (see below) contributes to the increase in refractory period. Consequently, premature excitation with risk of fibrillation is prevented.
Mechanism of action. Na+-channel blocking antiarrhythmics resemble most local anesthetics in being cationic amphiphilic molecules (p.206; exception: phenytoin, p.191). Possible molecular mechanisms of their inhibitory effects are outlined on p.202 in more detail. Their low structural specificity is reflected by a low selectivity toward different cation channels. Besides the Na+ channel, Ca2+and K+ channels are also likely to be blocked. Accordingly, cationic amphiphilic antiarrhythmics affect both the depolarization and repolarization phases. Depending on the substance, AP duration can be increased (Class IA), decreased (Class IB), or remain the same (Class IC). Antiarrhythmics representative of these categories include: Class IA—quinidine, procainamide, ajmaline, disopyramide; Class IB—lidocaine, mexiletine, tocainide; Class IC—flecainide, propafenone.
K2+–channel blocking antiarrhythmics. The drug amiodarone and the β-blocker sotalol have been assigned to Class III, comprising agents that cause marked prolongation of AP with less effect on the velocity of depolarization. Note that Class II is represented by β-blockers and Class IV by the Ca2+-chan- nel blockers verapamil and diltiazem (see p.126).
Therapeutic uses. Because of their narrow therapeutic margin, antiarrhythmics are only employed when rhythm disturbances are of such severity as to impair the pumping action of the heart, or when there is a threat of other complications. Combinations of different antiarrhythmics are not recommended (e.g., quinidine plus verapamil). Some agents, such as amiodarone, are reserved for special cases. This iodine-containing substance has unusual properties: its elimination half-life is 50–70 days; depending on its electrical charge, it is bound to apolar and polar lipids, stored in tissues (corneal opacification, pulmonary fibrosis); and it interferes with thyroid function.
Antiarrhythmics of Na+-Channel Blocking Type |
139 |
A. Effects of antiarrhythmics of the Na+-channel blocking type
|
|
[mV] |
|
|
|
potentialMembrane |
0 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
-80 |
|
|
|
|
|
|
|
|
|
|
|
|
Na+
|
|
|
Action potential |
|
|
|
|
|
|
|
|
1 |
2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
0 |
|
|
Rate of |
|
3 |
|
|
|
|
|
|
depolarization |
|
4 |
|
|
|||
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
Refractory period |
|
|
|
|
|
|
|
|
|
|
|
250 Time [ms] |
|
|||
|
0 |
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Heart muscle cell
Ca2+(+Na+)
|
|
K+ |
|
Phase 0 |
Phases 1,2 |
Phase 3 |
Phase 4 |
Fast |
Slow Ca2+-entry |
|
|
Na+-entry |
|
|
|
Ionic currents during action potential |
|
|
|
Na+ |
Na+-channels |
|
|
Open (active) |
Closed |
|
Closed |
Opening impossible |
|
Opening possible |
|
|
|
||
|
(inactivated) |
|
(resting, can be |
States of Na+-channels during an action potential |
|
activated) |
|
|
|
||
Inhibition of |
Antiarrhythmics of the |
|
|
Na+-channel opening |
Na+-channel blocking type |
|
|
|
|
Inexcitability |
|
Stimulus |
|
|
|
Rate of |
Suppression |
Prolongation of refractory period = |
|
depolarization |
of AP generation |
duration of inexcitability |
|
