
- •Preface to the 3rd edition
- •General Pharmacology
- •Systems Pharmacology
- •Therapy of Selected Diseases
- •Subject Index
- •Abbreviations
- •General Pharmacology
- •History of Pharmacology
- •Drug and Active Principle
- •The Aims of Isolating Active Principles
- •European Plants as Sources of Effective Medicines
- •Drug Development
- •Congeneric Drugs and Name Diversity
- •Oral Dosage Forms
- •Drug Administration by Inhalation
- •Dermatological Agents
- •From Application to Distribution in the Body
- •Potential Targets of Drug Action
- •External Barriers of the Body
- •Blood–Tissue Barriers
- •Membrane Permeation
- •Binding to Plasma Proteins
- •The Liver as an Excretory Organ
- •Biotransformation of Drugs
- •Drug Metabolism by Cytochrome P450
- •The Kidney as an Excretory Organ
- •Presystemic Elimination
- •Drug Concentration in the Body as a Function of Time—First Order (Exponential) Rate Processes
- •Time Course of Drug Concentration in Plasma
- •Time Course of Drug Plasma Levels during Repeated Dosing (A)
- •Time Course of Drug Plasma Levels during Irregular Intake (B)
- •Accumulation: Dose, Dose Interval, and Plasma Level Fluctuation (A)
- •Dose–Response Relationship
- •Concentration–Effect Curves (B)
- •Concentration–Binding Curves
- •Types of Binding Forces
- •Agonists—Antagonists
- •Other Forms of Antagonism
- •Enantioselectivity of Drug Action
- •Receptor Types
- •Undesirable Drug Effects, Side Effects
- •Drug Allergy
- •Cutaneous Reactions
- •Drug Toxicity in Pregnancy and Lactation
- •Pharmacogenetics
- •Placebo (A)
- •Systems Pharmacology
- •Sympathetic Nervous System
- •Structure of the Sympathetic Nervous System
- •Adrenergic Synapse
- •Adrenoceptor Subtypes and Catecholamine Actions
- •Smooth Muscle Effects
- •Cardiostimulation
- •Metabolic Effects
- •Structure–Activity Relationships of Sympathomimetics
- •Indirect Sympathomimetics
- •Types of
- •Antiadrenergics
- •Parasympathetic Nervous System
- •Cholinergic Synapse
- •Parasympathomimetics
- •Parasympatholytics
- •Actions of Nicotine
- •Localization of Nicotinic ACh Receptors
- •Effects of Nicotine on Body Function
- •Aids for Smoking Cessation
- •Consequences of Tobacco Smoking
- •Dopamine
- •Histamine Effects and Their Pharmacological Properties
- •Serotonin
- •Vasodilators—Overview
- •Organic Nitrates
- •Calcium Antagonists
- •ACE Inhibitors
- •Drugs Used to Influence Smooth Muscle Organs
- •Cardiac Drugs
- •Cardiac Glycosides
- •Antiarrhythmic Drugs
- •Drugs for the Treatment of Anemias
- •Iron Compounds
- •Prophylaxis and Therapy of Thromboses
- •Possibilities for Interference (B)
- •Heparin (A)
- •Hirudin and Derivatives (B)
- •Fibrinolytics
- •Intra-arterial Thrombus Formation (A)
- •Formation, Activation, and Aggregation of Platelets (B)
- •Inhibitors of Platelet Aggregation (A)
- •Presystemic Effect of ASA
- •Plasma Volume Expanders
- •Lipid-lowering Agents
- •Diuretics—An Overview
- •NaCl Reabsorption in the Kidney (A)
- •Aquaporins (AQP)
- •Osmotic Diuretics (B)
- •Diuretics of the Sulfonamide Type
- •Potassium-sparing Diuretics (A)
- •Vasopressin and Derivatives (B)
- •Drugs for Gastric and Duodenal Ulcers
- •Laxatives
- •Antidiarrheal Agents
- •Drugs Affecting Motor Function
- •Muscle Relaxants
- •Nondepolarizing Muscle Relaxants
- •Depolarizing Muscle Relaxants
- •Antiparkinsonian Drugs
- •Antiepileptics
- •Pain Mechanisms and Pathways
- •Eicosanoids
- •Antipyretic Analgesics
- •Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- •Cyclooxygenase (COX) Inhibitors
- •Local Anesthetics
- •Opioid Analgesics—Morphine Type
- •General Anesthesia and General Anesthetic Drugs
- •Inhalational Anesthetics
- •Injectable Anesthetics
- •Sedatives, Hypnotics
- •Benzodiazepines
- •Pharmacokinetics of Benzodiazepines
- •Therapy of Depressive Illness
- •Mania
- •Therapy of Schizophrenia
- •Psychotomimetics (Psychedelics, Hallucinogens)
- •Hypothalamic and Hypophyseal Hormones
- •Thyroid Hormone Therapy
- •Glucocorticoid Therapy
- •Follicular Growth and Ovulation, Estrogen and Progestin Production
- •Oral Contraceptives
- •Antiestrogen and Antiprogestin Active Principles
- •Aromatase Inhibitors
- •Insulin Formulations
- •Treatment of Insulin-dependent Diabetes Mellitus
- •Treatment of Maturity-Onset (Type II) Diabetes Mellitus
- •Oral Antidiabetics
- •Drugs for Maintaining Calcium Homeostasis
- •Drugs for Treating Bacterial Infections
- •Inhibitors of Cell Wall Synthesis
- •Inhibitors of Tetrahydrofolate Synthesis
- •Inhibitors of DNA Function
- •Inhibitors of Protein Synthesis
- •Drugs for Treating Mycobacterial Infections
- •Drugs Used in the Treatment of Fungal Infections
- •Chemotherapy of Viral Infections
- •Drugs for the Treatment of AIDS
- •Drugs for Treating Endoparasitic and Ectoparasitic Infestations
- •Antimalarials
- •Other Tropical Diseases
- •Chemotherapy of Malignant Tumors
- •Targeting of Antineoplastic Drug Action (A)
- •Mechanisms of Resistance to Cytostatics (B)
- •Inhibition of Immune Responses
- •Antidotes and Treatment of Poisonings
- •Therapy of Selected Diseases
- •Hypertension
- •Angina Pectoris
- •Antianginal Drugs
- •Acute Coronary Syndrome— Myocardial Infarction
- •Congestive Heart Failure
- •Hypotension
- •Gout
- •Obesity—Sequelae and Therapeutic Approaches
- •Osteoporosis
- •Rheumatoid Arthritis
- •Migraine
- •Common Cold
- •Atopy and Antiallergic Therapy
- •Bronchial Asthma
- •Emesis
- •Alcohol Abuse
- •Local Treatment of Glaucoma
- •Further Reading
- •Further Reading
- •Picture Credits
- •Drug Indexes

218 General Anesthetics
Injectable Anesthetics
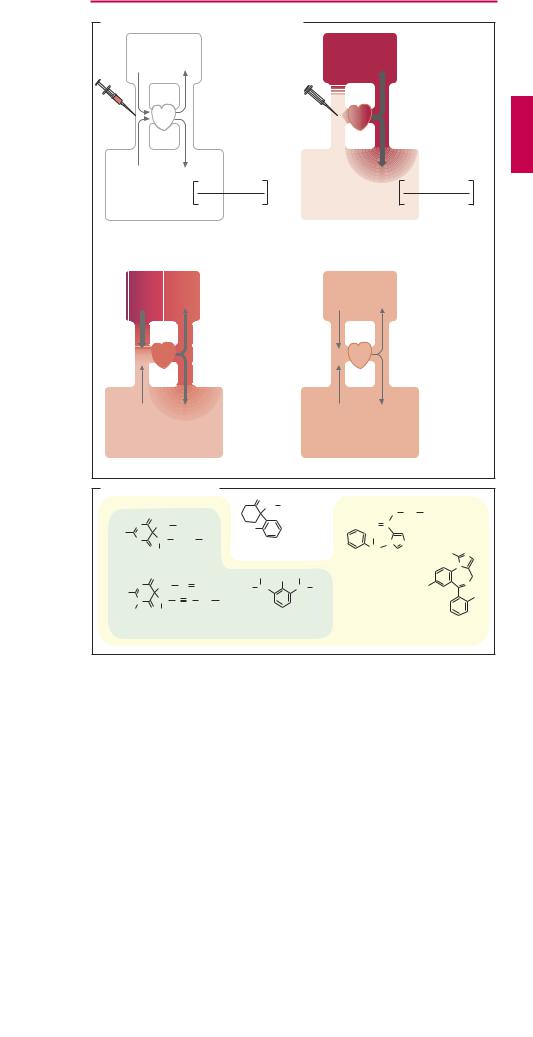
Substances from different chemical classes suspend consciousness when given intravenously and can be used as injectable anesthetics (A). Like inhalational agents, most of these drugs affectconsciousness onlyandare devoid of analgesic activity (exception: ketamine). The effect appears to arise from an interaction with ligand-gated ion channels. Channels mediating neuronal excitation (NMDA receptor, see below) are blocked, while the function of channels dampening excitation (GABAA receptor, p.222; and, for three drugs, additionally also the glycine receptor) is enhanced allosterically.
Most injectable anesthetics are characterized by a short duration of action. The rapid cessation of action is largely due to redistribution: after intravenous injection, brain concentration climbs rapidly to effective anesthetic levels because of the high cerebral blood flow; the drug then distributes evenly in the body, i.e., concentration rises in the periphery, but falls in the brain—redis- tribution and cessation of anesthesia (A). Thus, the effect subsides before the drug has left the body. A second injection of the same drug would encounter “presaturated” body compartments and thus be dif cult to predict in terms of effect intensity. Only etomidate and propofol may be given by infusion over a longer period to maintain unconsciousness. If no additional inhalational agent is employed, the procedure is referred to as total intravenous anesthesia (TIVA).
Thiopental and methohexital belong to the barbiturates,which, depending on dose,produce sedation, sleepiness, or anesthesia. Barbiturates lower pain threshold and thereby facilitate defensive reflex movements; they also depress central inspiratory drive. Barbiturates are frequently used for induction of anesthesia.
Ketamine has analgesic activity that persistsup to1hour after injection, wellbeyond the initial period of unconsciousness (~ 15 minutes only). On regaining consciousness, the patient may experience a disconnection
between outside reality and inner mental state (dissociative anesthesia). Frequently there is memory loss for the duration of the recovery period; however, adults in particular complain about distressing dreamlike experiences. These can be counteracted by administration of a benzodiazepine (e.g., midazolam). TheCNSeffectsofketamine arise,in part, from an interference with excitatory glutamatergic transmission via ligand-gated cation channels of the NMDA subtype, at which ketamine acts as a channel blocker. The nonnatural excitatory amino acid N- methyl D-aspartate (NMDA) is a selective agonist at this receptor. Ketamine can induce release of catecholamines with a resultant increase in heart rate and blood pressure.
Propofol has a remarkably simple structure resembling that of phenol disinfectants. Because the substance is water-insoluble, an injectable emulsion is prepared by means of soy oil, phosphatide, and glycerol. The effect has a rapid onset and decays quickly, being experienced by the patient as fairly pleasant. The intensity of the effect can be well controlled during prolonged administration. Possible adverse reactions include hypotension and respiratory depression, and a potentially fatal syndrome of bronchospasm, hypotension, and erythema.
The anesthetic effect of (+)-etomidate subsides within a few minutes owing to redistribution of the drug. Etomidate can provoke myoclonic movements that can be prevented by premedicationwith a benzodiazepine or an opioid. Because it has little effect on the autonomic nervous system, it is suitable for induction in combination anesthesia. Etomidate inhibits cortisol synthesis in subanesthetic doses and can therefore be used in the long-term treatment of adrenocortical overactivity (Cushing disease).
Midazolam is a rapidly metabolized benzodiazepine (p.224) that is used for induction of anesthesia. The longer-acting lorazepam is preferred as an adjunctive anesthetic in prolonged cardiacsurgery with cardiopulmonary bypass; its amnesiogenic effect is pronounced.
|
|
|
|
|
|
|
|
|
Injectable Anesthetics |
219 |
||
A. Termination of drug effect by redistribution |
|
|
|
|
||||||||
|
|
|
|
CNS: |
|
|
|
|
High concentration |
|||
|
|
|
|
|
|
|
|
in tissue |
|
|||
|
|
|
|
relatively |
|
|
|
|
|
|
|
|
|
|
|
|
high |
|
|
|
|
Relatively large |
|
||
|
|
|
|
blood flow |
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
amount of drug |
||||
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
i.v. injection |
|
|
|
|
|
|
|
|
|
Periphery: |
|
|
|
|
|
|
|
|
|
|
|
|
relatively |
|
|
|
|
|
|
|
|
|
|
|
|
low blood flow |
|
|
|
Relatively small |
|
|||
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
amount of drug |
||
|
|
|
|
ml blood |
|
|
|
|
mg drug |
|
||
|
|
|
|
min x g tissue |
|
|
|
|
min x g tissue |
|
||
1. Initial situation |
|
|
|
|
|
|
2. Preferential accumulation |
|
|
|||
|
|
|
|
|
|
|
|
of drug in brain |
|
|
|
|
|
|
|
|
Decrease |
|
|
|
|
Low concentration |
|||
|
|
|
|
in tissue |
|
|
|
|
in periphery |
|
||
|
|
|
|
concentration |
|
|
|
|
|
|
||
|
|
|
|
Further |
|
|
|
|
|
|
|
|
|
|
|
|
increase |
|
|
|
|
|
|
|
|
|
|
|
|
in tissue |
|
|
|
|
|
|
|
|
|
|
|
|
concentration |
|
|
|
|
|
|
||
3. Redistribution |
|
|
|
|
|
|
4. Steady state of distribution |
|
|
|||
B. Intravenous anesthetics |
|
O |
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
NH |
CH3 |
|
O |
CH2 |
CH3 |
|
|
O |
|
|
|
|
|
Ketamine |
|
||||
|
|
|
|
|
|
|
|
|
|
|||
N |
CH2 |
CH3 |
|
Cl |
|
O C |
|
|
|
|||
|
|
|
|
Etomidate |
|
|||||||
NaS |
CH |
(CH2 )2 |
CH3 |
|
|
|
CH3 |
|
||||
N |
|
|
|
|
|
|
|
|||||
NMDA receptor |
|
N |
N |
|
|
|||||||
H |
|
|
|
|
|
|
|
|||||
|
O CH3 |
|
|
|
blockade |
|
|
CH |
|
H3C |
N |
|
Sodium thiopental |
|
|
|
|
|
|
|
|
N |
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
O |
|
|
|
|
CH3 |
OH |
CH3 |
|
|
|
|
N |
CH2 |
CH |
|
CH2 |
|
|
|
|
|
Cl |
N |
|
|
H3C |
CH |
|
CH CH3 |
|
|
||||||
NaO |
|
|
|
|
|
|
|
|
F |
|||
CH |
C |
C |
CH2 |
CH3 |
|
|
|
|
|
|
||
N |
|
|
Propofol |
|
|
|
||||||
|
|
|
|
|
|
|||||||
H3C |
O CH3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Activation of |
|
|
Activation of |
|
|
||||
Sodium methohexital |
|
|
|
Midazolam |
||||||||
|
glycine receptors |
|
GABAA receptors |
|||||||||
|
|
|
|
|
|
|
|
|||||

220 Psychopharmacologicals
Sedatives, Hypnotics
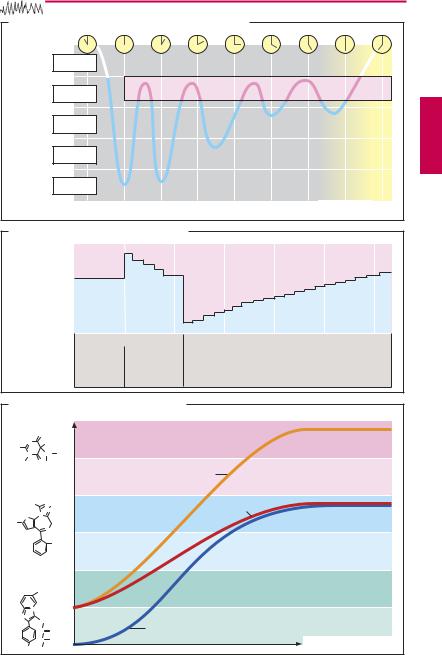
During sleep, the brain generates a patterned rhythmic activity that can be monitored by means of the electroencephalogram (EEG). Internal sleep cycles recur 4–5 times per night, each cycle being interrupted by a rapid eye movement (REM) sleep phase (A). The REM stage is characterized by EEG activity similar to that seen in the waking state, rapid eye movements, vivid dreams, and occasional twitches of individual muscle groups against a background of generalized atonia of skeletal musculature. Normally, the REM stage is entered only after a preceding non-REM cycle. Frequent interruption of sleep will, therefore, decrease the REM portion. Shortening of REM sleep (normally ~ 25% of total sleep duration) results in increased irritability and restlessness during the daytime. With undisturbed night rest, REM deficits are compensated by increased REM sleep on subsequent nights (B).
Hypnotic drugs can shorten REM sleep phases (B). With repeated ingestion of a hypnotic on several successive days, the proportion of time spent in REM vs. non-REM sleep returns to normal despite continued drug intake. Withdrawal of the hypnotic drug results in REM rebound, which tapers off only over many days (B). Since REM stages are associated with vivid dreaming, sleep with excessively long REM episodes is experienced as unrefreshing. Thus, the attempt to discontinue use of hypnotics may result in the impression that refreshing sleep calls for a hypnotic, probably promoting hypnotic drug dependence.
Benzodiazepines and benzodiazepine-like substances are the hypnotics of greatest therapeutic importance. They display a positive allosteric action at the GABAA receptor (p.222). The formerly popular barbiturates have become obsolete because of their narrow margin of safety (respiratory arrest after overdosage). Barbiturates can also activate GABAA receptors allosterically; however, this action does not occur at benzodiazepine
binding sites. At high dosage, barbiturates can apparently produce an additional direct GABA agonist effect.
Depending on their blood levels, both benzodiazepines and barbiturates produce calming and sedative effects. At higher dosage, both groups promote the onset of sleep or induce it (C). At low doses, benzodiazepines have a predominantly anxiolytic effect.
Unlike barbiturates, benzodiazepine derivatives administered orally lack a general anesthetic action; cerebral activity is not globally inhibited (the virtual impossibility of respiratory paralysis negates suicidal misuse) and autonomic functions, such as blood pressure, heart rate, or body temperature, are unimpaired. Thus, benzodiazepines possess a therapeutic margin considerably wider than that of barbiturates.
Zolpidem (an imidazopyridine), zaleplone (a pyrazolopyrimidine) and zopiclone (a cyclopyrrolone) are hypnotics that, despite their different chemical structure, can bind to the benzodiazepine site on the GABAA receptor (p.222). However, their effects do not appear to be identical to those of benzodiazepines. Thus, compared with benzodiazepines, zolpidem exerts a weaker effect on sleep phases, supposedly carries a lower risk of dependence, and appears to have less anxiolytic activity. Heterogeneity of GABAA receptors may explain these differences in activity. GABAA receptors consist of five subunits that exist in several subtypes.
Antihistaminics are popular as nonprescription (over-the-counter) sleep remedies (e.g., diphenhydramine, doxylamine, p.118), in which case their sedative side effect is used as the principal effect. The hypnotic effect is weak; adverse effects (e.g., atro- pine-like) and corresponding contraindications need to be taken into account.
|
Benzodiazepines |
221 |
A. Succession of different sleep phases during night rest |
|
|
Waking |
|
|
state |
|
|
Sleep |
|
REM |
stage I |
|
|
|
|
|
Sleep |
|
|
stage II |
|
|
Sleep |
|
|
stage III |
|
|
Sleep |
|
|
stage IV |
|
|
REM-sleep = Rapid Eye Movement sleep |
NREM = No Rapid Eye Movement sleep |
|
B. Influence of hypnotics on sleep phases
REM |
|
|
|
|
|
|
|
|
NREM |
|
|
|
|
|
|
||
|
Proportion |
|
5 |
10 |
15 |
20 |
25 |
30 |
|
|
Nights |
Nights |
Nights after |
|
|
|
|
|
|
without |
with |
withdrawal |
|
|
|
|
|
|
hypnotic |
hypnotic |
of hypnotic |
|
|
|
|
|
|
|
|
|
|
|
|
|
C. Concentration dependence of effects |
|
|
|
|
||||
Barbiturates: |
|
|
|
|
|
|||
Pentobarbital |
Effect |
|
|
|
|
|
||
|
O |
|
|
|
|
|
Paralyzing |
|
N |
C2H5 |
|
|
|
|
|
||
HO |
CH |
CH3 |
|
|
|
|
|
|
N |
|
|
|
|
|
|||
H |
O C3H7 |
|
Pentobarbital |
|
|
|
||
Benzo- |
|
|
|
|
Anesthetizing |
|
||
|
|
|
|
|
|
|
||
diazepines: |
|
|
|
|
|
|||
|
|
|
|
|
|
|||
Brotizolam |
|
|
|
|
|
|
|
|
H3C |
N |
N |
|
|
Zolpidem |
|
|
|
|
N |
|
|
|
Hypnogenic |
|
||
S |
|
|
|
|
|
|
||
|
|
|
|
|
|
|
||
Br |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
N |
|
|
|
|
|
|
|
|
|
Cl |
|
|
|
|
|
|
Imidazo- |
|
|
|
|
|
Hypnagogic |
|
|
|
|
|
|
|
|
|
||
pyridines: |
|
|
|
|
|
|
|
|
Zolpidem |
|
|
|
|
|
|
|
|
|
CH3 |
|
|
|
|
|
Sedating |
|
|
|
|
|
|
|
|
|
|
N |
|
|
|
|
|
|
|
|
N |
CH2 |
|
|
Triazolam |
|
|
Anxiolytic |
|
|
|
|
|
|
|
|||
|
C |
O |
|
|
|
|
||
|
|
|
|
|
|
|
||
|
N |
CH3 |
|
|
|
Concentration in blood |
||
CH3 |
CH3 |
|
|
|
|
|
|
|
