
- •Preface to the 3rd edition
- •General Pharmacology
- •Systems Pharmacology
- •Therapy of Selected Diseases
- •Subject Index
- •Abbreviations
- •General Pharmacology
- •History of Pharmacology
- •Drug and Active Principle
- •The Aims of Isolating Active Principles
- •European Plants as Sources of Effective Medicines
- •Drug Development
- •Congeneric Drugs and Name Diversity
- •Oral Dosage Forms
- •Drug Administration by Inhalation
- •Dermatological Agents
- •From Application to Distribution in the Body
- •Potential Targets of Drug Action
- •External Barriers of the Body
- •Blood–Tissue Barriers
- •Membrane Permeation
- •Binding to Plasma Proteins
- •The Liver as an Excretory Organ
- •Biotransformation of Drugs
- •Drug Metabolism by Cytochrome P450
- •The Kidney as an Excretory Organ
- •Presystemic Elimination
- •Drug Concentration in the Body as a Function of Time—First Order (Exponential) Rate Processes
- •Time Course of Drug Concentration in Plasma
- •Time Course of Drug Plasma Levels during Repeated Dosing (A)
- •Time Course of Drug Plasma Levels during Irregular Intake (B)
- •Accumulation: Dose, Dose Interval, and Plasma Level Fluctuation (A)
- •Dose–Response Relationship
- •Concentration–Effect Curves (B)
- •Concentration–Binding Curves
- •Types of Binding Forces
- •Agonists—Antagonists
- •Other Forms of Antagonism
- •Enantioselectivity of Drug Action
- •Receptor Types
- •Undesirable Drug Effects, Side Effects
- •Drug Allergy
- •Cutaneous Reactions
- •Drug Toxicity in Pregnancy and Lactation
- •Pharmacogenetics
- •Placebo (A)
- •Systems Pharmacology
- •Sympathetic Nervous System
- •Structure of the Sympathetic Nervous System
- •Adrenergic Synapse
- •Adrenoceptor Subtypes and Catecholamine Actions
- •Smooth Muscle Effects
- •Cardiostimulation
- •Metabolic Effects
- •Structure–Activity Relationships of Sympathomimetics
- •Indirect Sympathomimetics
- •Types of
- •Antiadrenergics
- •Parasympathetic Nervous System
- •Cholinergic Synapse
- •Parasympathomimetics
- •Parasympatholytics
- •Actions of Nicotine
- •Localization of Nicotinic ACh Receptors
- •Effects of Nicotine on Body Function
- •Aids for Smoking Cessation
- •Consequences of Tobacco Smoking
- •Dopamine
- •Histamine Effects and Their Pharmacological Properties
- •Serotonin
- •Vasodilators—Overview
- •Organic Nitrates
- •Calcium Antagonists
- •ACE Inhibitors
- •Drugs Used to Influence Smooth Muscle Organs
- •Cardiac Drugs
- •Cardiac Glycosides
- •Antiarrhythmic Drugs
- •Drugs for the Treatment of Anemias
- •Iron Compounds
- •Prophylaxis and Therapy of Thromboses
- •Possibilities for Interference (B)
- •Heparin (A)
- •Hirudin and Derivatives (B)
- •Fibrinolytics
- •Intra-arterial Thrombus Formation (A)
- •Formation, Activation, and Aggregation of Platelets (B)
- •Inhibitors of Platelet Aggregation (A)
- •Presystemic Effect of ASA
- •Plasma Volume Expanders
- •Lipid-lowering Agents
- •Diuretics—An Overview
- •NaCl Reabsorption in the Kidney (A)
- •Aquaporins (AQP)
- •Osmotic Diuretics (B)
- •Diuretics of the Sulfonamide Type
- •Potassium-sparing Diuretics (A)
- •Vasopressin and Derivatives (B)
- •Drugs for Gastric and Duodenal Ulcers
- •Laxatives
- •Antidiarrheal Agents
- •Drugs Affecting Motor Function
- •Muscle Relaxants
- •Nondepolarizing Muscle Relaxants
- •Depolarizing Muscle Relaxants
- •Antiparkinsonian Drugs
- •Antiepileptics
- •Pain Mechanisms and Pathways
- •Eicosanoids
- •Antipyretic Analgesics
- •Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- •Cyclooxygenase (COX) Inhibitors
- •Local Anesthetics
- •Opioid Analgesics—Morphine Type
- •General Anesthesia and General Anesthetic Drugs
- •Inhalational Anesthetics
- •Injectable Anesthetics
- •Sedatives, Hypnotics
- •Benzodiazepines
- •Pharmacokinetics of Benzodiazepines
- •Therapy of Depressive Illness
- •Mania
- •Therapy of Schizophrenia
- •Psychotomimetics (Psychedelics, Hallucinogens)
- •Hypothalamic and Hypophyseal Hormones
- •Thyroid Hormone Therapy
- •Glucocorticoid Therapy
- •Follicular Growth and Ovulation, Estrogen and Progestin Production
- •Oral Contraceptives
- •Antiestrogen and Antiprogestin Active Principles
- •Aromatase Inhibitors
- •Insulin Formulations
- •Treatment of Insulin-dependent Diabetes Mellitus
- •Treatment of Maturity-Onset (Type II) Diabetes Mellitus
- •Oral Antidiabetics
- •Drugs for Maintaining Calcium Homeostasis
- •Drugs for Treating Bacterial Infections
- •Inhibitors of Cell Wall Synthesis
- •Inhibitors of Tetrahydrofolate Synthesis
- •Inhibitors of DNA Function
- •Inhibitors of Protein Synthesis
- •Drugs for Treating Mycobacterial Infections
- •Drugs Used in the Treatment of Fungal Infections
- •Chemotherapy of Viral Infections
- •Drugs for the Treatment of AIDS
- •Drugs for Treating Endoparasitic and Ectoparasitic Infestations
- •Antimalarials
- •Other Tropical Diseases
- •Chemotherapy of Malignant Tumors
- •Targeting of Antineoplastic Drug Action (A)
- •Mechanisms of Resistance to Cytostatics (B)
- •Inhibition of Immune Responses
- •Antidotes and Treatment of Poisonings
- •Therapy of Selected Diseases
- •Hypertension
- •Angina Pectoris
- •Antianginal Drugs
- •Acute Coronary Syndrome— Myocardial Infarction
- •Congestive Heart Failure
- •Hypotension
- •Gout
- •Obesity—Sequelae and Therapeutic Approaches
- •Osteoporosis
- •Rheumatoid Arthritis
- •Migraine
- •Common Cold
- •Atopy and Antiallergic Therapy
- •Bronchial Asthma
- •Emesis
- •Alcohol Abuse
- •Local Treatment of Glaucoma
- •Further Reading
- •Further Reading
- •Picture Credits
- •Drug Indexes

180 Antidiarrheals
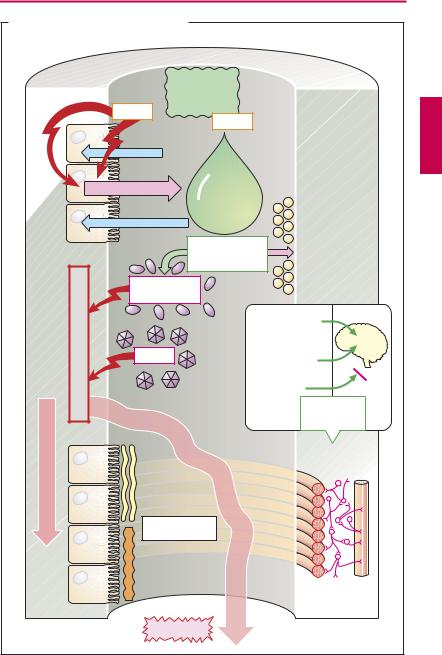
Antidiarrheal Agents
Causes of diarrhea. Many bacteria (e.g., Vibrio cholerae) secrete toxins that inhibit the ability of mucosal enterocytes to absorb NaCl and water and, at the same time, stimulate mucosal secretory activity. Bacteria or viruses that invade the gut wall cause inflammation characterized by increased fluid secretion into the lumen. The enteric musculature reacts with increased peristalsis.
The aims of antidiarrheal therapy are (1) to prevent dehydration and electrolyte depletion (exsiccosis) of the body, and (2) to prevent the distressing, though nonthreatening, frequent bowel movements. The different therapeutic approaches listed are variously suited for these purposes.
Adsorbent powders are nonabsorbable materials with a large surface area. These bind diverse substances including toxins, permitting them to be inactivated and eliminated. Medicinal charcoal has a particularly large surface because of the preserved cell structures. The recommended effective antidiarrheal dose is in the range of 4–8 g. Kaolin (hydrated aluminum silicate) is another adsorbent.
Oral rehydration solution (in g/l of boiled water: NaCl 3.5, glucose 20, NaHCO3 2.5, KCl 1.5). Oral administration of glucose-contain- ing salt solutions enables fluids to be absorbed because toxins do not impair the co-transport of Na+ and glucose (as well as of H2O) through the mucosal epithelium. In this manner, although frequent discharge of stool is not prevented, dehydration is successfully corrected (important in therapy of cholera).
Opioids. Activation of opioid receptors in the enteric nerve plexus results in inhibition of propulsive motor activity and enhancement of segmentation activity. This antidiarrheal effect was formerly induced by application of opium tincture (paregoric) containing morphine. Because of the CNS effects (sedation,
respiratory depression, physical dependence), derivatives with mainly peripheral actions have been developed. Whereas diphenoxylate can still produce clear CNS effects, loperamide does not affect brain functions at normal dosage because it is pumped back into the blood by a P-glycoprotein located in capillary endothelial cells of the blood–brain barrier.
Loperamide is, therefore, the opioid antidiarrheal of first choice. The prolonged contact time for intestinal contents and mucosa may also improve absorption of fluid. With overdosage, there is a hazard of ileus. The drug is contraindicated in infants below age 2 years.
Antibacterial drugs. Use of these agents (e.g., co-trimoxazole, p.274) is only rational when bacteria are the cause of diarrhea. This is rarely the case. Note that antibiotics also damage the intestinal flora, which in turn can give rise to diarrhea.
Astringents such as tannic acid (home remedy: black tea) or metal salts precipitate surface proteins and are thought to help “seal” the mucosal epithelium. Protein denaturation must not include cellular proteins, for this would mean cell death. Although astringents induce constipation (cf. Al3+salts, p.170), a therapeutic effect in diarrhea is doubtful.
Demulcents, e.g., pectin (home remedy: grated apples) are carbohydrates that expand on absorbing water. They improve the consistency of bowel contents; beyond that they are devoid of any favorable effect.
|
|
|
Antidiarrheal Agents |
181 |
||
A. Antidiarrheals and their sites of action |
|
|
|
|||
|
|
|
Adsorption |
|
|
|
|
|
|
e.g., to |
|
|
|
|
|
|
medicinal |
|
|
|
|
|
Toxins |
charcoal |
|
|
|
|
|
|
Toxins |
|
|
|
|
|
Na+ |
|
|
|
|
|
|
Cl- |
|
|
|
|
|
|
|
Oral |
|
|
|
|
|
Fluid secretion |
rehydration |
|
|
|
|
|
|
solution: |
|
|
|
|
|
Na+ |
salts and |
|
|
|
|
|
|
glucose |
|
|
|
|
|
Glucose |
Antibacterial |
|
|
|
|
|
|
|
Resident |
|
|
|
|
|
drugs: e.g., co- |
|
||
|
|
|
microflora |
|
||
|
|
|
trimoxazole |
|
|
|
|
|
|
|
|
|
|
|
|
Pathogenic |
|
|
|
|
|
|
bacteria |
|
|
|
|
|
injury |
|
|
Opium tincture |
|
|
|
|
|
with morphine |
|
||
|
Mucosal |
|
|
|
|
CNS |
|
Viruses |
|
Diphenoxylate |
|
||
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
Loperamide |
|
|
|
|
|
|
|
Inhibition of |
|
|
|
|
|
|
propulsive |
|
peristalsis |
|
|
|
|
peristalsis |
|
|
|
|
|
Opioid |
|
|
|
|
|
|
receptors |
|
|
Enhanced |
|
Protein- |
|
|
|
|
|
containing |
|
|
|
||
|
mucus |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Astringents: |
|
|
|
|
|
|
e.g., tannic acid |
|
|
|
|
|
|
Precipitation of |
|
|
|
|
|
|
surface proteins, |
|
|
|
|
|
|
sealing of |
|
|
|
|
|
|
mucosa |
Fluid loss |
|
|
|
|
|
|
|
|
|
|
|
|
Diarrhea |
|
|
|
|

182 Drugs Acting on the Motor System
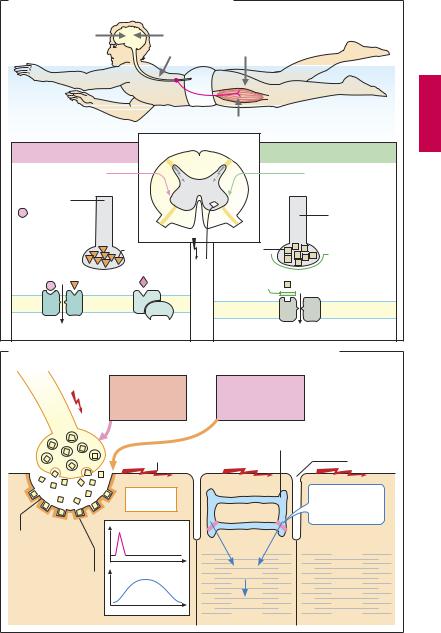
Drugs Affecting Motor Function
The smallest structural unit of skeletal musculature is the striated muscle fiber. It contracts in response to an impulse of “its” motor nerve. In executing motor programs, the brain sends impulses to the spinal cord. These converge on α-motoneurons in the anterior horn of the spinal medulla. Bundled in motor nerves, efferent axons course to skeletal muscles. Simple reflex contractions to sensory stimuli, conveyed via the dorsal roots to the motoneurons, occur without participation of the brain. Neural circuits that propagate afferent impulses into the spinal cord contain inhibitory interneurons. These serve to prevent a possible overexcitation of motoneurons (or excessive muscle contractions) due to the constant barrage of sensory stimuli.
Neuromuscular transmission (B) of motor nerve impulses to the striated muscle fiber takes place at the motor end plate. The nerve impulse liberates acetylcholine (ACh) from the axon terminal. ACh binds to nicotinic cholinoceptors at the motor end plate. This causes depolarization of the postsynaptic membrane, which in turn elicits a propagated action potential (AP) in the surrounding sarcolemma. The AP triggers a release of Ca2+ from its storage organelles, the sarcoplasmic reticulum (SR), within the muscle fiber; the rise in Ca2+ concentration induces a contraction (electromechanical coupling). Meanwhile, ACh is hydrolyzed by acetylcholinesterase (p.104); excitation of the end plate subsides. If no AP follows, Ca2+ is taken up again by the SR and the myofilaments relax.
Centrally-acting muscle relaxants (A) lower muscle tone by augmenting the activity of intraspinal inhibitory interneurons. They are used in the treatment of painful muscle spasms, e.g., in spinal disorders. Benzodiazepines enhance the effectiveness of the inhibitory transmitter GABA (p.222) at *$%$$ receptors, which are ligand-gated ion chan-
nels. Baclofen stimulates GABAB receptors, which are G-protein coupled.
The convulsants toxins tetanus toxin
(cause of wound tetanus) and strychnine, diminish the ef cacy of interneuronal synaptic inhibition mediated by the amino acid glycine (A). As a consequence of an unrestrained spread of impulses in the spinal cord, motor convulsions develop. Spasms of respiratory muscle groups endanger life.
Botulinus toxin from Clostridium botulinum is the most potent poison known. The estimated lethal dose for 50% of an exposed human population is ~ 1 × 10–9 g/kg (i.e., about 75 nanograms for an adult individual). The toxin, a zinc endopeptidase, blocks exocytosis of ACh in motor (and also parasympathetic) nerve endings. Death is caused by paralysis of respiratory muscles.
Targeted intramuscular injection of the toxin can produce a long-lasting localized paralysis. This procedure is used to treat pathological or painful muscle spasms (e.g., blepharospasm, esophageal achalasia, cervical dystonia). The same method is increasingly practiced in cosmetic surgery for removal of facial wrinkles (“face lift”). In focal hyperhidrosis (palmar, axillary, plantar), local injection of the toxin disrupts cholinergic sympathetic innervation, the effect of a single treatment lasting for several weeks.
A pathological rise in serum Mg2+ levels also causes inhibition of neuromuscular transmission.
Dantrolene interferes with electromechanical coupling in the muscle cell by inhibiting Ca2+ release from the SR. It isused to treat painful muscle spasms attending spinal diseases and skeletal muscle disorders involving excessive release of Ca2+ (malignant hyperthermia).
Drugs Affecting Motor Function |
183 |
A. Mechanisms for influencing skeletal muscle tone |
|
|
||
Antiepileptics |
Antiparkinsonian drugs |
|
||
|
Myotonolytics |
Dantrolene |
||
|
|
|
Muscle relaxants |
|
Myotonolytics |
|
|
|
Convulsants |
Increased inhibition |
|
|
|
Attenuated |
Inhibitory |
|
|
|
inhibition |
|
|
|
|
|
neuron |
|
|
|
Inhibitory |
|
|
|
|
interneuron |
Benzodiazepines |
|
|
|
Tetanus |
allosteric |
|
|
|
|
enhancement of |
GABA |
|
Glycine |
Toxin |
GABA effect |
|
|
|
Inhibition |
|
Agonist |
Strychnine |
of release |
|
Cl– |
Baclofen |
Receptor |
Cl- |
|
|
|
antagonist |
||
GABAA receptor |
GABAB receptor |
|
|
Glycine receptor |
B. Inhibition of neuromuscular transmission and electromechanical coupling |
||||
Motor |
Mg2+ |
|
Muscle relaxants |
|
axon |
Botulinum toxin |
inhibit generation |
||
|
inhibit |
|
of action |
|
|
ACh-release |
|
potential |
|
|
|
|
|
Sarcoplasmic |
|
|
|
|
reticulum |
|
|
Action potential |
t-Tubule |
|
ACh |
|
Depolari- |
|
Dantrolene |
|
|
|
||
|
|
zation |
|
inhibits |
|
|
|
|
Ca2+ release |
Motor |
Membrane potential |
|
||
|
|
|
Myofilaments |
|
end plate |
|
|
|
|
ACh receptor |
Muscle tone |
|
Ca2+ |
|
(nicotinic) |
|
|
|
|
|
ms |
10 |
20 |
Contraction |
|
|
|||
