
- •Preface to the 3rd edition
- •General Pharmacology
- •Systems Pharmacology
- •Therapy of Selected Diseases
- •Subject Index
- •Abbreviations
- •General Pharmacology
- •History of Pharmacology
- •Drug and Active Principle
- •The Aims of Isolating Active Principles
- •European Plants as Sources of Effective Medicines
- •Drug Development
- •Congeneric Drugs and Name Diversity
- •Oral Dosage Forms
- •Drug Administration by Inhalation
- •Dermatological Agents
- •From Application to Distribution in the Body
- •Potential Targets of Drug Action
- •External Barriers of the Body
- •Blood–Tissue Barriers
- •Membrane Permeation
- •Binding to Plasma Proteins
- •The Liver as an Excretory Organ
- •Biotransformation of Drugs
- •Drug Metabolism by Cytochrome P450
- •The Kidney as an Excretory Organ
- •Presystemic Elimination
- •Drug Concentration in the Body as a Function of Time—First Order (Exponential) Rate Processes
- •Time Course of Drug Concentration in Plasma
- •Time Course of Drug Plasma Levels during Repeated Dosing (A)
- •Time Course of Drug Plasma Levels during Irregular Intake (B)
- •Accumulation: Dose, Dose Interval, and Plasma Level Fluctuation (A)
- •Dose–Response Relationship
- •Concentration–Effect Curves (B)
- •Concentration–Binding Curves
- •Types of Binding Forces
- •Agonists—Antagonists
- •Other Forms of Antagonism
- •Enantioselectivity of Drug Action
- •Receptor Types
- •Undesirable Drug Effects, Side Effects
- •Drug Allergy
- •Cutaneous Reactions
- •Drug Toxicity in Pregnancy and Lactation
- •Pharmacogenetics
- •Placebo (A)
- •Systems Pharmacology
- •Sympathetic Nervous System
- •Structure of the Sympathetic Nervous System
- •Adrenergic Synapse
- •Adrenoceptor Subtypes and Catecholamine Actions
- •Smooth Muscle Effects
- •Cardiostimulation
- •Metabolic Effects
- •Structure–Activity Relationships of Sympathomimetics
- •Indirect Sympathomimetics
- •Types of
- •Antiadrenergics
- •Parasympathetic Nervous System
- •Cholinergic Synapse
- •Parasympathomimetics
- •Parasympatholytics
- •Actions of Nicotine
- •Localization of Nicotinic ACh Receptors
- •Effects of Nicotine on Body Function
- •Aids for Smoking Cessation
- •Consequences of Tobacco Smoking
- •Dopamine
- •Histamine Effects and Their Pharmacological Properties
- •Serotonin
- •Vasodilators—Overview
- •Organic Nitrates
- •Calcium Antagonists
- •ACE Inhibitors
- •Drugs Used to Influence Smooth Muscle Organs
- •Cardiac Drugs
- •Cardiac Glycosides
- •Antiarrhythmic Drugs
- •Drugs for the Treatment of Anemias
- •Iron Compounds
- •Prophylaxis and Therapy of Thromboses
- •Possibilities for Interference (B)
- •Heparin (A)
- •Hirudin and Derivatives (B)
- •Fibrinolytics
- •Intra-arterial Thrombus Formation (A)
- •Formation, Activation, and Aggregation of Platelets (B)
- •Inhibitors of Platelet Aggregation (A)
- •Presystemic Effect of ASA
- •Plasma Volume Expanders
- •Lipid-lowering Agents
- •Diuretics—An Overview
- •NaCl Reabsorption in the Kidney (A)
- •Aquaporins (AQP)
- •Osmotic Diuretics (B)
- •Diuretics of the Sulfonamide Type
- •Potassium-sparing Diuretics (A)
- •Vasopressin and Derivatives (B)
- •Drugs for Gastric and Duodenal Ulcers
- •Laxatives
- •Antidiarrheal Agents
- •Drugs Affecting Motor Function
- •Muscle Relaxants
- •Nondepolarizing Muscle Relaxants
- •Depolarizing Muscle Relaxants
- •Antiparkinsonian Drugs
- •Antiepileptics
- •Pain Mechanisms and Pathways
- •Eicosanoids
- •Antipyretic Analgesics
- •Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- •Cyclooxygenase (COX) Inhibitors
- •Local Anesthetics
- •Opioid Analgesics—Morphine Type
- •General Anesthesia and General Anesthetic Drugs
- •Inhalational Anesthetics
- •Injectable Anesthetics
- •Sedatives, Hypnotics
- •Benzodiazepines
- •Pharmacokinetics of Benzodiazepines
- •Therapy of Depressive Illness
- •Mania
- •Therapy of Schizophrenia
- •Psychotomimetics (Psychedelics, Hallucinogens)
- •Hypothalamic and Hypophyseal Hormones
- •Thyroid Hormone Therapy
- •Glucocorticoid Therapy
- •Follicular Growth and Ovulation, Estrogen and Progestin Production
- •Oral Contraceptives
- •Antiestrogen and Antiprogestin Active Principles
- •Aromatase Inhibitors
- •Insulin Formulations
- •Treatment of Insulin-dependent Diabetes Mellitus
- •Treatment of Maturity-Onset (Type II) Diabetes Mellitus
- •Oral Antidiabetics
- •Drugs for Maintaining Calcium Homeostasis
- •Drugs for Treating Bacterial Infections
- •Inhibitors of Cell Wall Synthesis
- •Inhibitors of Tetrahydrofolate Synthesis
- •Inhibitors of DNA Function
- •Inhibitors of Protein Synthesis
- •Drugs for Treating Mycobacterial Infections
- •Drugs Used in the Treatment of Fungal Infections
- •Chemotherapy of Viral Infections
- •Drugs for the Treatment of AIDS
- •Drugs for Treating Endoparasitic and Ectoparasitic Infestations
- •Antimalarials
- •Other Tropical Diseases
- •Chemotherapy of Malignant Tumors
- •Targeting of Antineoplastic Drug Action (A)
- •Mechanisms of Resistance to Cytostatics (B)
- •Inhibition of Immune Responses
- •Antidotes and Treatment of Poisonings
- •Therapy of Selected Diseases
- •Hypertension
- •Angina Pectoris
- •Antianginal Drugs
- •Acute Coronary Syndrome— Myocardial Infarction
- •Congestive Heart Failure
- •Hypotension
- •Gout
- •Obesity—Sequelae and Therapeutic Approaches
- •Osteoporosis
- •Rheumatoid Arthritis
- •Migraine
- •Common Cold
- •Atopy and Antiallergic Therapy
- •Bronchial Asthma
- •Emesis
- •Alcohol Abuse
- •Local Treatment of Glaucoma
- •Further Reading
- •Further Reading
- •Picture Credits
- •Drug Indexes

258 Hormones
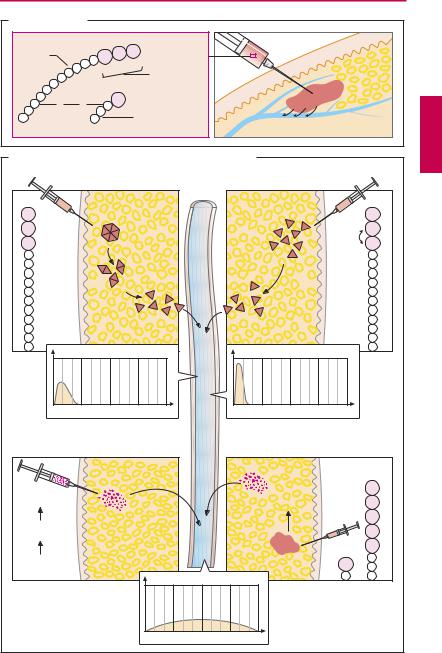
Insulin Formulations
Insulin is synthesized in the B- (or β-) cells of the pancreatic islets of Langerhans. It is a protein (MW 5800) consisting of two peptide chains linked by two disulfide bridges; the A chain has 21 and the B chain 30 amino acids. Upon ingestion of carbohydrates, insulin is released into the blood and promotes uptake and utilization of glucose in specific organs, namely, the heart, adipose tissue, and skeletal muscle.
Insulin is used in the replacement therapy of diabetes mellitus.
Sources of therapeutic insulin preparations
(A). Porcine insulin differs from human insulin by one B-chain amino acid. Owing to the slightness of this difference, its biological activity is similar to that of human hormone.
Human insulin is produced by two methods: biosynthetically from porcine insulin, by exchanging the wrong amino acid; or by gene technology involving synthesis in E. coli bacteria.
Recombinant insulin is produced to modify pharmacokinetic properties (see below). It is important in these insulin analogues that specificity for the insulin receptor is preserved (e.g., also toward the receptor for IGF-1 = somatomedin C, which promotes proliferation of cells; p.238).
Control of delivery from injection site into blood (B). As a peptide, insulin is unsuitable for oral administration (owing to destruction by gastrointestinal proteases) and thus needs to be given parenterally. Usually, insulin preparations are injected subcutaneously. The duration of action depends on the rate of absorption from the injection site.
Variations in Dosage Form
Insulin solution. Dissolved insulin is dispensed as a clear neutral solution known as regular (R) insulin or crystalline zinc insulin. Inemergencies,suchashyperglycemiccoma,
it can be given intravenously (mostly by infusion because i.v. injections have too short an action; plasma t½ ~ 9 minutes). With the usual subcutaneous application, the effect is evident within 15–20 minutes, reaches a peak after ~ 3 hours, and lasts for ~ 6 hours.
Insulin suspensions. When it is injected as a suspension of insulin-containing particles, dissolution and release of the hormone in subcutaneous tissue is retarded (extendedaction insulins). Suitable particles can be obtained by precipitation of apolar, poorly water-soluble complexes consisting of anionic insulin and cationic partners, e.g., the polycationic protein protamine. In the presence of zinc ions, insulin crystallizes; crystal size determines the rate of dissolution. Intermediate-acting insulin preparations (NPH or isophane; Lente) act for 18–26 hours, slow-acting preparations (protamine zinc, ultralente) for up to 36 hours.
Variation in Amino Acid Sequence
Rapidly acting insulin analogues. After injection of a regular insulin solution, insulin molecules exist at the injection site in the form of hexameric aggregates. Only after disintegration into monomers can rapid diffusion into the bloodstream occur. In insulin lispro, two amino acids are exchanged, resulting in a diminished propensity toward aggregate formation. Thus, diffusion from the injection site is faster, with rapid onset and short duration of action. Insulin aspart hassimilarproperties.Fast-actinginsulinsare injected immediately before a meal, whereas regularinsulinrequiresa15–30minuteinter- val between injection and food intake.
Long-acting insulin analogues. The more extensive alteration of amino acids in insulin glargine changes the electric charge of the molecule. At pH 4 of the injectate, it is dissolved; however, at the pH of tissue it is poorly water-soluble and precipitates. Resolubilization and diffusion into the bloodstream take about one day.
|
|
|
|
Insulin Formulations |
259 |
A. Human insulin |
|
|
|
|
|
B-chain |
|
|
|
Subcutaneous insulin injection |
|
|
Pro Lys Thr |
|
|||
|
|
28 |
29 |
30 |
|
|
|
|
C-terminus |
|
|
|
|
|
|
|
|
S |
S |
|
Asn 21 |
|
|
|
|
A-chain |
|
||
|
|
|
|
|
|
B. Control of release from injection site into bloodstream |
|
|
|
|
|||||||
Human insulin solution |
|
Blood- |
Variation in amino acid sequence |
|
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
stream |
|
|
|
|
|
|
Thr 30 |
|
|
|
|
|
|
|
|
|
|
Thr 30 |
Lys 29 |
|
|
Hexamer |
|
|
|
|
|
|
|
Pro 29 |
Pro 28 |
Insulin |
|
|
|
|
|
|
|
Insulin lispro |
Lys 28 |
|
|
|
Dimers |
|
|
|
|
|
|
|||
|
solution |
|
|
|
|
|
solution |
|
|||
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
No aggregate |
|
||
|
|
Monomers |
|
|
|
|
formation |
|
|
||
|
|
|
|
|
|
|
|
|
|
||
|
Insulin concentration in blood |
|
|
|
Insulin concentration in blood |
|
|||||
0 |
6 |
12 |
18 |
h |
|
0 |
6 |
12 |
18 |
h |
|
Variation in formulation |
|
|
|
Variation in amino acid sequence |
|||||||
Insulin |
|
|
|
|
|
|
|
Precipitation |
Insulin |
Arg 32 |
|
suspension |
|
|
|
|
|
|
of crystals |
glargine |
Arg 31 |
||
|
|
|
|
|
|
|
|
solution |
|||
Crystal |
|
|
|
|
|
|
|
|
|
(pH 4) |
Thr 30 |
|
|
|
|
|
|
|
|
|
|
Lys 29 |
|
formation |
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
Pro 28 |
Addition |
|
|
|
|
|
|
|
Tissue |
|
Gly 21 |
|
of zinc ions |
|
Insulin concentration in blood |
(pH 7) |
|
|
||||||
|
|
|
|
|
|
|
|||||
|
|
|
0 |
6 |
12 |
18 |
h |
|
|
|
|

260 Hormones
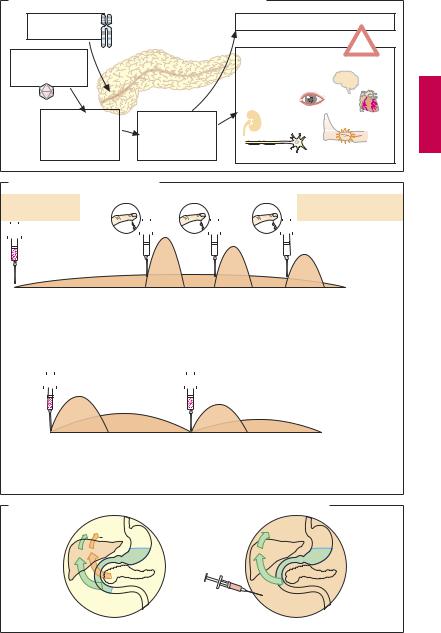
Treatment of Insulin-dependent Diabetes Mellitus
Pathogenesis and complications (A). Type I diabetesmellitustypicallymanifestsinchildhood or adolescence (juvenile onset diabetes mellitus); it is caused by the destruction of insulin-producing B cells in the pancreas. A genetic predisposition together with a precipitating factor (viral infection) could start an autoimmune reaction against B-cells. Replacement of insulin (daily dose ~ 40 U, equivalent to ~ 1.6 mg) becomes necessary.
Therapeutic objectives. (1) prevention of life-threatening hyperglycemic (diabetic) coma; (2) prevention of diabetic sequelae arising from damage to small and large blood vessels, precise “titration” of the patient being essential to avoid even shortterm spells of pathological hyperglycemia;
(3) prevention of insulin overdosage leading to life-threatening hypoglycemic shock (CNS disturbance due to lack of glucose).
Therapeutic principles. In healthy subjects, the amount of insulin is “automatically” matched to carbohydrate intake, hence to blood glucose concentration. The critical secretory stimulus is the rise in plasma glucose level. Food intake and physical activity (increased glucoseuptakeinto musculature,decreased insulindemand) areaccompanied by corresponding changes in insulin secretion.
Methods of insulin replacement (B). In the diabetic, insulin can be administered as it is normally secreted. For instance, administration of a long-acting insulin in the late evening generates a basal level, whereas a fast acting insulin is used before meals. The dose needed is determined on the basis of the actual blood glucose concentration mea- suredbythepatientandthemeal-dependent demand. This regimen (so-called intensified insulin therapy) provides the patient with much flexibility in planning daily activities. A well-educated, cooperative, and compe-
tent patient is a precondition. In other cases, a fixed-dosage schedule (conventional insulin therapy) will be needed, e.g., with morning and evening injections of a combination insulin (a mixture of regular insulin plus insulin suspension) in constant respective dosage (A). To avoid hypoglycemia or hyperglycemia, dietary carbohydrate (CH) intake must be synchronized with the time course of insulin absorption from the s.c. depot: diet control! Caloric intake is to be distributed (50% CH, 30% fat, 20% protein) in small meals over the day so as to achieve a steady CH supply—snacks, late night meal. Rapidly absorbable CH (sweets, cakes) must be avoided (hyperglycemic peaks) and replaced with slowly digestible ones.
Undesirable Effects
Hypoglycemia is heralded by warning signs: tachycardia, unrest, tremor, pallor, profuse sweating. Some of these are due to the release of glucose-mobilizing epinephrine. Counter-measures: glucose administration, rapidly absorbed CH orally (diabetics should always have a suitable preparation within reach)or10–20 gglucosei.v.incaseofunconsciousness; if necessary, injection of glucagon, the pancreatic hyperglycemic hormone.
Allergic reactions are rare; locally, redness may occur at the injection site and atrophy of adipose tissue; lipodystrophy). A possible local lipohypertrophy can be avoided by alternating injection sites.
Evenwithoptimalcontrolofbloodsugar,s. c. administration of insulin cannot fully replicate the physiological situation. In healthy subjects, absorbed glucose and insulin released from the pancreas simultaneously reach the liver in high concentrations, whereby effective presystemic elimination of both substances is achieved. In the diabetic, s.c. injected insulin is uniformly distributed in the body. Since insulin concentration in blood supplying the liver cannot rise, less glucose is extracted from portal blood. A significant amount of glucose enters extrahepatic tissues, where it has to be utilized.
Treatment of IDDM |
261 |
A. Diabetes mellitus type I: pathogenesis and complications |
|
|||
Genetic |
|
Diabetic coma |
|
|
disposition |
|
|
! |
|
Environmental |
|
Diabetic microand |
||
|
|
|||
factors, e.g., |
|
macroangiopathy |
|
|
viral infection |
|
Late organ damage |
Stroke |
|
|
|
Retinopathy |
|
|
Autoimmune |
Absolute insulin |
Nephropathy |
Myocardial |
|
infarction |
||||
destruction of |
deficiency |
|
||
|
|
|||
B-cells in islets |
Hyperglycemia |
|
Peripheral obliterating |
|
of Langerhans |
Neuropathy |
|||
|
|
|
arterial disease |
|
B. Methods of insulin replacement
Extended-action |
Blood glucose measurement |
Rapid-acting insulin: |
insulin |
|
flexible time and dose |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
22 |
|
|
24 |
|
4 |
|
8 |
|
12 |
|
|
|
|
|
|
|
16 |
20 |
22 |
|
||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Breakfast |
|
|
|
|
|
Lunch |
|
|
Dinner |
Food intake: |
|
||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
flexible |
|
|||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
1. Intensified insulin therapy |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Combination |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Insulin administration: |
||||||||||||||
|
insulin |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
fixed schedule |
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
4 |
|
|
8 |
|
12 |
|
16 |
|
20 |
|
|
|
|
|
|
|
24 |
4 |
8 |
|
||||||||||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Breakfast |
|
|
Lunch |
|
|
|
|
|
|
|
|
|
Dinner |
|
|
|
|
|
|
|
|
|
|
Food intake: |
|
||||||||||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
& snacks |
|
|
|
|
|
|
|
|
|
Supper |
|
|
|
|
|
|
|
|
|
|
fixed schedule |
|
||||||||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
2.Conventional insulin therapy
C. Presystemic and systemic insulin action in healthy and diabetic subjects
Insulin
Glucose
 Glucose
Glucose
InsulinInsulin
Healthy subject |
Diabetic |
