
- •Preface to the 3rd edition
- •General Pharmacology
- •Systems Pharmacology
- •Therapy of Selected Diseases
- •Subject Index
- •Abbreviations
- •General Pharmacology
- •History of Pharmacology
- •Drug and Active Principle
- •The Aims of Isolating Active Principles
- •European Plants as Sources of Effective Medicines
- •Drug Development
- •Congeneric Drugs and Name Diversity
- •Oral Dosage Forms
- •Drug Administration by Inhalation
- •Dermatological Agents
- •From Application to Distribution in the Body
- •Potential Targets of Drug Action
- •External Barriers of the Body
- •Blood–Tissue Barriers
- •Membrane Permeation
- •Binding to Plasma Proteins
- •The Liver as an Excretory Organ
- •Biotransformation of Drugs
- •Drug Metabolism by Cytochrome P450
- •The Kidney as an Excretory Organ
- •Presystemic Elimination
- •Drug Concentration in the Body as a Function of Time—First Order (Exponential) Rate Processes
- •Time Course of Drug Concentration in Plasma
- •Time Course of Drug Plasma Levels during Repeated Dosing (A)
- •Time Course of Drug Plasma Levels during Irregular Intake (B)
- •Accumulation: Dose, Dose Interval, and Plasma Level Fluctuation (A)
- •Dose–Response Relationship
- •Concentration–Effect Curves (B)
- •Concentration–Binding Curves
- •Types of Binding Forces
- •Agonists—Antagonists
- •Other Forms of Antagonism
- •Enantioselectivity of Drug Action
- •Receptor Types
- •Undesirable Drug Effects, Side Effects
- •Drug Allergy
- •Cutaneous Reactions
- •Drug Toxicity in Pregnancy and Lactation
- •Pharmacogenetics
- •Placebo (A)
- •Systems Pharmacology
- •Sympathetic Nervous System
- •Structure of the Sympathetic Nervous System
- •Adrenergic Synapse
- •Adrenoceptor Subtypes and Catecholamine Actions
- •Smooth Muscle Effects
- •Cardiostimulation
- •Metabolic Effects
- •Structure–Activity Relationships of Sympathomimetics
- •Indirect Sympathomimetics
- •Types of
- •Antiadrenergics
- •Parasympathetic Nervous System
- •Cholinergic Synapse
- •Parasympathomimetics
- •Parasympatholytics
- •Actions of Nicotine
- •Localization of Nicotinic ACh Receptors
- •Effects of Nicotine on Body Function
- •Aids for Smoking Cessation
- •Consequences of Tobacco Smoking
- •Dopamine
- •Histamine Effects and Their Pharmacological Properties
- •Serotonin
- •Vasodilators—Overview
- •Organic Nitrates
- •Calcium Antagonists
- •ACE Inhibitors
- •Drugs Used to Influence Smooth Muscle Organs
- •Cardiac Drugs
- •Cardiac Glycosides
- •Antiarrhythmic Drugs
- •Drugs for the Treatment of Anemias
- •Iron Compounds
- •Prophylaxis and Therapy of Thromboses
- •Possibilities for Interference (B)
- •Heparin (A)
- •Hirudin and Derivatives (B)
- •Fibrinolytics
- •Intra-arterial Thrombus Formation (A)
- •Formation, Activation, and Aggregation of Platelets (B)
- •Inhibitors of Platelet Aggregation (A)
- •Presystemic Effect of ASA
- •Plasma Volume Expanders
- •Lipid-lowering Agents
- •Diuretics—An Overview
- •NaCl Reabsorption in the Kidney (A)
- •Aquaporins (AQP)
- •Osmotic Diuretics (B)
- •Diuretics of the Sulfonamide Type
- •Potassium-sparing Diuretics (A)
- •Vasopressin and Derivatives (B)
- •Drugs for Gastric and Duodenal Ulcers
- •Laxatives
- •Antidiarrheal Agents
- •Drugs Affecting Motor Function
- •Muscle Relaxants
- •Nondepolarizing Muscle Relaxants
- •Depolarizing Muscle Relaxants
- •Antiparkinsonian Drugs
- •Antiepileptics
- •Pain Mechanisms and Pathways
- •Eicosanoids
- •Antipyretic Analgesics
- •Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- •Cyclooxygenase (COX) Inhibitors
- •Local Anesthetics
- •Opioid Analgesics—Morphine Type
- •General Anesthesia and General Anesthetic Drugs
- •Inhalational Anesthetics
- •Injectable Anesthetics
- •Sedatives, Hypnotics
- •Benzodiazepines
- •Pharmacokinetics of Benzodiazepines
- •Therapy of Depressive Illness
- •Mania
- •Therapy of Schizophrenia
- •Psychotomimetics (Psychedelics, Hallucinogens)
- •Hypothalamic and Hypophyseal Hormones
- •Thyroid Hormone Therapy
- •Glucocorticoid Therapy
- •Follicular Growth and Ovulation, Estrogen and Progestin Production
- •Oral Contraceptives
- •Antiestrogen and Antiprogestin Active Principles
- •Aromatase Inhibitors
- •Insulin Formulations
- •Treatment of Insulin-dependent Diabetes Mellitus
- •Treatment of Maturity-Onset (Type II) Diabetes Mellitus
- •Oral Antidiabetics
- •Drugs for Maintaining Calcium Homeostasis
- •Drugs for Treating Bacterial Infections
- •Inhibitors of Cell Wall Synthesis
- •Inhibitors of Tetrahydrofolate Synthesis
- •Inhibitors of DNA Function
- •Inhibitors of Protein Synthesis
- •Drugs for Treating Mycobacterial Infections
- •Drugs Used in the Treatment of Fungal Infections
- •Chemotherapy of Viral Infections
- •Drugs for the Treatment of AIDS
- •Drugs for Treating Endoparasitic and Ectoparasitic Infestations
- •Antimalarials
- •Other Tropical Diseases
- •Chemotherapy of Malignant Tumors
- •Targeting of Antineoplastic Drug Action (A)
- •Mechanisms of Resistance to Cytostatics (B)
- •Inhibition of Immune Responses
- •Antidotes and Treatment of Poisonings
- •Therapy of Selected Diseases
- •Hypertension
- •Angina Pectoris
- •Antianginal Drugs
- •Acute Coronary Syndrome— Myocardial Infarction
- •Congestive Heart Failure
- •Hypotension
- •Gout
- •Obesity—Sequelae and Therapeutic Approaches
- •Osteoporosis
- •Rheumatoid Arthritis
- •Migraine
- •Common Cold
- •Atopy and Antiallergic Therapy
- •Bronchial Asthma
- •Emesis
- •Alcohol Abuse
- •Local Treatment of Glaucoma
- •Further Reading
- •Further Reading
- •Picture Credits
- •Drug Indexes

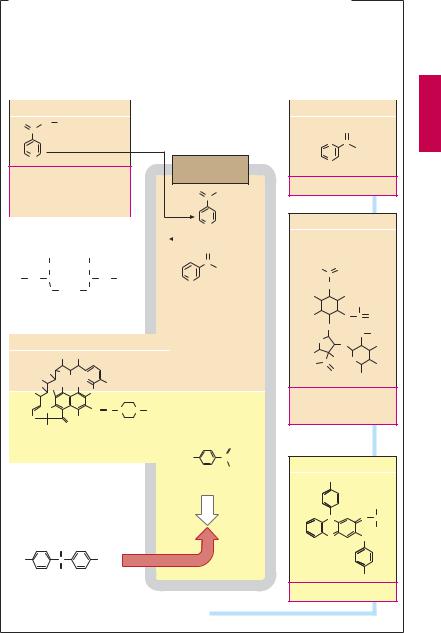
282 Antibacterial Drugs
Drugs for Treating Mycobacterial Infections
In the past 100 years, advances in hygiene have led to a drastic decline in tubercular diseases in central Europe. Infection with
Mycobacterium tuberculosis could be diagnosed increasingly earlier and in most cases be cured by a systematic long-term therapy (6–12 months) with effective chemotherapeutics. Worldwide, however, tuberculosis has remained one of the most threatening diseases. In developing countries, long-term combination therapy is scarcely realizable. Therapeutic success is thwarted by a lack of adequate (medical) infrastructure and financial resources, and insuf cient compliance of patients; as a result, millions of persons die annually of tuberculosis infections. The insuf cient treatment entails an additional bad consequence: more and more mycobacterial strains develop resistance and cannot be adequately treated. Patients suffering from immune deficiency are affected more severely by infections with M. tuberculosis.
Antitubercular drugs (1)
Drugs of choice are isoniazid, rifampin, and ethambutol, along with streptomycin and pyrazinamide. Less well tolerated, secondline agents include p-aminosalicylic acid, cycloserine, viomycin, kanamycin, amikacin, capreomycin, and ethionamide.
Isoniazid is bactericidal against growing M. tuberculosis. Its mechanism of action remains unclear. In the bacterium it is converted to isonicotinic acid, which is membrane impermeable and hence likely to accumulate intracellularly. Isoniazid is rapidly absorbed after oral administration. In the liver, it is inactivated by acetylation. Notable adverse effects are peripheral neuropathy, optic neuritis preventable by administration of vitamin B6 (pyridoxine), and liver damage.
Rifampin. Source, antibacterial activity, and routes of administration are described on p.276. Although mostly well tolerated, this drug may cause several adverse effects
including hepatic damage, hypersensitivity with flulike symptoms, disconcerting but harmless red/orange discoloration of body fluids, and enzyme induction (failure of oral contraceptives). Concerning rifabutin, see
p.276.
Pyrazinamide exerts a bactericidal action
byan unknown mechanism. Itisgiven orally. Pyrazinamide may impair liver function; hyperuricemia results from inhibition of renal urate elimination.
Streptomycin must be given i.v. like other aminoglycoside antibiotics (p.280). It damages the inner ear and the labyrinth. Its nephrotoxicity is comparatively minor
Ethambutol. The cause of ethambutol’s specific antitubercular action is unknown. It is given orally. It is generally well tolerated, but may cause dose-dependent reversible disturbances of vision (red/green blindness, visual field defects).
Antileprotic drugs (2)
Rifampin is frequently given in combination with one or both of the following twoagents.
Dapsone is a sulfone that, like sulfonamides, inhibits dihydrofolate synthesis (p.274). It is bactericidal against susceptible strains of M. leprae. Dapsone is given orally. The most frequent adverse effect is methemoglobinemia with accelerated erythrocyte degradation (hemolysis).
Clofazimine is a dye with bactericidal activity against M. leprae and anti-inflamma- tory properties. It is given orally but is incompletely absorbed. Because of its high lipophilicity, it accumulates in adipose and other tissues and leaves the body only rather slowly (t½ ~ 70 days). Red-brown skin pigmentation is an unwanted effect, particularly in fair-skinned patients.
Drugs for Treating Mycobacterial Infections |
283 |
A. Drugs used to treat infections with mycobacteria (1. tuberculosis, 2. leprosy)
|
|
|
Combination therapy |
|
||
|
Reduced risk of |
|
Reduction of dose and of |
|
||
|
bacterial resistance |
|
risk of adverse reactions |
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Isoniazid |
|
|
Pyrazinamide |
|||
ONH NH2
C |
|
|
O |
|
|
|
|
N C |
|
|
|
|
NH2 |
|
N |
Mycobacterium |
N |
||
CNS damage |
||||
tuberculosis |
|
|||
and peripheral |
|
|
Liver damage |
|
neuropathy |
O |
OH |
||
|
||||
(Vit. B6 administration) |
|
C |
|
|
Liver damage |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
N |
||
Ethambutol |
|
|
|
|
|
|
|
|
|
Isonicotinic acid |
||||||
|
|
|
|
|
|
|
|
|
||||||||
|
|
CH3 |
|
|
CH3 |
|
|
|
|
|
|
|
|
O |
||
|
|
|
|
|
|
|
|
|
|
|
|
C |
||||
|
|
CH2 |
|
|
CH2 |
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
OH |
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
HO CH2 |
CH |
|
|
HC CH2 |
OH |
|
|
|
|
|
N |
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
HN |
(CH2)2 |
NH |
|
|
|
|
|
|
|
Nicotinic acid |
||||
Optic nerve damage |
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Rifampicin |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
H3C |
CH3 |
|
|
|
|
|
|
|
|
|
|
|
||
|
H3C |
OH |
|
|
|
|
|
|
|
|
|
|
1. |
|||
H3CCOO |
|
OH |
O |
CH3 |
|
|
|
|
|
|
|
|||||
|
H3C |
CH3OH |
OH |
|
|
|
|
|
|
|
|
|
|
|||
H3CO |
O |
|
|
NH |
N |
N N CH3 |
|
|
|
2. |
||||||
|
|
|
|
CH |
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|||||||
|
O |
|
O |
OH |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
CH3 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Liver damage |
|
|
|
|
|
|
|
|
|
|
|
O |
||||
and enzyme induction |
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
|
|
|
|
H2N |
|
C |
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
OH |
|
|
|
|
|
|
|
|
|
|
|
|
p-Aminobenzoic acid |
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Folate |
|
Dapsone |
|
|
|
|
|
|
|
|
|
|
|
|
synthesis |
|||
|
|
|
O |
|
|
|
|
|
|
|
|
|
|
|
|
|
H2N |
|
S |
|
NH2 |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
O |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Mycobacterium |
|
||
Hemolysis |
|
|
|
|
|
|
|
|
|
|
|
leprae |
|
|||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Streptomycin
an aminoglycoside antibiotic
H2N |
C |
NH |
|
|
|
|
NH |
|
|
||
HO |
|
OH |
|
||
|
|
|
NH2 |
||
HO |
|
N |
C |
NH |
|
|
O |
H |
|
|
|
|
|
HN |
CH3 |
||
O |
|
|
|||
|
O |
|
OH |
||
|
|
|
|||
H3C |
C |
OH |
O |
|
|
H |
OH |
||||
|
|
|
|||
OCH2OH
Vestibular and cochlear ototoxicity
Clofazimine
Cl
CH3
NN CH
CH3
NNH
Cl
Skin discoloration

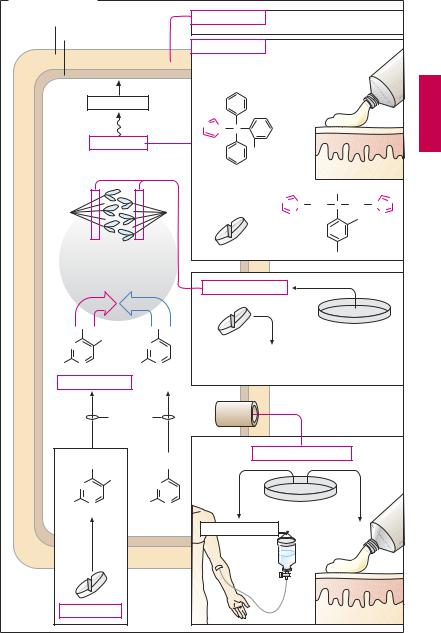
284 Antifungal Drugs
Drugs Used in the Treatment of Fungal Infections
Infections due to fungi are usually confined to the skin or mucous membranes: local or superficial mycosis. However, in immune deficiency states, internal organs may also be affected: systemic or deep mycosis.
Mycoses are most commonly due to dermatophytes, which affect the skin, hair, and nails following external infection, and to Candida albicans, a yeast organism normally found on body surfaces, which may cause infections of mucous membranes, less frequently of the skin or internal organs when natural defenses are impaired (immunosuppression, or damage of microflora by broadspectrum antibiotics).
Imidazole derivatives inhibit synthesis of ergosterol, an integral constituent of cytoplasmic membranes of fungal cells. Fungi stop growing (fungistatic effect) or die (fungicidal effect). The spectrum of affected fungi is very broad. Because they are poorly absorbed and poorly tolerated systemically, most imidazoles are suitable only for topical use (clotrimazole, econazole, oxiconazole and other azoles). Fluconazole and itroconazole are newer orally effective triazole derivatives. Owing to its hydroxyl group, fluconazole is suf ciently water-soluble to allow formulation as an injectable solution. Both substances are slowly eliminated (plasma t½ ~ 30 hours). The topically active allyl amine naftidine and the morpholine amorolfine also inhibit ergosterol synthesis, albeit at a different step. Both are for topical use.
The polyene antibiotics amphotericin B and nystatin are of bacterial origin. They insert themselves into fungal cell membranes (probably next to ergosterol molecules) and cause formation of hydrophilic channels. Amphotericin B is active against most organisms responsible for systemic mycoses. Because polyene antimycotics are nonabsorbable, it must be given by infusion, which is, however, poorly tolerated (chills, fever, CNS disturbances, impaired renal function, and
phlebitis at the infusion site). Applied topically to skin or mucous membranes, amphotericin B is useful in the treatment of candidal mycosis. Because of the low rate of enteral absorption, oral administration in intestinal candidiasis can be considered a topical treatment. Likewise, nystatin is only used topically (e.g., oral cavity, gastrointestinal tract) against candidiasis.
Flucytosine is converted in candidal fungi to 5-fluorouracil by the action of a specific fungal cytosine deaminase. As an antimetabolite, this compound disrupts DNA and RNA synthesis (p.300), resulting in a fungicidal effect. Given orally, flucytosine is rapidly absorbed. It is often combined with amphotericin B to allow dose reduction of the latter.
Caspofungin is a cyclic polypeptide that inhibits synthesis of the fungal cell wall. It can be used in systemic mycoses due to aspergillus fungi when amphotericin B or itroconazole cannot be employed. It is given by infusion and causes various adverse effects.
Griseofulvin originates from molds and has activity only against dermatophytes. It presumably acts as a spindle poison to inhibit fungal mitosis. Although targeted against local mycoses, griseofulvin must be used systemically. It is incorporated into newly-formed keratin. “Impregnated” in this manner, keratin becomes unsuitable as a fungal nutrient. The time required for the eradication of dermatophytes corresponds to the renewal period of skin, hair, or nails. Griseofulvin may cause uncharacteristic adverse effects. Because of its cumbersome application, this antimycotic is becoming obsolete.
Drugs Used in the Treatment of Fungal Infections |
285 |
A. Antifungal drugs |
|
|
|
|
|
|
|
|
|
Cell wall |
|
|
|
Caspofungin |
Inhibition of |
|
|
||
|
|
|
|
|
cell wall synthesis |
|
|||
Cytoplasmic membrane |
|
|
|
||||||
Azoles |
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Imidazoles topical, |
|
|
|
|
|
|
|
|
|
e.g., clotrimazole |
|
|
|
|
|
|
Ergosterol |
|
|
|
|
|
|
|
|
|
|
|
|
N |
C |
|
|
|
|
|
|
|
|
N |
|
|
|
|
|
|
Synthesis |
|
|
|
|
|
|
|
|
|
|
|
|
|
Cl |
|
|
|
|
|
|
|
|
Triazoles systemic, |
|
|
|
|
|
|
|
|
|
e.g., fluconazole |
|
OH |
|
|
|
|
|
|
|
|
|
N |
|
N |
|
|
|
|
|
|
|
C |
CH2 |
||
|
|
|
|
|
|
N CH2 |
N |
||
|
|
|
|
|
|
N |
|
F |
N |
|
|
|
|
|
|
|
|
|
|
|
Mitotic spindle |
|
|
|
|
|
|
|
|
|
DNA/RNA |
|
|
|
|
F |
|
|
|
|
|
|
|
|
|
|
|
||
|
metabolism |
|
|
|
|
|
|
|
|
|
|
|
|
Griseofulvin |
|
|
|
|
|
|
OH |
|
OH |
|
|
|
Mold fungi |
||
|
F |
|
|
|
|
|
|||
N |
N |
|
|
|
|
|
|
|
|
|
|
Incorporation into |
|
|
|
|
|||
|
|
|
|
|
|
|
|
||
HO |
N |
HO |
N |
growing skin, hair, nails |
|
|
|
||
“Impregnation effect” |
|
|
|
||||||
|
|
|
|
|
|
|
|||
5-Fluorouracil |
Uracil |
|
|
|
|
|
|
||
cell |
|
Cytosine |
|
|
|
|
|
|
|
Fungal |
|
deaminase |
|
|
|
|
|
|
|
|
|
|
|
Polyene Antibiotics |
|
|
|||
|
|
|
|
|
|
|
|||
|
NH 2 |
|
NH 2 |
|
|
|
|
|
|
|
N |
F |
N |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
HO |
N |
HO |
N |
|
Streptomyces bacteria |
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
Amphotericin B |
|
Nystatin |
|
||
Flucytosine |
|
|
|
|
|
|
|
||
