
- •Preface to the 3rd edition
- •General Pharmacology
- •Systems Pharmacology
- •Therapy of Selected Diseases
- •Subject Index
- •Abbreviations
- •General Pharmacology
- •History of Pharmacology
- •Drug and Active Principle
- •The Aims of Isolating Active Principles
- •European Plants as Sources of Effective Medicines
- •Drug Development
- •Congeneric Drugs and Name Diversity
- •Oral Dosage Forms
- •Drug Administration by Inhalation
- •Dermatological Agents
- •From Application to Distribution in the Body
- •Potential Targets of Drug Action
- •External Barriers of the Body
- •Blood–Tissue Barriers
- •Membrane Permeation
- •Binding to Plasma Proteins
- •The Liver as an Excretory Organ
- •Biotransformation of Drugs
- •Drug Metabolism by Cytochrome P450
- •The Kidney as an Excretory Organ
- •Presystemic Elimination
- •Drug Concentration in the Body as a Function of Time—First Order (Exponential) Rate Processes
- •Time Course of Drug Concentration in Plasma
- •Time Course of Drug Plasma Levels during Repeated Dosing (A)
- •Time Course of Drug Plasma Levels during Irregular Intake (B)
- •Accumulation: Dose, Dose Interval, and Plasma Level Fluctuation (A)
- •Dose–Response Relationship
- •Concentration–Effect Curves (B)
- •Concentration–Binding Curves
- •Types of Binding Forces
- •Agonists—Antagonists
- •Other Forms of Antagonism
- •Enantioselectivity of Drug Action
- •Receptor Types
- •Undesirable Drug Effects, Side Effects
- •Drug Allergy
- •Cutaneous Reactions
- •Drug Toxicity in Pregnancy and Lactation
- •Pharmacogenetics
- •Placebo (A)
- •Systems Pharmacology
- •Sympathetic Nervous System
- •Structure of the Sympathetic Nervous System
- •Adrenergic Synapse
- •Adrenoceptor Subtypes and Catecholamine Actions
- •Smooth Muscle Effects
- •Cardiostimulation
- •Metabolic Effects
- •Structure–Activity Relationships of Sympathomimetics
- •Indirect Sympathomimetics
- •Types of
- •Antiadrenergics
- •Parasympathetic Nervous System
- •Cholinergic Synapse
- •Parasympathomimetics
- •Parasympatholytics
- •Actions of Nicotine
- •Localization of Nicotinic ACh Receptors
- •Effects of Nicotine on Body Function
- •Aids for Smoking Cessation
- •Consequences of Tobacco Smoking
- •Dopamine
- •Histamine Effects and Their Pharmacological Properties
- •Serotonin
- •Vasodilators—Overview
- •Organic Nitrates
- •Calcium Antagonists
- •ACE Inhibitors
- •Drugs Used to Influence Smooth Muscle Organs
- •Cardiac Drugs
- •Cardiac Glycosides
- •Antiarrhythmic Drugs
- •Drugs for the Treatment of Anemias
- •Iron Compounds
- •Prophylaxis and Therapy of Thromboses
- •Possibilities for Interference (B)
- •Heparin (A)
- •Hirudin and Derivatives (B)
- •Fibrinolytics
- •Intra-arterial Thrombus Formation (A)
- •Formation, Activation, and Aggregation of Platelets (B)
- •Inhibitors of Platelet Aggregation (A)
- •Presystemic Effect of ASA
- •Plasma Volume Expanders
- •Lipid-lowering Agents
- •Diuretics—An Overview
- •NaCl Reabsorption in the Kidney (A)
- •Aquaporins (AQP)
- •Osmotic Diuretics (B)
- •Diuretics of the Sulfonamide Type
- •Potassium-sparing Diuretics (A)
- •Vasopressin and Derivatives (B)
- •Drugs for Gastric and Duodenal Ulcers
- •Laxatives
- •Antidiarrheal Agents
- •Drugs Affecting Motor Function
- •Muscle Relaxants
- •Nondepolarizing Muscle Relaxants
- •Depolarizing Muscle Relaxants
- •Antiparkinsonian Drugs
- •Antiepileptics
- •Pain Mechanisms and Pathways
- •Eicosanoids
- •Antipyretic Analgesics
- •Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
- •Cyclooxygenase (COX) Inhibitors
- •Local Anesthetics
- •Opioid Analgesics—Morphine Type
- •General Anesthesia and General Anesthetic Drugs
- •Inhalational Anesthetics
- •Injectable Anesthetics
- •Sedatives, Hypnotics
- •Benzodiazepines
- •Pharmacokinetics of Benzodiazepines
- •Therapy of Depressive Illness
- •Mania
- •Therapy of Schizophrenia
- •Psychotomimetics (Psychedelics, Hallucinogens)
- •Hypothalamic and Hypophyseal Hormones
- •Thyroid Hormone Therapy
- •Glucocorticoid Therapy
- •Follicular Growth and Ovulation, Estrogen and Progestin Production
- •Oral Contraceptives
- •Antiestrogen and Antiprogestin Active Principles
- •Aromatase Inhibitors
- •Insulin Formulations
- •Treatment of Insulin-dependent Diabetes Mellitus
- •Treatment of Maturity-Onset (Type II) Diabetes Mellitus
- •Oral Antidiabetics
- •Drugs for Maintaining Calcium Homeostasis
- •Drugs for Treating Bacterial Infections
- •Inhibitors of Cell Wall Synthesis
- •Inhibitors of Tetrahydrofolate Synthesis
- •Inhibitors of DNA Function
- •Inhibitors of Protein Synthesis
- •Drugs for Treating Mycobacterial Infections
- •Drugs Used in the Treatment of Fungal Infections
- •Chemotherapy of Viral Infections
- •Drugs for the Treatment of AIDS
- •Drugs for Treating Endoparasitic and Ectoparasitic Infestations
- •Antimalarials
- •Other Tropical Diseases
- •Chemotherapy of Malignant Tumors
- •Targeting of Antineoplastic Drug Action (A)
- •Mechanisms of Resistance to Cytostatics (B)
- •Inhibition of Immune Responses
- •Antidotes and Treatment of Poisonings
- •Therapy of Selected Diseases
- •Hypertension
- •Angina Pectoris
- •Antianginal Drugs
- •Acute Coronary Syndrome— Myocardial Infarction
- •Congestive Heart Failure
- •Hypotension
- •Gout
- •Obesity—Sequelae and Therapeutic Approaches
- •Osteoporosis
- •Rheumatoid Arthritis
- •Migraine
- •Common Cold
- •Atopy and Antiallergic Therapy
- •Bronchial Asthma
- •Emesis
- •Alcohol Abuse
- •Local Treatment of Glaucoma
- •Further Reading
- •Further Reading
- •Picture Credits
- •Drug Indexes

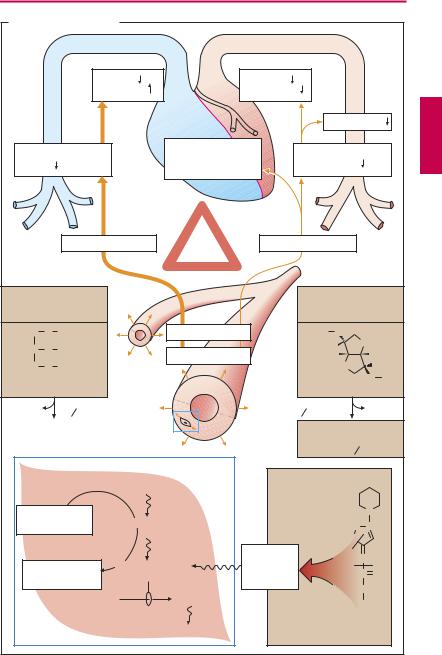
124 Vasodilators
Organic Nitrates
Various esters of nitric acid (HNO3) and polyvalent alcohols relax vascular smooth muscle, e.g., nitroglycerin (glyceryl trinitrate) and isosorbide dinitrate. The effect is more pronounced in venous than in arterial beds.
These vasodilator effects produce hemodynamic consequences that can be put to therapeutic use. Owing to a decrease in both venous return (preload) and arterial afterload, cardiac work is decreased (p.318). As a result, the cardiac oxygen balance improves. Spasmodic constriction of larger coronary vessels (coronary spasm) is prevented.
Uses. Organic nitrates are used chiefly in angina pectoris (p.316), less frequently in severe forms of chronic and acute congestive heart failure. Continuous intake of higher doses with maintenance of steady plasma levels leads to loss of ef cacy, inasmuch as the organism becomes refractory (tachyphylactic). This “nitrate tolerance” can be avoided if a daily “nitrate-free interval” is maintained, e.g., overnight.
At the start of therapy, unwanted reactions occur frequentlyin the formofathrobbing headache, probably caused by dilation of cephalic vessels. This effect also exhibits tolerance, even when daily “nitrate pauses” are observed. Excessive dosages give rise to hypotension, reflex tachycardia, and circulatory collapse.
Mechanism of action. The reduction in vascular smooth muscle tone is due to activation of guanylate cyclase and elevation of cyclic GMP levels. The causative agent is nitric oxide (NO) generated from the organic nitrate. NO is a physiological messenger molecule that endothelial cells release onto subjacent smooth muscle cells (“endothe- lium-derived relaxant factor,” EDRF). Organic nitrates thus utilize a physiological pathway; hence their high ef cacy. The enzymatically mediated generation of NO from
organic nitrates (via a mitochondrial aldehyde dehydrogenase) within the smooth muscle cell depends on a supply of free sulfhydryl (–SH) groups; “nitrate-tolerance” is attributed to a cellular exhaustion of SH donors.
Nitroglycerin (NTG) is distinguished by a high membrane penetrability and very low stability. It is the drug of choice in the treatment of angina pectoris attacks. For this purpose, it is administered as a spray, or in sublingual or buccal tablets for transmucosal delivery. The onset of action is between 1 and 3 minutes. Due to a nearly complete presystemic elimination, it is poorly suited for oral administration. Transdermal delivery (nitroglycerin patch) also avoids presystemic elimination.
Isosorbide dinitrate (ISDN) penetrates wellthroughmembranes,ismorestablethan NTG, and is partly degraded into the weaker, but much longer acting, 5-isosorbide mononitrate (ISMN). ISDN can also be applied sublingually; however, it is mainly administered orally in order to achieve a prolonged effect. ISMN is not suitable for sublingual use because of its higher polarityandslower rate of absorption. Taken orally, it isabsorbed and is not subject to first-pass elimination.
Molsidomine itself is inactive. After oral intake, it is slowly converted into an active metabolite, linsidomine. The differential effectiveness in arterial vs. venous beds is less evident compared to the drugs mentioned above. Moreover, development of “nitrate tolerance” is of less concern. These differencesinactivityprofileappeartoreflectadifferent mechanism of NO release. The same applies to the following sodium nitroprusside.
Sodium nitroprusside contains a nitroso (–NO) group, but is not an ester. It dilates venousand arterial beds equally. It is administered by infusion to achieve controlled hypotension under continuous close monitoring. Cyanide ions liberated from nitroprusside can be inactivated with sodium thiosulfate (p.310).
|
|
|
|
|
|
|
Organic Nitrates |
|
|
|
125 |
||
A. Vasodilators: Nitrates |
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
Preload |
|
Afterload |
|
|
|
|
|
|
|
|
|
|
|
O2-supply |
|
O2-demand |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Blood pressure |
||||
Venous blood return |
|
Prevention of |
|
|
Peripheral |
|
|
||||||
|
coronary artery |
|
|
|
|
||||||||
to heart |
|
|
|
|
|
|
resistance |
|
|
||||
|
|
|
|
spasm |
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Venous bed |
“Nitrate |
Arterial bed |
|
|
|
|
|||
|
|
|
|
|
|
tolerance” |
|
|
|
|
|
|
|
Route: |
|
|
|
|
|
|
|
Route: |
|
|
|
|
|
e.g., sublingual, |
|
|
|
|
e.g., sublingual, |
||||||||
transdermal |
|
|
|
|
|
oral, transdermal |
|||||||
H2C |
O |
NO2 |
|
|
|
Vasodilation |
|
|
O2N O |
|
|
O |
|
HC |
O |
NO2 |
|
|
|
|
|
|
H |
5 |
|
||
|
|
|
“Nitrates” |
|
|
|
|
|
H |
||||
|
|
|
|
|
|
|
|
H |
4 |
3 |
|
||
H2C O NO2 |
|
|
|
|
|
|
O 1 |
2 |
H |
||||
Glyceryl trinitrate |
|
|
|
|
|
|
|
|
O NO2 |
||||
Nitroglycerin |
|
|
|
|
|
Isosorbide dinitrate |
|||||||
NO |
|
t 1 |
2 |
~ 2 min |
|
|
t 1 |
2 |
~ 30 min |
|
|
|
NO |
|
|
|
|
|
|
|
|
|
|
|
|
||
Inactivation |
|
|
|
5-Isosorbide mono- |
|||||||||
|
|
|
|
|
|
|
nitrate, an active meta- |
||||||
|
|
|
|
|
|
|
bolite |
t 1 2 ~ 240 min |
|||||
|
|
|
|
|
R – O – NO2 |
|
|
|
|
|
|
|
|
SH-donators |
|
|
Release of NO |
|
|
|
|
|
|
N |
|||
e.g., glutathione |
|
|
|
–N |
|
N+ |
|||||||
|
|
|
|
|
|
|
|
|
|
O |
|
|
|
|
|
|
|
|
|
|
Active |
|
|
2 |
|
N |
|
Consumption |
Activation of |
|
|
|
1 |
|
|
||||||
|
metabolite |
|
|
|
C |
O |
|||||||
guanylate cyclase |
|
|
|
|
|||||||||
of SH donors |
|
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
|
|
|
O |
|
|
|
|
|
GTP |
|
cGMP |
|
|
|
|
|
C2H5 |
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
Smooth mucle cell |
|
Relaxation |
|
|
Molsidomine |
|
||||||
|
|
|
|
(precursor) |
|
|
|
||||||

126 Vasodilators
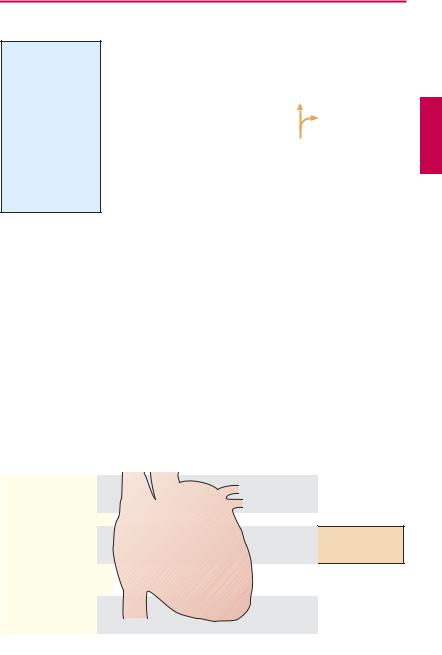
Calcium Antagonists
During electrical excitation of the cell membrane of heart or smooth muscle, different ionic currents are activated, including an inward Ca2+ current. The term Ca2+ antagonist is applied to drugs that inhibit the influx of Ca2+ ions without affecting inward Na+ or outward K+ currents to a significant degree. Other labels are calcium entry blocker or
Ca2+-channel blocker. Ca2+ antagonists used therapeutically can be divided into three groups according to their effects on heart and vasculature.
I. Dihydropyridine Derivatives
The dihydropyridines, e.g., nifedipine, are uncharged hydrophobic substances. They particularly induce a relaxation of vascular smooth muscle in arterial beds. An effect on cardiac function is practically absent at therapeutic dosage. (In pharmacological experiments on isolated cardiac muscle preparations, a clear negative inotropic effect is, however, demonstrable at high concentrations.) They are thus regarded as vasoselective Ca2+ antagonists. Because of the dilation of resistance vessels, blood pressure falls. Cardiac afterload is diminished (p.318) and, therefore, also oxygen demand. Spasms of coronary arteries are prevented.
Indications. An indication for nifedipine is angina pectoris (p.318). In angina pectoris, it is effective when given either prophylactically or during acute attacks. Adverse effects are palpitation (reflex tachycardia due to hypotension), headache, and pretibial edema.
The successor substances principally exert the same effects, but have different kinetic properties (slow elimination and, hence, steady plasma levels).
Nitrendipine, isradipine, and felodipine are used in the treatment of hypertension. Nicardipine and nisoldipine are also used in angina pectoris. Nimodipine is given prophylactically after subarachnoidal hemorrhage to prevent vasospasms. On its dihydropyri-
dine ring, amlodipine possesses a side chain with a protonatable nitrogen and can therefore exist in a positively charged state. This influences its pharmacokinetics, as evidenced by the very long half-life of elimination (~ 40 hours).
II. Verapamil and Other Catamphiphilic Ca2+ Antagonists
Verapamil contains a nitrogen atom bearing a positive charge at physiological pH and thus represents a cationic amphiphilic molecule. It exerts inhibitory effects not only on arterial smooth muscle, but also on heart muscle. In the heart, Ca2+ inward currents are important in generating depolarization of sinoatrial node cells (impulse generation), in impulse propagation through the AVjunction (atrioventricular conduction), and in electromechanical coupling in the ventricular cardiomyocytes. Verapamil thus produces negative chronotropic, dromotropic, and inotropic effects.
Indications. Verapamil is used as an antiarrhythmic drug in supraventricular tachyarrhythmias. In atrial flutter or fibrillation, it is effective in reducing ventricular rate by virtue of inhibiting AV conduction. Verapamil is also employed in the prophylaxis of angina pectoris attacks (p.318) and the treatment of hypertension (p.314).
Adverse effects. Because of verapamil’s effects on the sinus node, a drop in blood pressure fails to evoke a reflex tachycardia. Heart rate hardly changes; bradycardia may even develop. AV-block and myocardial insuf ciency can occur. Patients frequently complain of constipation, because verapamil also inhibits intestinal musculature.
Gallopamil (= methoxyverapamil) is closely related to verapamil in terms of both structure and biological activity.
Diltiazem is a catamphiphilic benzothiazepine derivative with an activity profile resembling that of verapamil.
|
|
|
|
|
|
Calcium Antagonists |
127 |
||
A. Vasodilators: calcium antagonists |
|
|
|
|
|
||||
Smooth muscle cell |
|
|
|
|
|
|
|
||
|
|
|
|
|
|
Afterload |
|
|
|
|
|
|
|
|
|
O2-demand |
|
|
|
|
|
|
|
|
|
|
Blood pressure |
||
Contraction |
|
|
|
|
|
|
|
||
|
|
|
|
Inhibition of |
|
Peripheral |
|
||
|
|
|
|
|
resistance |
|
|||
|
|
|
|
coronary spasm |
|
||||
|
|
|
|
|
|
|
|||
Ca2+ |
|
|
|
|
|
|
|
|
|
|
|
|
|
Arterial |
|
|
|
|
|
|
|
|
|
blood vessel |
|
|
|
|
|
|
|
|
Vasodilation in arterial bed |
|
|
|
|||
|
|
|
|
Na+ Ca2+10-3M |
|
|
|
|
|
|
|
|
depolarization |
|
|
O |
CH3 |
|
|
|
|
|
|
|
H3CO |
O |
CH3 |
|
|
|
|
NO2 |
|
|
H3C |
|
O |
CH3 |
|
H3C O C H |
|
|
|
|
|
O CH3 |
|||
|
C O CH3 |
Ca2+10-7M |
K+ |
HC C C N |
|
||||
O |
|
O |
H3C H2C |
|
|
|
|||
H3C |
N |
CH3 |
Membrane |
|
|
H2C |
|
CH2 |
|
|
H |
|
Selective |
|
H2C + |
C |
|
||
|
|
|
inhibition of |
|
|
N |
H2 |
|
|
|
|
|
|
|
H3C |
H |
|
||
|
|
|
calcium influx |
|
|
||||
|
|
|
|
|
|
|
|||
Nifedipine |
|
|
|
|
|
Verapamil |
|
|
|
(dihydropyridine derivative) |
|
|
|
(cationic-amphiphilic) |
|||||
|
|
|
Inhibition of cardiac functions |
|
|
|
|||
|
|
|
|
|
|
Impulse |
Heart rate |
|
|
|
|
|
Sinus node |
|
generation |
Reflex tachycardia |
|||
|
|
|
|
|
|
|
with nifedipine |
||
Ca2+ |
|
|
|
|
|
|
|
|
|
|
|
Ca2+ |
|
|
|
Impulse |
AV- |
|
|
|
|
AV-node |
|
|
conduction |
conduction |
|
||
|
|
|
|
|
|
||||
|
|
Ca2+ |
|
|
|
|
|
|
|
Ca2+ |
|
|
|
|
|
|
|
|
|
|
|
|
|
Ventricular |
Electro- |
Contractility |
|||
|
|
|
|
mechanical |
|||||
|
|
|
|
muscle |
|
||||
|
|
|
|
|
coupling |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Heart muscle cell |
|
|
|
|
|
|
|
||
