
- •VOLUME 3
- •CONTRIBUTOR LIST
- •PREFACE
- •LIST OF ARTICLES
- •ABBREVIATIONS AND ACRONYMS
- •CONVERSION FACTORS AND UNIT SYMBOLS
- •EDUCATION, COMPUTERS IN.
- •ELECTROANALGESIA, SYSTEMIC
- •ELECTROCARDIOGRAPHY, COMPUTERS IN
- •ELECTROCONVULSIVE THERAPHY
- •ELECTRODES.
- •ELECTROENCEPHALOGRAPHY
- •ELECTROGASTROGRAM
- •ELECTROMAGNETIC FLOWMETER.
- •ELECTROMYOGRAPHY
- •ELECTRON MICROSCOPY.
- •ELECTRONEUROGRAPHY
- •ELECTROPHORESIS
- •ELECTROPHYSIOLOGY
- •ELECTRORETINOGRAPHY
- •ELECTROSHOCK THERAPY.
- •ELECTROSTIMULATION OF SPINAL CORD.
- •ELECTROSURGICAL UNIT (ESU)
- •EMERGENCY MEDICAL CARE.
- •ENDOSCOPES
- •ENGINEERED TISSUE
- •ENVIRONMENTAL CONTROL
- •EQUIPMENT ACQUISITION
- •EQUIPMENT MAINTENANCE, BIOMEDICAL
- •ERGONOMICS.
- •ESOPHAGEAL MANOMETRY
- •EVENT-RELATED POTENTIALS.
- •EVOKED POTENTIALS
- •EXERCISE FITNESS, BIOMECHANICS OF.
- •EXERCISE, THERAPEUTIC.
- •EXERCISE STRESS TESTING
- •EYE MOVEMENT, MEASUREMENT TECHNIQUES FOR
- •FETAL MONITORING
- •FETAL SURGERY.
- •FEVER THERAPY.
- •FIBER OPTICS IN MEDICINE
- •FICK TECHNIQUE.
- •FITNESS TECHNOLOGY.
- •FIXATION OF ORTHOPEDIC PROSTHESES.
- •FLAME ATOMIC EMISSON SPECTROMETRY AND ATOMIC ABSORPTION SPECTROMETRY
- •FLAME PHOTOMETRY.
- •FLOWMETERS
- •FLOWMETERS, RESPIRATORY.
- •FLUORESCENCE MEASUREMENTS
- •FLUORESCENCE MICROSCOPY.
- •FLUORESCENCE SPECTROSCOPY.
- •FLUORIMETRY.
- •FRACTURE, ELECTRICAL TREATMENT OF.
- •FUNCTIONAL ELECTRICAL STIMULATION
- •GAMMA CAMERA.
- •GAMMA KNIFE
- •GAS AND VACUUM SYSTEMS, CENTRALLY PIPED MEDICAL
- •GAS EXCHANGE.
- •GASTROINTESTINAL HEMORRHAGE
- •GEL FILTRATION CHROMATOGRAPHY.
- •GLUCOSE SENSORS
- •HBO THERAPY.
- •HEARING IMPAIRMENT.
- •HEART RATE, FETAL, MONITORING OF.
- •HEART VALVE PROSTHESES
- •HEART VALVE PROSTHESES, IN VITRO FLOW DYNAMICS OF
- •HEART VALVES, PROSTHETIC
- •HEART VIBRATION.
- •HEART, ARTIFICIAL
- •HEART–LUNG MACHINES
- •HEAT AND COLD, THERAPEUTIC
- •HEAVY ION RADIOTHERAPY.
- •HEMODYNAMICS
- •HEMODYNAMIC MONITORING.
- •HIGH FREQUENCY VENTILATION
- •HIP JOINTS, ARTIFICIAL
- •HIP REPLACEMENT, TOTAL.
- •HOLTER MONITORING.
- •HOME HEALTH CARE DEVICES
- •HOSPITAL SAFETY PROGRAM.
- •HUMAN FACTORS IN MEDICAL DEVICES
- •HUMAN SPINE, BIOMECHANICS OF
ECG Storage
XML File Format
150 ECGs to internal flash memory
2–3 ECGs typical per 1.4 MB floppy disk
150 ECGs per 128 MB PCMCIA card (optional)
ECG File Formats
XML and XML SVG
Power and Environment
Line Power 100–240 Vac, 50/60 Hz, 150 VA max
Environmental Operating Conditions
15–35 8C (50–104 8F)
15–70% relative humidity (noncondensing) Up to 4550 m (15,000 ft.) altitude
Environmental Storage Conditions
0–408C (32–122 8F)
15–80% relative humidity (noncondensing) Up to 4550 m (15,000 ft) altitude
Cardiograph Dimensions
45 45.8 16 cm (17.7 18.0 6.34 in.)
Cardiograph Weight
13 kg (28 lb.) including accessories
Patient Interface Module
Remote, microprocessor-controlled module
Safety and Performance
Meets the following requirements for safety and performance:
IEC 60601-1:1988 þ A1: 1991 þ A2: 1995 General Requirements for Safety including all National Deviations
IEC 60601-1-2: 1993 General Requirements for Safety Electromagnetic Compatibility
IEC 60601-2-25: 1993 þ A1: 1999 Safety of Electrocardiographs
IEC 55011: 1998 Radio Frequency disturbance, Limits and Methods of Test
AAMI EC11: 1991 Diagnostic Electrocardiographic Devices
JIST 1202: 1998 Japanese Industrial Standard for Electrocardiographs
ACKNOWLEDGMENT
The excellent support of Ms Mary-Lou Lufkin with the Diagnostic ECG Division at Philips Medical Systems, USA is greatly appreciated.
ELECTROCONVULSIVE THERAPHY |
53 |
BIBLIOGRAPHY
Cited References
1.Clark JW. The origin of biopotentials. In: Webster JG, editor. Medical Instrumentation. 3rd ed. New York: John Wiley & Sons; 1998, p 121–182.
2.Malmivuo J, Plonsey R. Bioelectromagnetism: Principles and Applications of Bioelectric and Biomagnetic Fields. New York: Oxford University Press; 1995.
3.Netter FH. The Heart, Vol. 5. The Ciba Collection of Medical Illustrations. Ciba Pharmaceutical Company; 1971.
4.Haykin S. Adaptive Filter Theory. 4th ed. New York: Prentice Hall; 2001.
5.Anonymous. American National Standard for Diagnostic Electrocardiographic Devices. ANSI/AAMI EC 13, New York: American National Standards Institute; 1983.
6.Webster JG, editor. Bioinstrumentation. New York: Wiley; 2004.
7.Available at http://medstat.med.utah.edu/kw/ecg/ACC_AHA. html.
8.Macfarlane PW, Lawrie TDV, editors. Comprehensive Electrocardiology: Theory and Practice in Health and Disease. 1st ed. Vols. 1–3. New York: Pergamon Press; 1989. 1785 p.
9.Available at http://www.sci.utah.edu.
10.Available at http://butler.cc.tut.fi/ malmivuo/bem/index.htm.
11.Available at http://rudylab.wustl.edu.
12.Available at http://www.bioeng.auckland.ac.nz/projects/ei/ eimaging.php.
13.Chatlapalli S, et al. Accurate Derivation of Heart Rate Variability Signal for Detection of Sleep Disordered Breathing in Children. Proc 26th Annu Int Conf IEEE EMBS San Francisco, (CA) Sept., 2004.
14.Benitez D, Gaydecki PA, Zaidi A, Fitzpatric AP. The use of Hilbert Transform in ECG signal analysis. Comput Biol Med Sept.2001;31(5):399–406.
15.Mendoza P, et al. A Web-based Vital Sign Telemonitor and Recorder for Telemedicine Applications. Proc IEEE/EMBS, 26th Annu Int Conf, San Francisco (CA). Sept. 1–4, 2004.
See also ARRHYTHMIA ANALYSIS, AUTOMATED; GRAPHIC RECORDERS; PHONOCARDIOGRAPHY.
ELECTROCONVULSIVE THERAPHY
MILTON J. FOUST, JR
MARK S. GEORGE
Medical University of South
Carolina
Charleston, South Carolina
INTRODUCTION
Electroconvulsive therapy (ECT) is a technique for the treatment of severe psychiatric disorders, which consists of the deliberate induction of a generalized tonic-clonic seizure by electrical means. Contemporary ECT devices typically deliver bidirectional (alternating current) briefpulse square-wave stimulation through a pair of electrodes that are applied externally to the patient’s scalp. The procedure is now almost always performed under general anesthesia, although, in some unusual situations, such as in developing countries with limited medical resources, it
54 ELECTROCONVULSIVE THERAPHY
may be occasionally done without anesthesia (1). As with other convulsive therapies that historically preceded ECT, the goal is to produce a seizure. The presence of seizure activity appears to be essential; stimuli that are below the seizure threshold appear to be clinically ineffective. However, although the production of a seizure appears to be necessary, a seizure alone is not sufficient. Some forms of seizure induction are, in fact, clinically ineffective. A variety of psychiatric and neurological conditions exist that respond favorably to ECT, although the majority of patients treated with ECT have mood disorders, such as unipolar or bipolar depression, particularly when severe or accompanied by psychotic symptoms. Certain other conditions, such as mania, schizoaffective disorder, catatonia, neuroleptic malignant syndrome, Parkinson’s disease, and intractable seizures, may respond to ECT as well. Schizophrenia has also been treated with ECT, although the results tend to be less favorable than those obtained in patients with mood disorders. Those patients with schizophrenia who also have a prominent disturbance of mood probably respond best to ECT (2,3). Typically, a series or a course of treatments is prescribed. By convention, ECT treatments are usually given two to three times per week. A course usually consists of around six to eight treatments, which may then be followed by maintenance treatment in the form of either medication, additional ECT given at less frequent intervals, or both. A number of questions still remain regarding the most effective methods for performing ECT, the mechanism of action of ECT, and what role there may be in the future for ECT and other forms of brain stimulation, such as repeated transcranial magnetic stimulation (rTMS), magnetic seizure therapy (MST), and vagus nerve stimulation (VNS).
HISTORY
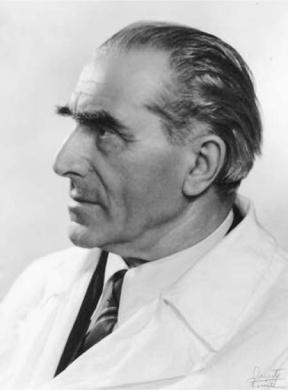
ECT was first used by the Italian psychiatrists Ugo Cerletti (Fig. 1) and Lucio Bini to treat a disorganized, psychotic man found wandering the streets of Rome in 1938. The results were dramatic, with complete recovery reported (4). The treatment was developed as an alternative to other, higher risk forms of artificial seizure induction, specifically Ladislas von Meduna’s convulsive therapy involving the use of stimulants such as camphor, strychnine, and Metrazol (pentylenetetrazol) (4–6). ECT was welcomed due to its effectiveness with otherwise treatment-resistant and profoundly disabled patients. However, the procedure was at risk of being abandoned due to the incidence of fractures (up to 40%) caused by uncontrolled seizure activity. This problem was resolved by the introduction of muscle relaxation (originally in the form of curare, and later with depolarizing muscle relaxants such as succinylcholine) and general anesthesia (7). The use of anesthesia and muscle relaxation was one of the most important innovations in ECT treatment, another being the use of brief-pulse square-wave stimulation in place of sine-wave alternating current. Brief-pulse ECT was found to cause less cognitive impairment compared with sine-wave ECT, as well as less disruption of the EEG (8,9). The routine use of oxygen and monitoring of vital signs, cardiac rhythm, pulse oximetry,
Figure 1. Ugo Cerletti 1877–1963. Reprinted with permission from the American Journal of Psychiatry, (Copyright 1999). American Psychiatric Association.
electromyography (EMG), and electroencephalography (EEG) have also helped to reduce the risks associated with the procedure.
PRE-ECT EVALUATION
In order to receive ECT, a patient must first be evaluated by a physician (typically a psychiatrist) who is trained and credentialed in the procedure and who agrees that the patient is a suitable candidate, based on psychiatric history and examination, physical condition, and capacity to consent. If a patient is unable to consent, a suitable substitute decision-maker must be identified, usually a family member (in some states, a court-order may be required). The process of evaluation typically consists, at a minimum, of a psychiatric interview and mental status examination, a medical history (including a past medical history, family and social history, and review of systems) and physical examination (including a screening neurological examination and fundoscopic examination to exclude papilledema) (1,2,10). It is necessary to review the patient’s current medications, including those that are prescribed for concurrent medical conditions as well as psychiatric medications, and to obtain some information about previous medication trials for the psychiatric condition under consideration. Usually, it is desirable to obtain some basic laboratory studies (such as complete blood count, serum electrolytes, BUN, glucose and creatinine, urinalysis, liver

function tests, and thyroid function tests) both to screen for medical conditions that may cause depressive or psychotic symptoms and to identify conditions of increased ECT or anesthesia risk. Most patients, and especially older patients or patients with a history of cardiovascular disease, should have an electrocardiogram (ECG). The use of brain imaging is controversial; many practitioners prefer some form of pre-ECT brain imaging to identify or exclude the possibility of an intracranial mass, one of the few conditions that may be associated with a high risk of mortality with ECT (11). However, it has been argued that a neurologic examination should be sufficient to screen for this particular risk factor (12).
CONSENT
Prior to undergoing ECT or any other procedure, the patient (or patient’s surrogate decision-maker) must demonstrate a satisfactory understanding of the nature of the procedure, its risks, benefits, and alternatives. In some states, the physician may need to petition the court for permission to perform ECT on patients who lack the capacity to consent. The issue of consent is complex, as those patients who are most in need of ECT are generally those who are the most ill, and are often the most vulnerable and impaired. It is possible to have a severe psychiatric illness and yet still retain the capacity to rationally evaluate the necessary issues involved in making a decision as to whether to have ECT, but one can be seriously incapacitated as well. Evaluating the patient’s capacity to give informed consent is one of the most important parts of the pre-ECT consultation process, along with establishing the presence or absence of an appropriate indication for treatment and identifying concurrent medical conditions and medications that may increase the risk of treatment. It is part of the consultant’s responsibility to educate the patient about what is, for many, an unfamiliar or frightening treatment. Often, much of what a patient or family may understand of ECT consists of disturbing images, such as those presented in films like ‘‘One Flew over the Cuckoo’s Nest’’ (13). In most cases, the patient will be able to understand the information presented and engage in a rational decision-making process despite their illness. However, some patients may be able to express a superficial understanding of the facts at hand and yet be impaired in the ability to make rational decisions (14), which may be demonstrated through self-destructive behavior, lack of self-care, or irrational refusal of necessary treatment. In these cases, it becomes necessary to seek a substitute, usually a family member, who can make medical decisions on the patient’s behalf. State laws differ regarding the details and circumstances under which another person can make these types of treatment decisions, and it is necessary to become familiar with the particular local laws governing consent.
INDICATIONS
The most common indication for ECT is severe, treatmentresistant depression, either of the unipolar or bipolar type
ELECTROCONVULSIVE THERAPHY |
55 |
Table 1. Indications for ECT
Unipolar or bipolar depression
Mania
Schizoaffective disorder
Schizophreniform disorder
Schizophrenia
Catatonia
Neuroleptic malignant syndrome
(Table 1). The syndrome of depression is characterized by a sad or depressed mood, as well as disturbances in energy level, sleep, and the capacity to experience pleasure (anhedonia) (15). It may include psychotic symptoms such as delusions (fixed, false beliefs that are held despite evidence to the contrary) or hallucinations. Patients with so-called ‘‘unipolar’’ depression exhibit one or more episodes of depression without episodes of mania. Such patients will usually be formally diagnosed as having a major depressive disorder (MDD). Patients with so-called ‘‘bipolar’’ depression have also suffered from one or more episodes of mania, frequently in a cyclical pattern of alternating mania followed by depression. Those patients who are most severely ill, particularly those who are delusional or catatonic, will typically respond best to ECT. Although usually reserved for those patients who have not had a successful response to one or more medication trials, ECT is an appropriate first treatment when the patient’s life is threatened by severe illness in the form of aggressively self-destructive behavior, refusal or inability to eat or drink, or extreme agitation. Mania, a condition characterized by an abnormally elevated or irritable mood, hyperactivity, agitation, impulsivity, and grandiosity, also responds well to ECT. Schizophrenia is often treated with ECT, particularly in some European and Asian countries, but may respond less well, unless mood disturbance is a prominent component of the patient’s illness. Neuroleptic malignant syndrome (an antipsychotic drug-induced syndrome that shares many of the characteristics of catatonia) is a less common indication for ECT and may be used when the syndrome persists despite the usual interventions such as discontinuing neuroleptics and treatment with dopamine agonists. Catatonia (which may be an expression of either a mood disorder or schizophrenia) is characterized by mutism and immobility, sometimes with alternating periods of agitation. These patients may respond to treatment with benzodiazepines, but if they do not, ECT is indicated and frequently effective. Recurrent, treatmentrefractory seizures may respond to ECT as well, suggesting an anticonvulsant mechanism of action for ECT (16). Patients with Parkinson’s disease may improve with ECT, possibly due to the dopaminergic effect of ECT.
Certain conditions exist, such as personality disorders, that do not respond well to ECT or may even reduce the likelihood of successful treatment when they coexist with a more suitable indication, such as a mood disorder (17–19). In some cases, the burden of disability and suffering may be so great (and the risk of serious complications so low) that ECT may reasonably be offered even if the patient’s diagnosis is not one of those generally considered a standard indication for the treatment (20).
56 ELECTROCONVULSIVE THERAPHY
Table 2. Conditions of Increased Risk with ECT
Increased intra-cranial pressure
Recent myocardial infraction or stroke
Unstable angina
Severe cardiac valvular disease
Severe congestive heart failure
Unstable aneurysms
Severe pulmonary disease
Pheochromocytoma
Retinal detachment
Glaucoma
CONDITIONS OF INCREASED RISK
As will be discussed later in this article, ECT as currently practiced is a relatively low risk procedure. It can be safely used to treat all patient groups including children and adolescents (21–25), pregnant women (26,27), and the elderly (28). In particular, age alone should not be considered a barrier to treatment; elderly patients are among those who often have the most dramatic and favorable responses to ECT (29). However, certain medical conditions exist that may, to a greater or lesser degree, contribute to an increase in risk of morbidity or mortality with the procedure (Table 2). Most significant among these would be severe or unstable cardiac disease or the presence of a space-occupying lesion (such as a tumor) within the cranial cavity, resulting in increased intracranial pressure. Very small tumors without a visible mass effect on computerized tomography (CT) or magnetic resonance imaging (MRI) do not appear to pose a high risk with ECT (30). Detecting such masses and making the distinction between low and high risk lesions may help to support a rationale for pre-ECT brain imaging as a screening tool (11).
COMPLICATIONS
Serious complications with ECT are rare (Table 3). The risk of death has been estimated at 4 per 100,000 treatments (31). The risk of other potentially life-threatening complications, such as myocardial infraction and stroke, is also very low, although the risk of cardiac arrhythmias appears to be higher in persons with pre-existing cardiac disease (32,33). The introduction of general anesthesia and muscle relaxation has almost eliminated the risk of fractures with ECT. Both retrograde amnesia and anterograde amnesia are common, but it is unusual for cognitive impairment to be severe or prolonged. Minor side effects such as headaches, muscle aches, and nausea frequently occur; these side effects are usually transient and easily managed with symptomatic treatment.
The amnesia or memory loss that occurs with ECT typically takes two forms: loss of memory for past or previously learned information (retrograde amnesia) as well as difficulty in learning new information (anterograde amnesia). The retrograde amnesia associated with ECT tends to be greater for ‘‘public’’ or ‘‘impersonal’’ knowledge about the world than for autobiographical or personal memories. Memories for remote events also tend to be
Table 3. Side Effects and Complications with ECT
Common:
Cognitive side effects
Transient postictal confusion or delirium Retrograde and anterograde amnesia
Headaches Muscle soreness Nausea
Less common or rare: Death (1/10,000 patients) Aspiration
Brochospasm or laryngospasm Cardiovascular
Arrhythmias
Severe hypertension or hypotension Cardiac ischemia
Myocardial infarction Cardiac arrest
Neurological
Prolonged or tardive seizures Nonconvulsive status epilepticus Stroke
Prolonged apnea due to pseudocholinesterase deficiency Malignant hyperthermia of anesthesia
better preserved than that for more recent events. Bilateral ECT appears to produce greater and more persistent memory deficits than right-unilateral ECT (34). ECT-induced anterograde amnesia is typically greatest immediately following treatment and tends to rapidly resolve in the weeks following the last treatment of a series. Recovery also typically occurs over time with retrograde amnesia, although patients may notice some persistent gaps in memory for past events. Although anecdotal, it may be reassuring to patients to be made aware of the stories of psychologists and physicians who have had ECT, benefited, and resumed their professional activities (35). Uncommon exceptions to these rules exist, however. A few patients complain of severe and persistent problems with memory that cause them much distress (36). No satisfactory explanation exists for this phenomenon of severe ECT-induced memory loss (37). No reliable evidence exists that ECT causes damage or injury to the nervous system.
MEDICATIONS AND ECT
Experts in the past have recommended stopping antidepressants prior to ECT (38), although a recent study now suggests that tricyclic antidepressants (TCAs) and selective serotonin reuptake inhibitors (SSRIs) may be safe in combination with ECT (39). Evidence exists that certain antipsychotic medications (such as haloperidol, risperidone, and clozapine) may have beneficial effects in combination with ECT (40–44). Many drugs that were originally developed and used as anticonvulsants (such as carbamazepine, valproic acid, and lamotrigine) are frequently used as either mood stabilizers or as adjunctive agents in antidepressant regimens. As these drugs, by definition, can be expected to inhibit seizure activity, they are generally tapered and discontinued prior to beginning
ECT. An exception would be those patients for whom these drugs are prescribed for a concurrent seizure disorder. In these cases, anticonvulsant drugs should usually be continued in order to minimize the risk of uncontrolled seizure activity between treatments. Lithium, a commonly used mood stabilizer, has been associated with prolonged delirium following ECT. In general, it should be avoided, but, in special circumstances and with careful monitoring, its use in combination with ECT may be justified (45,46). Both chlorpromazine and reserpine, an antipsychotic and antihypertensive agent that acts through the depletion of neuronal dopamine, have been associated with severe hypotension and death when combined with ECT (47).
Certain drugs that are prescribed for concurrent medical conditions (and not primarily for psychiatric conditions) help to reduce the risks associated with ECT and anesthesia. Patients who have gastro-esophageal reflux disease (GERD) should be treated with a suitable medication (such as a histamine-2 receptor blocker or proton pump inhibitor) in the morning prior to ECT to reduce the risk of reflux and aspiration. Patients who may be especially prone to aspiration can be treated with intravenous metoclopramide to accelerate gastric emptying. Pregnant women may be given sodium citrate/citric acid solution by mouth. Patients with known hypertension should receive their usual antihypertensive regimen prior to ECT; an exception would be made for diuretics, which should be delayed until after ECT to avoid bladder filling before or during the procedure. Some patients may have an exaggerated hypertensive response to the outpouring of catecholamines that occurs with seizure response to ECT, which can usually be controlled with intravenous beta-adrenergic antagonists such as esmolol or labetalol. A patient with a pheochromocytoma (catecholaminesecreting tumor) is at especially high risk of severe hypertension (48). Such a patient may require more aggressive measures (such as arterial blood-pressure monitoring and intravenous sodium nitroprusside) in order to maintain satisfactory blood pressure control (49). Patients with pulmonary disease should have their pulmonary status assessed prior to treatment and should receive their usual medications, including inhaled beta-agonists or steroids. As ECT and the resulting seizure produces a transient increase in intraocular pressure (50), patients with retinal detachment may be at risk of further eye injury and should have this condition treated prior to ECT. Similarly, patients with glaucoma should have their intraocular pressures controlled with suitable medications prior to ECT (51).
ANESTHESIA
Methohexital was previously a very popular anesthetic drug for ECT, but manufacturing problems made it essentially unavailable for several years, forcing changes in ECT anesthesia practice (52). Anesthesia for ECT may be induced with an intravenous injection of other short-acting anesthetic agents such as propofol and etomidate. Etomidate may be substituted for methohexital or propofol in an effort to produce seizures of longer duration (53) or to
ELECTROCONVULSIVE THERAPHY |
57 |
stimulate seizures in those uncommon situations of no seizure activity despite maximum stimulus and bilateral electrode placement. Once anesthesia is induced (typically within seconds following the injection), a muscle relaxant is injected, typically succinylcholine, but a nondepolarizing muscle relaxant such as mivacurium may be used when there are coexisting medical conditions that increase the risk of exaggerated hyperkalemic response with succinylcholine, such as burns, renal failure, or neurologic disease, or if a history of malignant hyperthermia exists (54,55). The ECT stimulus may elicit a vagal (parasympathetic) response, which can lead to bradycadia, transient heart block, or even asystole, which has been explained as the result of forced expiration against a closed glottis during the stimulus, or it may be a direct effect of the stimulus on the central nervous system. Bradycardia and asystole have been observed in the postictal period as well (56). An anticholinergic compound such as glycopyrrolate or atropine may be injected proximate to the anesthetic to reduce the bradyarrhythmias that may occur with ECT (57). If the stimulus is successful in producing a seizure, it results in an outpouring of catecholamines and a sympathetic response with resulting tachycardia and hypertension as noted above, which is usually transient and without clinical significance, but in some patients, especially those with pre-existing hypertension or cardiovascular disease, it may be desirable to limit this response using an antihypertensive agent (54,55,58).
Patients are unable to breathe without assistance when anesthetized and fully relaxed; ventilation and oxygenation are provided by means of positive-pressure ventilation with 100% oxygen through a bag and mask. Endotracheal intubation is rarely required. In some patients (such as pregnant women), the risk of reflux may be higher and intubation may be the preferred option for airway management (27). Some patients may have abnormalities of the face and upper airway that interfere with mask ventilation. Other options for airway management including intubation, laryngeal mask airway (59,60), or even tracheostomy may be considered.
MONITORING
The type of medical monitoring that is used during ECT includes ECG blood pressure, pulse oximetry, EMG, and EEG. Modern ECT devices typically include the capacity to monitor and record ECG, EMG, and EEG; commonly, a paired right and left fronto-mastoid EEG placement is used. Two-channel EEG monitoring is helpful both to ensure that the seizure generalizes to both hemispheres and to evaluate the degree of inter-hemispheric EEG symmetry or coherence, as well as postictal EEG suppression, all factors that may predict the therapeutic efficacy of the seizure (61). Two EMG electrodes are placed on a foot, usually the right, which is isolated from the rest of the patient’s circulation with a blood pressure cuff acting as a tourniquet, which minimizes the effect of the muscle relaxant and permits the observation and recording of motor seizure activity in the foot, even with complete paralysis otherwise.

58ELECTROCONVULSIVE THERAPHY
0.5ms
+
Current
-
Time
Figure 2. Brief-pulse square-wave ECT stimulus.
ECT STIMULUS
As noted previously, the ECT stimulus itself typically consists of a series of brief electrical pulses. Early ECT devices provided stimulation with sine-wave alternating current; essentially the same type of current that is distributed through public utilities for use in household appliances and lighting. Most modern ECT devices now provide a stimulus that consists of brief pulses with a bidirectional square-wave pattern (Fig. 2). (One exception is the Ectron series 5A, manufactured by Ectron, Ltd, Letchworth, Hertfordshire, England. This device delivers unidirectional pulses.) The American Psychiatric Association has recommended the use of ‘‘constant-current’’ devices; so-called because a relatively constant (rather than continuously varying) current is maintained for the duration of the pulse. The advantage of using a constant-current rather than constant-voltage or constant-energy device is that the clinician is able to deliver a predetermined quantity of charge by varying the time interval of exposure to the current (62).
At 100% of available output, a typical ECT device such as the Thymatron System IV (Somatics, LLC, Lake Bluff, IL) can provide approximately 504 mC of charge (Table 4) (64), which will be delivered as brief pulses of 0.5 ms each at a frequency of 70 Hz for a total stimulus duration of 8 s. Members of the Thymatron (Fig. 3) series (DX, DGX, and System IV) and similar devices such as those of the Spectrum series (4000M, 4000Q, 5000M, and 5000Q manufactured by MECTA, Lake Oswego, OR) are calibrated in such a way
Table 4. ECT Device Specifications (Thymatron System
IV)
Current: |
0.9 A (fixed) |
Frequency: |
10 to 140 Hz |
Pulsewidth: |
0.25 to 1.5 ms |
Duration: |
0.14 to 7.99 s |
Output: |
approx. 25 to 504 mC |
|
(5 to 99.4 J at 220 V) |
|
1008 mC (188.8 J at 220 V) |
|
with double-dose option |
Input: |
120 V AC, 60 Hz |
Recording: |
4 channel (2 EEG, EMG, ECG) |
|
|
Figure 3. Somatics Thymatron system IV ECT device (Image provided courtesy of Somatics, LLC).
that the user can select incremental quantities of charge. The device labels and manuals will usually refer to these as increments of ‘‘percent energy,’’ although the energy required to deliver the charge is actually dependent on the particular impedance of the patient being treated. The user (clinician) may have the option of individually adjusting such parameters as ‘‘percent energy’’ (charge), pulse frequency, pulsewidth, and total duration of pulse train. Both voltage and energy will be altered by the device to adjust for variations in impedance. The average impedance for a human receiving ECT is approximately 220 V, and the energy required to deliver 504 mC is 99.4 J (63).
Over an 8 s total stimulus duration, the average power for that interval is 99.4 J/8 s ¼ 12.4 W, although the power during each discrete electrical pulse is obviously much greater. Assuming a pulse frequency of 70 Hz (140 pulses/s with bidirectional current), delivered over a total stimulus duration (stimulus train) of 8 s, with a pulsewidth of 0.5 ms (or 0.0005 s), then the power during each discrete electrical pulse of this stimulus would be:
99:4 J=ð140 pulses=s 8 s 0:0005 s=pulseÞ
¼ 99:4 J=0:56 s ¼ 177:5 W
The stimulus is transmitted to the head of the patient (and, indirectly, to the brain) through externally applied scalp electrodes. These electrodes may either be stainless-steel discs held in place with an elastic band or self-adhesive flexible conductive pads. The stimulus electrodes can be applied in several configurations, including bilateral (also called bifronto-temporal), right unilateral, and bifrontal. In bilateral ECT, the electrodes are placed approximately 3 cm above the midpoint of a line between the canthus of the eye and tragus of the ear. With right unilateral ECT, the right electrode is placed in the conventional position for bilateral ECT, with the second electrode just to the right of the vertex of the skull. Bifrontal electrode placement is the newest of these various methods of performing ECT. Bifrontal placement is 5 cm above the angle of the orbit of the eye, which is usually found near the outer edge of the eyebrow. Comparative studies suggest that bilateral ECT may be more effective at lower energy levels, although right unilateral and bifrontal ECT may result in less cognitive impairment (64–68).
We consider the patient and device (including electrodes and cables) to be a circuit, and, for purposes of simplification, impedance in this circuit is usually treated as more or less equivalent to resistance. However, it should be recognized that impedance in the circuits being discussed has both resistive and reactive components (62). These reactive components are capacitance and inductance. Both inductance effects and capacitance in tissue are assumed to be low, but the treatment cables and electrode–skin interface may make a more significant contribution, altering both the amplitude and frequency of the stimulus. Complicating matters further, it should also be noted that the circuit impedance varies with the intensity of the stimulus. ECT devices typically provide a ‘‘static impedance’’ reading prior to treatment, which can vary widely, but is usually around 2000 V. The ‘‘dynamic impedance’’ can be measured during the stimulus and is substantially less, an average of about 200 V. The static impedance is measured with a very small test stimulus (insufficient to cause a seizure or even be detected by the patient). This static impedance is used primarily to test the integrity of the circuit. If the impedance is greater than 3000 V, it is assumed that either a break in the circuit occured or inadequate contact exists at the skin-electrode interface. Similarly, an excessively low impedance suggests shunting through a very low impedance channel (short-circuit) such as saline, conductive gel, or skin between closely applied electrodes. Interestingly, the seizure threshold (quantity of charge required to stimulate a seizure) is typically lower for unilateral than for bilateral ECT, despite the lower interelectrode distance with potential for lower impedance and greater shunting though scalp tissues with unilateral placement, which is thought to be a result of differing patterns of charge density, with maximum charge density in the frontal region for bilateral electrode placement and maximum charge density for unilateral placement in the region of the motor strip, an area of lower intrinsic seizure threshold (62).
SEIZURE RESPONSE
A seizure is characterized neurophysiologically by the paroxysmal synchronous discharge of populations of neurons. It is recognized clinically as abnormal behavior associated with abnormal neuronal activity and may present in a variety of different forms such as simple partial seizures, complex partial seizures, or generalized tonic-clonic seizures (69). During ECT, the patient is anesthetized and relaxed, so many of the clinical characteristics are altered. However, the observable characteristics of the ECT seizure are consistent with the generalized tonic-clonic type of seizure. The ECT stimulus predictably results in a pattern of spike and slow-wave activity that is distinctive and recognizable on EEG (70). The seizure activity rapidly spreads throughout both hemispheres and usually lasts for less than 60 s. The immediate goal of ECT is to produce such a seizure; stimuli that do not result in seizure activity appear to lack therapeutic benefit. However, it is possible to produce seizures, specifically with right unilateral ECT at or only slightly above the seizure threshold, that have a
ELECTROCONVULSIVE THERAPHY |
59 |
relatively weak therapeutic effect (64). Most experts recommend that right unilateral ECT be given with a stimulus that is at least five times the seizure threshold. Threshold may either be determined by titration (i.e., by giving a series of increasing stimuli), or the stimulus may be given at maximum energy. If bilateral or bifrontal electrode placement is used, energies just above the seizure threshold may be sufficient, and seizure threshold can be estimated based on the patient’s age (71).
Certain characteristics of the seizure activity may be associated with therapeutic efficacy, including coherence or symmetry between hemispheres of high amplitude slow waves on EEG and marked postictal suppression following the end of the seizure (61). Adjustments can be made in technique to try to improve response based on these characteristics and other seizure characteristics, including overall seizure duration.
MECHANISM OF ACTION OF ECT
The precise mechanisms of action of ECT are not well understood. A number of biochemical and physiological changes exist that have been detected following both ECT in humans and electroconvulsive shock (ECS) in animals. Some of these parallel those of antidepressant drugs, but others do not. In vivo studies of long-term ECS (and repeated tricyclic antidepressant drug administration) show increases in postsynaptic 5-hydroxytryptamine type 1a (5-HT-1a) receptor sensitivity. Long-term ECS increases 5-HT-2a receptors, but antidepressant administration in animals decreases 5-HT-2a receptors. Both antidepressant treatment and ECS reduce beta-adrenergic receptors (72). Evidence for increased dopaminergic activity with ECS and ECT exists, probably as a result of increased dopamine synthesis (73). Proton magnetic resonance spectroscopy measurements following ECT have demonstrated increases in concentrations of cortical gamma-amino butyric acid (GABA), an inhibitory neurotransmitter (74). This observation, as well as the finding that increasing seizure threshold during a course of ECT is associated with clinical response, has led to the hypothesis that a linked anticonvulsant and antidepressant response to ECT exists (61).
Magnetic resonance imaging (MRI) scans obtained before and after ECT have failed to demonstrate any structural changes in the brain. Positron emission tomography (PET) and single-photon emission computerized tomography (SPECT) scans of the brain during the ECT seizure show marked increases in global and regional metabolic activity and blood flow (75). However, PET scans taken several hours or days following ECT have shown a marked reduction in absolute and prefrontal activity (76). The majority of functional imaging studies with depressed patients have shown pretreatment deficits in similar regions (77). Paradoxically, those subjects with the greatest post-ECT reduction in the left prefrontal cortex show the greatest clinical response (78,79). One possible explanation for this may be that specific areas of the brain exist that are hypermetabolic in the depressed state and are suppressed by the effects of ECT, although, as mentioned
60 ELECTROCONVULSIVE THERAPHY
above, most scans show resting prefrontal hypoactivity in depression.
At the level of gene expression, ECS appears to induce brain-derived neurotrophic factor (BDNF) and its receptor, protein tyrosine kinase B (TrkB). Using our current understanding of the effects of ECS and neurotransmitter signal transduction, a model can be constructed that traces the effects of ECS/ECT-induced neuronal depolarization through pathways of norepinephrine (NE), 5-HT and glutamate release, monoamine receptors and ionotropic glutamate receptor binding by these neurotransmitters, cyclic adenosine monophosphate (cAMP) and other secondmessengers coupled to these receptors, and protein kinases stimulated by these second-messengers. Protein kinase A (PKA), protein kinase C (PKC), and calcium/calmodulindependent protein kinase (CaMK) phosphorylate and activate cAMP response element binding protein (CREB). CREB is a transcription factor for BDNF. BDNF then induces neuronal sprouting and may have other beneficial effects that reverse stress-induced neuronal atrophy (80) and, presumably, depression.
FUTURE DIRECTIONS FOR ELECTROMAGNETIC BRAIN STIMULATION
A number of unanswered questions regarding ECT still exist, including such questions as:
-What are the most effective methods of maintenance therapy (medications, ECT, or both) following an acute course of treatment?
-Which medications (including antidepressants, antipsychotics, and mood stabilizers) can be successfully and safely combined with ECT?
-What is the best electrode placement from a treatment efficacy and side-effect point of view?
-How can the ECT stimulus be modified to make it more therapeutically effective and diminish side effects (especially cognitive effects)?
-What is the actual mechanism (or mechanisms) by which ECT exerts its antidepressant, antipsychotic, and other beneficial effects?
ECT itself is no longer the only form of electromagnetic brain stimulation. Both rTMS (often referred to simply as TMS) and VNS have shown promise for the treatment of mood disorders (79,81). As it does not involve the production of seizures and therefore requires no anesthesia, TMS is a particularly attractive alternative to ECT, especially for mood disorders resistant to treatment with medication. MST involves magnetic stimulation at frequencies designed to provoke seizures. This technique obviously requires general anesthesia and muscle relaxation just as ECT does. The hope is that MST may be as effective as ECT, but with less cognitive impairment due to the more focal nature of the stimulus.
ECT will remain an important option for severe and treatment-refractory psychiatric illness for the foreseeable future. An improved understanding of the pathophysiology of psychiatric illness as well as the mechanism of action of
electromagnetic brain stimulation will lead to further refinements in technique that will make ECT and related therapies safer, more effective, and more acceptable to patients and their families. The availability of alternative methods of brain stimulation will provide a wider range of choices and will create opportunities for combining therapies in ways that will be more compatible with individual patients’ needs. Although changing social and political conditions may affect its image and public acceptance, it is unlikely that ECT will disappear or be replaced for some time to come.
ACKNOWLEDGMENTS
The authors would like to express their appreciation to Carol Burns, RN, ECT Program Coordinator of the Medical University of South Carolina Department of Psychiatry and Behavioral Sciences and to Drs. Melinda Bailey and Gary Haynes of the Medical University of South Carolina Department of Anesthesiology for their helpful advice during the preparation of this article.
BIBLIOGRAPHY
Cited References
1.Mudur G. Indian group seeks ban on use of electroconvulsive therapy without anesthesia. Br Med J 2002;324(6):806.
2.American Psychiatric Association. The Practice of Electroconvulsive Therapy: Recommendations for Treatment, Training and Privileging, A Task Force Report of the American Psychiatric Association. 2nd ed. Washington (DC): American Psychiatric Press, Inc.; 2000.
3.Kellner CH, Pritchett JT, Beale MD, Coffey CE. Handbook of ECT. Washington (DC): American Psychiatric Press, Inc.; 2001.
4.Fink M. Meduna and the origins of convulsive therapy. Am J Psychiatry 1984;141(9):1034–1041.
5.Fink M. Convulsive therapy: A review of the first 55 years. J Affect Disord 2001;63:1–15.
6.Fink M. Induced seizures as psychiatric therapy: Ladislas Meduna’s contributions in modern neuroscience. J ECT 2004; 20:133–136.
7.Bennett AE. Curare: A preventive of traumatic complications in convulsive shock therapy. Convulsive Ther 1997;13:93– 107. Originally published in the Am J Psychiatry 1941; 97:1040–1060.
8.Weiner RD, Rogers HJ, Davidson JR, Kahn EM. Effects of electroconvulsive therapy upon brain electrical activity. Ann NY Acad Sci 1986;462:270–281.
9.Weiner RD, Rogers HJ, Davidson JR, Squire LR. Effects of stimulus parameters on cognitive side effects. Ann NY Acad Sci 1986;462:315–325.
10.Klapheke MM. Electroconvulsive therapy consultation: An update. Convulsive Ther 1997;13:227–241.
11.Coffey CE. The role of structural brain imaging in ECT. Psychopharmacol Bull 1994;30:477–483.
12.Kellner CH. The CT scan (or MRI) before ECT: A wonderful test has been overused. Convulsive Ther 1996;12:79–80.
13.McDonald A, Walter G. The portrayal of ECT in American movies. J ECT 2001;17(4):264–274.
14.Appelbaum PS, Grisso T. Assessing patients’ capacities to consent to treatment. N Engl J Med 1988;319(25):1635– 1638.
15.Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Text Revision (DSM-IV-TR1), Washington (DC): American Psychiatric Press, Inc.; 2000.
16.Griesemer DA, Kellner CA, Beale MD, Smith GM. Electroconvulsive therapy for treatment of intractable seizures: Initial findings in two children. Neurology 1997;49.
17.DeBattista C, Mueller K. Is electroconvulsive therapy effective for the depressed patient with comorbid borderline personality disorder? J ECT 2001;17(2):91–98.
18.Feske U, Mulsant BH, Pilkonis PA, Soloff P, Dolata D, Sackeim HA, Haskett RF. Clinical outcome of ECT in patients with major depression and comorbid borderline personality disorder. Am J Psychiatry 2004;161(11):2073– 2080.
19.Sareen J, Enns MW, Guertin J. The impact of clinically diagnoses personality disorders on acute and one-year outcomes of electroconvulsive therapy. J ECT 2000;16(1):43– 51.
20.Fink M. The broad clinical activity of ECT should not be ignored. J ECT 2001;17(4):233–235.
21.Ghaziuddin N, Kutcher SP, Knapp P, Bernet W, Arnold V, Beitchman J, Benson RS, Bukstein O, Kinlan J, McClellan J, Rue D, Shaw JA, Stock S, Kroeger K. Practice parameter for use of electroconvulsive therapy with adolescents. J Am Acad Child Adolesc Psychiatry 2004;43(12):1521–1539.
22.Cohen D, Paillere-Martinot M-L, Basquin M. Use of electroconvulsive therapy in adolescents. Convulsive Ther 1997;13: 25–31.
23.Moise FN, Petrides G. Case study: Electroconvulsive therapy in adolescents. J Am Acad Child Adolesc Psychiatry 1996;35: 312–318.
24.Schneekloth TD, Rummans TA, Logan K. Electroconvulsive therapy in adolescents. Convulsive Ther 1993;9:158–166.
25.Bertagnoli MW, Borchardt CM. A review of ECT for children and adolescents. J Am Acad Child Adolesc Psychiatry 1990; 29:302–307.
26.Yonkers KA, Wisner KL, Stowe Z, Leibenluft E, Cohen L, Miller L, Manber R, Viguera A, Suppes T, Altshuler L. Management of bipolar disorder during pregnancy and the postpartum period. Am J Psychiatry 2004;161:608–620.
27.Walker R, Swartz CM. Electroconvulsive therapy during high-risk pregnancy. Gen Hosp Psychiatry 1994;16:348–353.
28.Kelly KG, Zisselman M. Update on electroconvulsive therapy (ECT) in older adults. J Am Geriatr Soc 2000;48(5):560– 566.
29.O’Connor MK, Knapp R, Husain M, Rummans TA, Petrides G, Snyder GK, Bernstein H, Rush J, Fink M, Kellner C. The influence of age on the response of major depression to electroconvulsive therapy: A C.O.R.E. report. Am J Geriatr Psychiatry 2001;9:382–390.
30.McKinney PA, Beale MD, Kellner CH. Electroconvulsive therapy in a patient with cerebellar meningioma. J ECT 1998; 14(1):49–52.
31.Abrams R. The mortality rate with ECT. Convulsive Ther 1997;13:125–127.
32.Nuttall GA, Bowersox MR, Douglass SB, McDonald J, Rasmussen LJ, Decker PA, Oliver WC, Rasmussen KG. Morbidity and mortality in the use of electroconvulsive therapy. J ECT 2004;20(4):237–241.
33.Zielinski RJ, Roose SP, Devanand DP, Woodring S, Sackeim HA. Cardiovascular complications in depressed patients with cardiac disease. Am J Psychiatry 1993;150:904–909.
34.Lisanby SH, Maddox JH, Prudic J, Davanand DP, Sackeim HA. The effects of electroconvulsive therapy on memory of autobiographical and public events. Arch Gen Psychiatry 2000;57:581–590.
ELECTROCONVULSIVE THERAPHY |
61 |
35.Fink M. A new appreciation of ECT. Psychiatric Times 2004; 21(4):
36.Donahue AB. Electroconvulsive therapy and memory loss. J ECT 2000;16(2):133–143.
37.Abrams R. Does brief-pulse ECT cause persistent or permanent memory impairment? J ECT 2002;18:71–73.
38.American Psychiatric Association. The Practice of Electroconvulsive Therapy: Recommendations for Treatment, Training and Privileging, A Task Force Report of the American Psychiatric Association. Washington, DC: American Psychiatric Press, Inc.; 1990.
¨¨
39.Lauritzen L, Odgaard K, Clemmesen L, Lunde M, Ohrstrom J, Black C, Bech P. Relapse prevention by means of paroxetine in ECT-treated patients with major depression: A comparison with imipramine and placebo in medium-term continuation therapy. Acta Psychiatrica Scandanavica 1996;94:241–251.
40.Hirose S, Ashby CR, Mills MJ. Effectiveness of ECT combined with risperidone against aggression in schizophrenia. J ECT 2001;17:22–26.
41.Sjatovic M, Meltzer HY. The effect of short-term electroconvulsive treatment plus neuroleptics in treatment-resistant schizophrenia and schizoaffective disorder. J ECT 1993;9: 167–175.
42.Chanpattana W, Chakrabhand MLS, Kongsakon R, Techakasem P, Buppanharun W. Short-term effect of combined ECT and neuroleptic therapy in treatment-resistant schizophrenia. J ECT 1999;15:129–139.
43.Tang WK, Ungvari GS. Efficacy of electroconvulsive therapy combined with antipsychotic medication in treatmentresistant schizophrenia: A prospective, open trial. J ECT 2002; 18:90–94.
44.Frankenburg FR, Suppes T, McLean P. Combined clozapine and electroconvulsive therapy. Convulsive Ther 1993;9: 176–180.
45.Kellner CH, Nixon DW, Bernstein HJ. ECT-drug interactions: A review. Psychopharmacol Bull 1991;27(4):
46.Mukherjee S. Combined ECT and lithium therapy. Convulsive Ther 1993;9(4):274–284.
47.Klapheke MM. Combining ECT and antipsychotic agents: Benefits and risks. Convulsive Ther 1993;9:241–255.
48.Carr ME, Woods JW. Electroconvulsive therapy in a patient with unsuspected pheochromocytoma. Southern Med J 1985; 78(5):613–615.
49.Weiner R. Electroconvulsive therapy in the medical and neurologic patient. In: Stoudemire A, Fogel BS, editors. Psychiatric Care of the Medical Patient. New York: Oxford University Press; 1993.
50.Edwards RM, Stoudemire A, Vela MA, Morris R. Intraocular changes in nonglaucomatous patients undergoing electroconvulsive therapy. Convulsive Ther 1990;6(3):209– 213.
51.Good MS, Dolenc TJ, Rasmussen KG. Electroconvulsive therapy in a patient with glaucoma. J ECT 2004;20(1):48–49.
52.Kellner C. Lessons from the methohexital shortage. J ECT 2003;19(3):127–128.
53.Stadtland C, Erhurth A, Ruta U, Michael N. A switch from propofol to etomidate during an ECT course increases EEG and motor seizure duration. J ECT 2002;18(1):22–25.
54.Folk JW, Kellner CH, Beale MD, Conroy JM, Duc TA. Anesthesia for electroconvulsive therapy: A review. J ECT 2000;16:157–170.
55.Ding Z, White PF. Anesthesia for electroconvulsive therapy. Anesthesia Analgesia 2002;94:1351–1364.
56.Bhat SK, Acosta D, Swartz C. Postictal systole during ECT. J ECT 2002;18(2):103–106.
