
Ghai Essential Pediatrics8th
.pdf
------------------------------------N_e_w_b_o_r_ni_n_fa_ _nt_s
four times daily for very small babies (<2 kg) and every two hour for sick babies. Mother should be encouraged to assess body temperature of the neonate by touching the baby.
Disorders of Body Temperature
Hypothermia mayhappen as aresult of exposure to a cold environment such as low ambient temperature, cold surface, or cold air, or the baby is wet or not clothed adequately. Hyperthermia may result if the infant is exposed to warm environmentsuchas in summers, direct sun exposure, or overheating in the incubator or radiant warmer. Hypothermia as well as hyperthermia can also indicate underlying serious illness.
Hypothermia
Prevention
Warm chain: The strategy for prevention of hypothermia is known as warm chain. The 'warm chain' is a set of ten steps (Table8.10)aimed atdecreasingheatloss, promoting heat gain and ensuring that baby is not exposed to the circumstances that can result in hypothermia.
Table 8.10: Ten steps of warm chain
i.Warm delivery room
ii.Warm resuscitation
iii.Immediate drying
iv.Skin to skin contact
v.Breastfeeding
vi.Bathing postponed
vii.Appropriate clothing
viii.Mother and baby together
ix.Professional alertness
x.Warm transportation
•The birthing room should have ambient temperature of at least 25°C and should be free from drafts of air (keep windows and doors closed).
•After delivery, the baby should be dried immediately, put in skin to skin contact on mother's abdomen and covered by warm and dry linen. The wet towel should be discarded. The baby should be capped and dressed adequately (Fig. 8.23).
•Kangaroo mother care (KMC) is an effective way to keep LBW baby warm.
•Frequent breastfeeding is critical to provide energy to keep the baby warm.
•Bathing and weighing are postponed. Term babies can be sponged after 24 hr of life in summer months. Bathing should be postponed during winters and in sick or LBWbabies until the umbilical cordfalls off (end of first week). Dressing the baby in multiple layers of warm and light clothes provides better thermal protection than a single layer of heavy woolen clothing.
Fig. 8.23: A well clothed baby
•Mother and baby should be kept on the same bed (co-bedding/rooming in).
•Warm transportation: This is the weakest link in the warm chain with greatest possibility of severe and undetected hypothermia.
•Training/awareness of healthcare providers: Unless persons involved in the care of newborns realize the implications of hypothermia it cannot be detected or managed effectively.
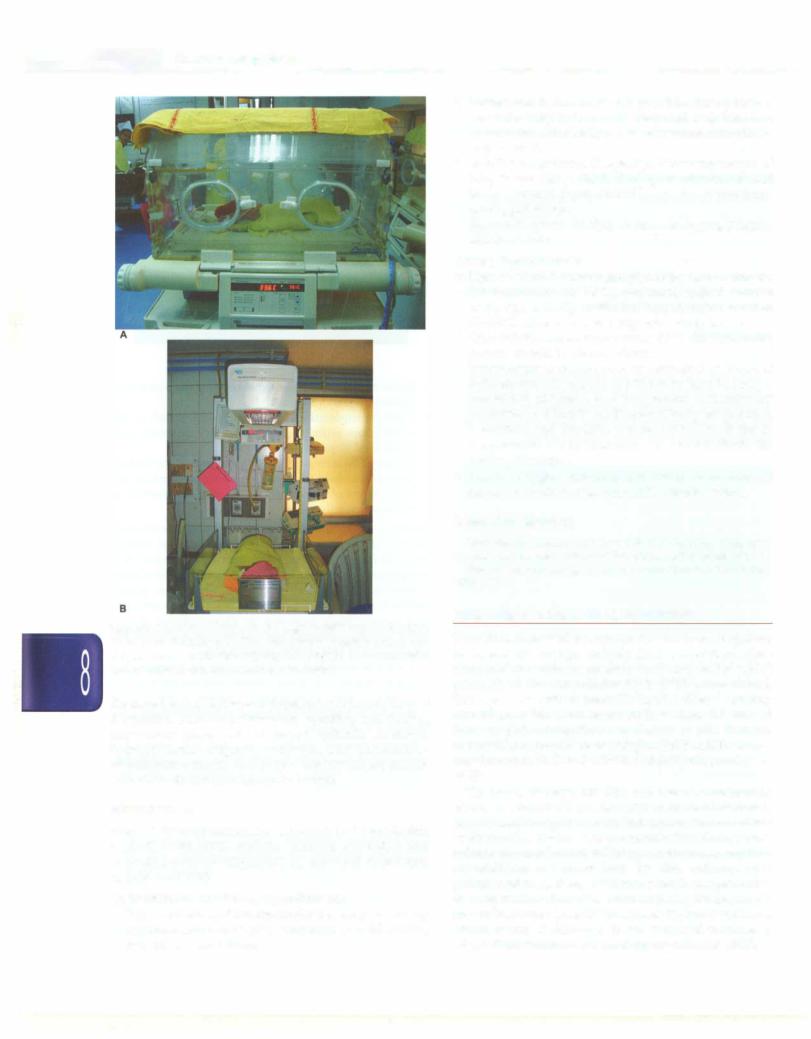
Incubators and radiant warmers. These equipment are used to assist sick and small neonates maintain their normal body temperature (Figs 8.24A and B). Incubator is a transparent acrylic cabin which has warm air circulating around the baby to keep him warm. There is an inbuilt feedback system (servo-control) that controls ambient temperature inside incubator by altering heater output based on baby's temperature and thereby maintains the temperature of baby in the normal range.
A radiant warmer is an open system (as compared to incubator which is a closed cabinet) and the neonate lies on a crib. There is overhead radiant warmer that modulates its heater output based on baby's temperature sensed by a skin probe.
Radiant warmers and incubators should be used in the servo control mode with the abdominal skin temperature maintained at 36.5°C to 37°C depending on the birth weight of the neonate.
Signs and Symptoms
Peripheral vasoconstriction results in acrocyanosis, cool extremities and delayed peripheral capillary refill time (CRT). The baby becomes restless and then lethargic. Chronic or recurrent episodes of hypothermia result in poor weight gain. Cardiovascular manifestations may occur in the form of bradycardia, hypotension, raised pulmonary artery pressure with resultant hypoxemia, tachypnea anddistress. Presence oflethargy,poorreflexes,
E |
_s_s _e _n_t1a_1_P_ e_d_1a_ tr1_cs---------------------------- |
- |
|
Figs 8.24A and B: A very low birth weight (VLBW) baby being cared for in (A) an incubator and (B) radiant warmer. Note that baby is well clothed and the incubator is covered with cloth to prevent excessive light or noise for adequate comfort of the baby
decreased oral acceptance and apnea denotes neurological depression. Abdomen distension, vomiting and feeding intolerance make enteral intake difficult. Acidosis, hypoglycemia, oliguria, azotemia and generalized bleeding canoccur in severe cases. Babies whoare chronic cold stress do not gain adequate weight.
Management
Methodsfortemperaturemaintenanceinclude skin to skin contact, warm room, radiant warmers, incubators and increasing ambient temperature by use of hot air blowers, or a 200 watt bulb.
Cold stress or moderate hypothermia
•Remove the baby from the source that may be causing hypothermia such as cold environment, cold clothes, cold air or wet clothing.
•Initiate skin to skin contact, is possible. If not possible, dress the baby in warm clothing and keep him in a warm room. Alternately a radiant warmer or incubator may be used.
•Monitor temperature frequently. If the temperature of baby is not rising, check if adequate amount of heat being provided. Sepsis should be suspected unrespon sive hypothermia.
•Ensure frequent feeding to prevent hypoglycemia. Monitor vitals.
Severe hypothermia
•Remove all wet clothing and place baby in an incubator (air temperature 35-36°C), preheated radiant warmer
or thermostatically controlled heated mattress set at 37-38°C. Alternately, one may use a room heater.
•Once baby's temperature reaches 34°C, the rewarming process should be slowed down.
•Temperature is measured every hour for 3 hr. If rise of temperature has been by 05°C per hr then heating is considered adequate, and temperature measurement is continued 2 hourly until normal body temperature is attained, and thereafter 3 hourly for 12 hr. If rise of temperature is not adequate, one should check the heating technique.
•Provide oxygen, empirical antibiotics, saline bolus if shock, IV dextrose and vitamin K. Monitor vitals.
Suggested Reading
Guidelines for perinatal care. Second Edition, American Academy of Pediatrics and American College ofObstetricians and Gynecologists, 1998 Thermal protection of the newborn: A practical guide. WHO/FHW/
MSM/97.2
FLUID AND ELECTROLYTE MANAGEMENT
Transition from fetal to extrauterine life is accompanied by remarkable changes in body fluid composition. Neo nates are born with an excess of total body water (TBW) primarily in the extracellular fluid (ECF) compartment. This excess of TBW is normally lost by diuresis during first week of life. Term neonates lose about 7%-10% of body weight during first 3 to 5 days of life. Preterm neonateshaveproportionatelyhigherTBWand,therefore, may lose up to 10%-15% of birth weight during first week of life.
The heart, kidneys, the skin and the neuroendocrine system regulate fluid and electrolyte balance in neonates. In neonates,kidneyshavealimitedcapacityto concentrate or dilute urine due to lower glomerular filtration rate and reduced proximal and distal tubular sodiumreabsorption. In addition to water loss by the kidneys and gastrointestinal system, additional water losses occur due to evaporation from the skin and respiratory tract (insensible water loss; IWL). IWL is higher in preterm
infants owing to thin skin. Fever, increased respiratory rate, radiant warmers and phototherapy increase IWL.
Newborn Infants -
Guldellnes for Fluld Therapy
Healthy babies of 1200 g or more should be started on enteral feeding with breast milk. A baby of 1800 g or more would be able to breastfeed directly while a smaller baby may require expressed breast milk fed by suitable alternate route.
Intravenous (IV)fluid therapy. IV fluids are indicated when baby is either small or sick. Babies less than 1200 g or gestation <30 week should be started on IV fluids routinely. Sick babies (irrespective of weight or gestation) such as those with respiratory distress, significant asphyxia, feed intolerance, hemodynamic instability, gastrointestinal malformations (like tracheoesophgeal fistula, intestinal atresia, etc.) or any other severe illness precluding oral feeding should be given IV fluids. Peripheral intravenous line is the most common route used to provide fluids. Fluid requirement is calculated based on birth weight, day of life and the current fluid balance.
Babies with birth weight :2,1500 g. Infants on IV fluids require to excrete a solute load of about 15 mOsm/kg/day in the urine. To excrete this solute load at a urine osmolarity of 300 mOsm/kg/day, the infant would have to pass a minimum of 40 ml/kg/day of urine. Allowing for an additional IWL of 20 ml/kg, the initial fluids should be 60-80 ml/kg/day. The initial fluids should be 10% dextrose with no electrolytes in order to maintain a glucose infusion rate of 4-6 mg/kg/min. (Table 8.11). As the infant grows and receives enteral feeds, the solute load presented to the kidneys increases and the infant requires more fluid to excrete the solute load. Water is also required for fecal losses and for growth purposes. Therefore, the fluid requirements increase by 15-20 ml/kg/day till a maxi mum of 150 ml/kg/day by the 7th day. Sodium and potassium should be added to IV fluids after 48 hr.
Babies with birthweight <1500 g. The urine output in these babies is similar to a baby of 1500 g or more. However, the fluid requirement is higher due to increased IWL. These babies need 80 ml/kg/day of 10% dextrose on day 1 of life (Table 8.11). The babies should be well dressed including provision of caps and socks to reduce the IWL under the radiant warmer. As the skin matures, the IWL progressively decreases and fluid requirement becomes similar to bigger babies. Fluids need to be increased at
10-15 ml/kg/day up to a maximum of 150 ml/kg/day by 5th to 7th day. Sodium and potassium should be added to IV fluids after 48 hr.
Problems with IV fluid therapy include local and systemic infection, phlebitis, fluid overload and extra vasation. Because IV fluid therapy is a major risk factor for nosocomial infection, all asepsis precautions must be followed during insertion of IV cannula or administering fluids. Oral feeds should be started at the earliest possible opportunity when clinical condition of neonate improves and IV fluid should be stopped when oral feeds constitute about two-thirds of daily fluid requirement. IV sites should be inspected frequently to timely detect extravasation.
Calculation of fluids for a 1250 g baby:
Day 1: 100 ml (80 ml/kg) to be infused at 4.2 ml/hr Day 2: 120 ml (95 ml/kg) to be infused at 5.0 ml/hr
Monitoring of Fluid and Electrolyte Status
Fluid therapy should be monitored every 12 to 24 hr in a baby on IV fluids using following parameters:
Body weight. Serial weight measurements can be used as a guide to estimate the fluid deficit in newborns. Term neonates lose 1-3% of their birth weight daily with a cumulative loss of 5-10% in the first week of life. Preterm neonates lose 2-3% of their birth weight daily with a cumulative loss of 10-15% in the first week of life. Failure to lose weight in the first week of life may be an indicator of excessive fluid administration. However, excessive weight loss (>3% in 24 hr) in the first 5-7 days or later would be non-physiological and would merit correction with fluid therapy.
Clinical examination. The usual physical signsof dehydration are unreliable in neonates. Infants with 10% (100 ml/kg) dehydration may have sunken eyes and fontanel, cold and clammy skin, poor skin turgor and oliguria. Infants with 15% (150 ml/kg) or more dehydration would have signs of shock (hypotension, tachycardia and weak pulses).
Urine output. A well hydrated baby would pass urine at 1 to 3 ml/kg/hr.
Suggested Reading
Chawla D, Agarwal R, Deorari AK, Paul VK. Fluid and electrolyte management in term and preterm neonates. Indian J Pediatr. 2008;75:255-9
Table 8.11: Dally fluid requirements during first week of life (ml/kg/day)
Birth weight |
Day 1 |
<1500 g |
80 |
1500 g |
60 |
Day 2
95
75
Day 3 |
Day 4 |
Day 5 |
Dny 6 |
Day 7 and onwards |
110 |
120 |
130 |
140 |
150 |
90 |
105 |
120 |
135 |
150 |
n i i is _____________
___Ess_e t al_Pe_d__atr_c _________________ _
KANGAROO MOTHER C_A_R_E________
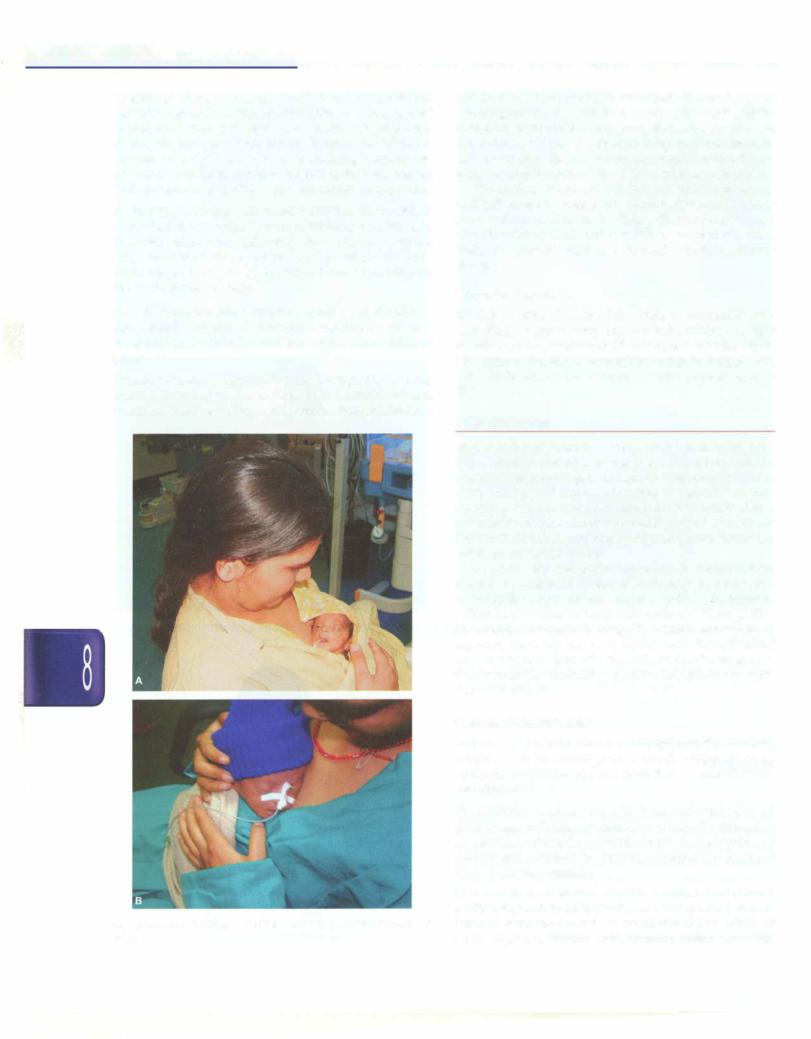
Kangaroo mother care (KMC) refers to care of preterm or low birth weight infants by placing the infant in skin-to skin contact with the mother or any other caregiver. Initially conceived as an alternative to conventional warmer care for LBW infants, KMC has now become standard of care either as an alternative to or an adjunct to technology-based care.
KMC was first suggested in 1978 by Dr Edgar Rey in Bogota, Colombia. The termkangaroocare isderivedfrom practicalsimilarities tomarsupialcaregiving,i.e. theinfant is kept warm in thematernalpouch and close tothebreasts for unlimited feeding.
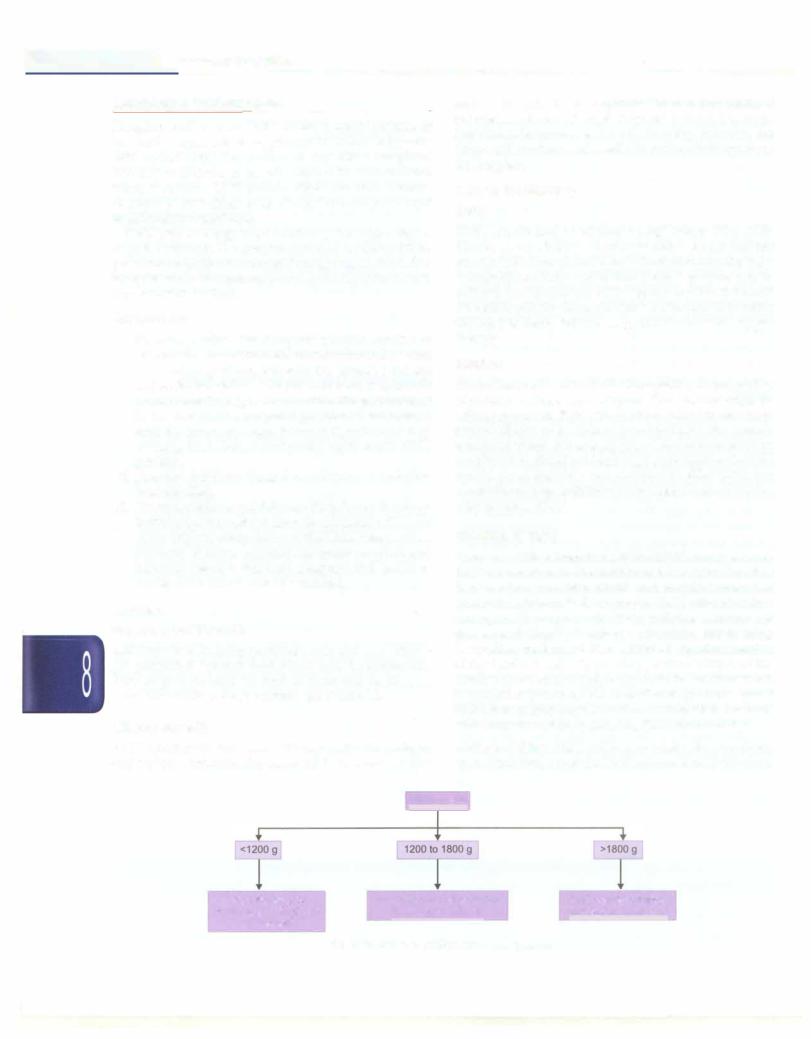
Componen ts
i.Kangaroo position. The kangaroo position consists of skin-to-skincontactbetweenthemotherand theinfant in a vertical position, between the mother's breasts andunder herclothes.Theprovidermustkeep herself in a semi-reclining position to avoid the gastric reflux in the infant. The kangaroo position is maintained until the infant no longer tolerates it, as indicated by sweating in the baby or baby refusing to stay in KMC position.
ii.Kangaroo nutrition: Kangaroo nutrition is exclusive breastfeeding.
iii.Kangaroo discharge andJollowup: Early home discharge in the kangaroo position from the neonatal unit is one of the original components of the KMC intervention. Mothers at home require adequate support and followup hence a followup program and access to emergency services must be ensured.
Benefits
Physiological Benefits
KMC results in keeping neonates warm and cozy. Babies get protected against cold stress and hypothermia. Physiological parameters such as heart and respiratory rates, oxygenation, sleep patterns get stabilized.
Clinical Benefits
KMC significantly increases milk production in mothers and exclusive breastfeeding rates. KMC improves weight
gain in the infants and improves thermal protection. It reduces incidence of respiratory tract and nosocomial infections, improves emotional bonding between the infant and mothers and results in earlier discharge from the hospital.
Criteriafor Eligibility
Baby
KMC is indicated in all stable LBW babies (Fig. 8.25). However, sick babies should be cared under radiant warmer initiallyandKMCshould be startedoncethebaby is hemodynamically stable. Short KMC sessions can be initiated during recoverywithongoing medical treatment (IV fluids, oxygen therapy). KMC can be provided while the baby is being fed via orogastric tube or on oxygen therapy.
Mother
All mothers can provide KMC, irrespective of age, parity, education, culture and religion. The mother must be willing to provide KMC. The mother should be free from serious illness to be able to provide KMC. She should receive adequate diet and supplements recommended by herphysician.Sheshould maintain good hygiene. Mother would need family's cooperation to deal with her conventional responsibilities of household chores till the baby requires KMC.
Initiation of KMC
Counseling. When baby is ready for KMC, arrange a time that is convenient to the mother and her baby. The first few sessions are important and require extended interaction. Demonstrate to her the KMC procedure in a caring, gentle manner and with patience. Answer her queries and allay her anxieties. Encourage her to bring her mother/mother-in-law,husbandor any othermember of the family. It helps in building positive attitude of the family and ensuring family support to the mother which is particularly crucial for post-discharge home-based KMC. It is helpful that themother starting KMC interacts with someone already practicing KMC for her baby.
Mother's clothing. KMC can be provided using any front open, light dress as per the local culture. KMC works well
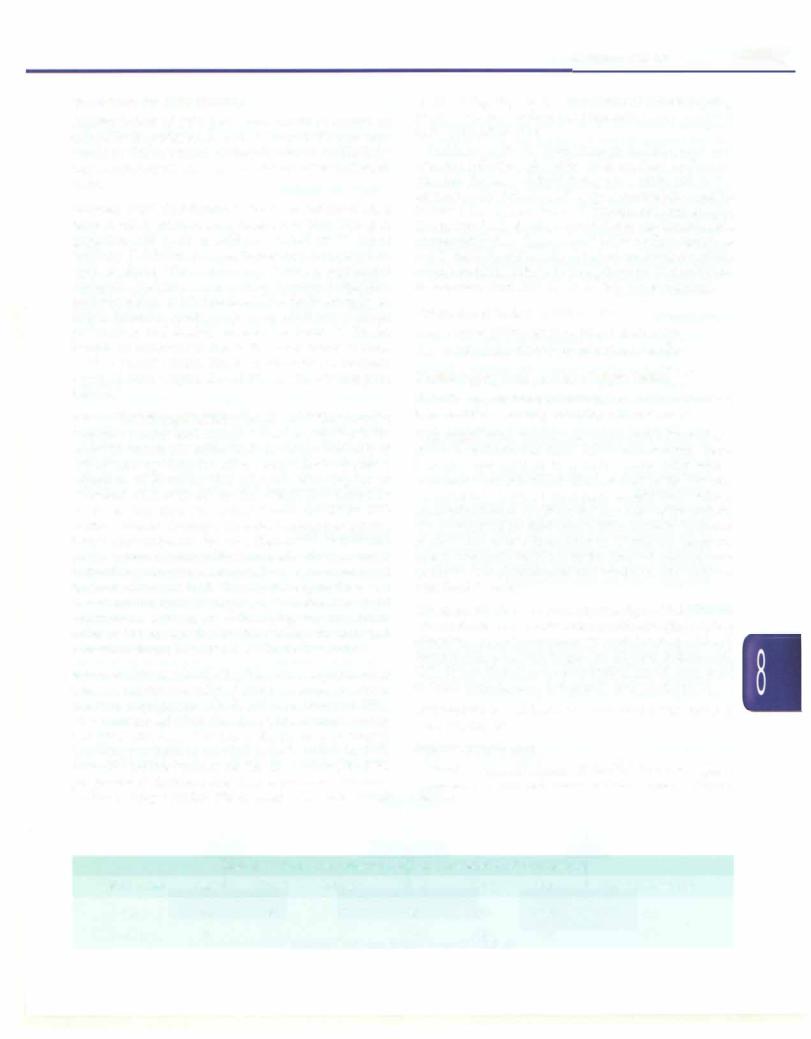
Birth weight
May take days to |
May take a few days before |
KMC can be initiated |
||
weeks before KMC can |
KMC can be initiated |
immediately after birth |
||
be initiated |
|
|
|
|
Fig 8.25: Kangaroo mother care (KMC) protocol |
|
|||
|
|
|||
------------------------------------N_e_w_b_o_r_n_i_n_ta_ n t s ....
J
I
D
Figs 8.26A to D: (A) Mother and (B) father practicing KMC in front open gown and shawl; (C) AIIMS KMCjacket; and (D) mother performing KMC using AIIMS KMC jacket
with blouse and sari, gown or shawl (Fig. 8.26). Suitable apparel that can retain the baby for extended period of time can be adapted locally.
Baby's clothing. Baby is dressed with cap, socks, nappy and front open sleeveless shirt.
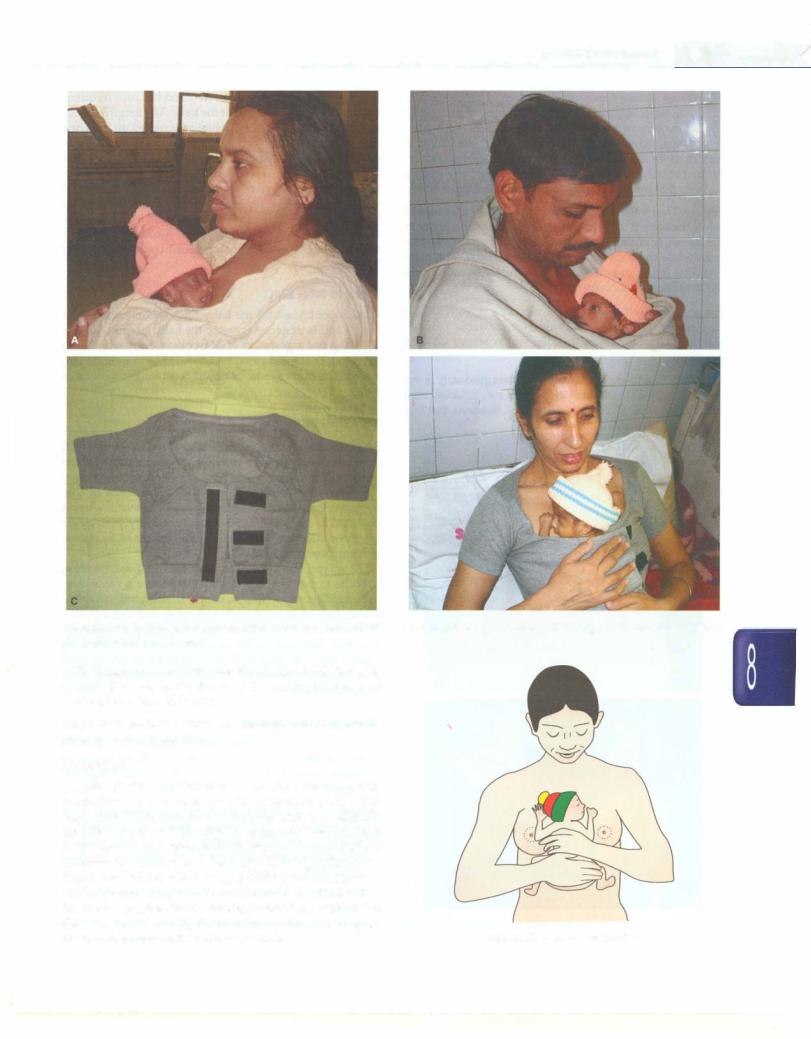
Procedure
Kangaroo positioning. The baby should be placed between |
|
the mother's breasts in an upright position (Fig. 8.27). The |
|
head should be turned to one side and in a slightly |
|
extended position. This slightly extended head position |
|
keeps the airway open and allows eye to eye contact |
|
between the mother and her baby. The hips should be |
|
flexed and abducted in a 'frog' position; the arms should |
|
also be flexed. Baby's abdomen should be at the level of |
|
the mother's epigastrium. Mother's breathing stimulates |
|
the baby, thus reducing the occurrence of apnea. Support |
|
the baby's bottom with a sling or binder. |
Fig. 8.27: Kangaroo positioning |
-1o..E_s_s_e _n_t1_a1_Pe_d_ 1_a_tr_1c_s____________________________ _
Monitoring. Babies receiving KMC should be monitored carefully, especially during the initial stages. Nursing staff should make sure that baby's neck position is neither too flexed nor too extended, airway is clear, breathing is regular, color is pink and baby ismaintaining temperature. Mother should be involved in observing the baby during KMC so that she herself can continue monitoring at home.
Feeding. Themothershouldbe explainedhowto breastfeed while the baby is in KMC position. Holding the baby near the breast stimulates milk production. She may express milk while the baby is still in KMC position. The baby could be fed with paladai, spoon or tube, depending on the condition of the baby.
Privacy. The staff must respect mother's sensitivities in this regard and ensure culturally acceptable privacy standards in the nursery and the wards where KMC is practised.
Duration. Skin-to-skincontactshould startgraduallyinthe nursery, with a smooth transition from conventional care to continuous KMC (Figs 8.28A and B). Sessions that last
Figs 8.28A and B: Kangaroo mother care being provided in postnatal ward
less than one hour should be avoided because frequent handling may be stressfulforthebaby.Thelength of skin to-skin contact should be gradually increased up to 24hr a day,interruptedonlyfor changingdiapers. Whenthebaby does not require intensive care, she should be transferred to the postnatal ward where KMC should be continued.
The mother can sleep with baby in KMC position in reclined or semi-recumbent position about 30 degrees from horizontal. This can be done with an adjustable bed or with pillows on an ordinary bed. A comfortable chair with an adjustable back may be used for resting during the day.
When to Stop KMC
KMC is continued till the baby finds it comfortable and cosy. KMC is unnecessary once the baby attains a weight of 2500 g and a gestation of 37 weeks. A baby who, upon being put in the kangaroo position, tends to wriggle out, pulls limbs out, or cries or fusses is no longer in need of KMC.
BREASTFEEDING
Breast milk is an ideal food for neonates. It is the best gift that a mother can give to her baby. It contains all the nutrients for normal growth and development of a baby from the time of birth to the first six months of life. Ensuring exclusive breastfeeding for six months has a potential to reduce under-5 mortality rate by 13%, by far the most effective intervention that is known to reduce newborn and child deaths.
To accrue the maximum benefits, the breastfeeding must be exclusive (only breast milk; nothing other than breast milk except vitamin drops, if indicated), initiated within half an hour of birth and continued through first six months after birth. Coverage Evaluation Survey (2009) reported that only 33.5% of infants were breastfeeding startedwithin anhour of birth. Only 36.8% of infants aged 6 to 9 months received exclusive breastfeeding until 6 months of age.
Benefits of Breast Milk
Nutritionalsuperiority. Breastmilkcontainsall the nutrients a baby needs for normal growth and development, in an optimum proportion and in a form that is easily digested and absorbed.
Carbohydrates. Lactose is in a high concentration (6-7 g/ dl) in breast milk.The galactose is necessary for formation of galactocerebrosides. Lactose helps in absorption of calcium and enhances the growth of lactobacilli, the good bacteria, in the intestine.
Proteins. The protein content of breast milk is low (0.9-1.1 g/dl) compared to animal milk. Most of the protein is in form of lactalbumin and lactoglobulin (60%), which is easily digested. Human milk contains amino acids like
taurine and cysteine which are necessary for neuro transmission and neuromodulation. These are lacking in cow milk and formula.
Fats. Breast milk is rich in polyunsaturated fatty acids, necessary for the myelination of the nervous system. It also contains omega 2 and omega 6 (very long chain) fatty acids, which are important for the formation of prosta glandins and cholesterol, required as a base for steroid hormones.
Vitamins and minerals. The quantity and bioavailability of vitamins and minerals is sufficient to the needs of the baby in the first 6 months of life.
Water and electrolytes. Breast milk has a water content of 88% and hence a breastfed baby does not require any additional water in the first few months of life even during summer months. The osmolality of breast milk is low, presenting a low solute load to the kidneys.
Immunological superiority. Breast milk contains a number of protective factors which include immunoglobulin mainly secretary IgA, macrophages, lymphocytes, lactoferrin, lysozyme, bifidus factor and interferon among others. Breastfed babies are less likely to develop infection. A breastfed baby is 14 times less likely to die of diarrhea and almost four times less likely to die of respiratory infection.
Other benefits. Breast milk contains a number of growth factor, enzymes and hormones. The epidermal growth factor in breast milk enhances maturation of the intestinal cells and reduces the risk of allergy in later life. Enzymes like lipases increase the digestion of fats in the milk.
Protection against other illness. Breastfed babies have a lower risk of allergy, ear infections and orthodontic problems. They have a lower risk of diabetes, heart disease and lymphoma in later life.
Mental growth. Babies who are breastfed are better bonded to their mothers. Studies have shown that babies who were breastfed had a higher IQ than those babies who were given other forms of milk.
Benefits to mother. Breastfeeding soon after birth helps uterine involution, reducing chances of postpartum hemorrhage. It provides protection against pregnancy due to lactational amenorrhea. If the mother has been exclusively breastfeeding her baby and has not resumed menses then there is no need for any other contraception during initial 6 months after delivery.
Breastfeeding is most convenient and time saving. It reduces the risk of cancer of breast and ovary. Breast feeding is the most effective way of shedding extra weight that mother has gained during pregnancy.
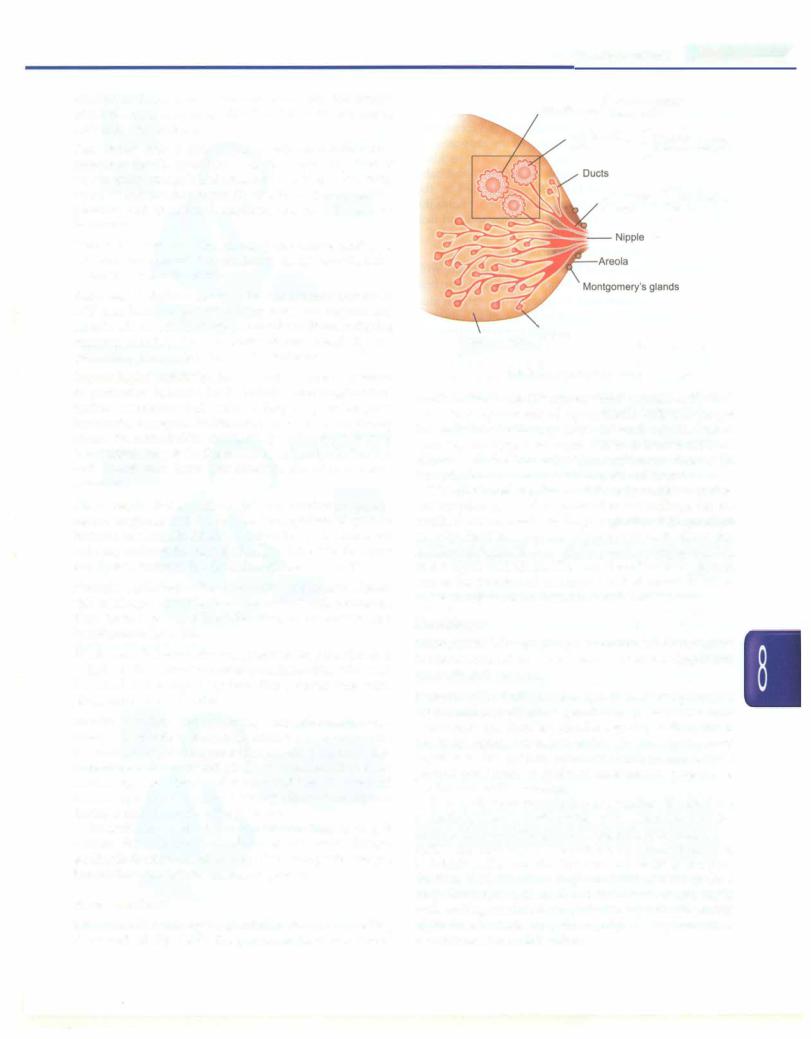
Breast Anatomy
The breast is made up of glandular tissue, supporting tissue and fat (Fig. 8.29). The glandular tissue consists of
Newborn Infants -
Muscle cells {Oxytocin makes them contract
Milk secreting |
|
Prolactin makes |
|
cells |
|
{ them secrete milk |
|
|
Lactiferous |
Milk collects |
|
|
sinuses |
|
{ here |
Support.1ng t·issue Alveoli and fat
Fig. 8.29: Anatomy of breast
small clusters of sac-like spaces which produce milk. Each sac is lined by network of myoepithelial cells that propel the milk into lactiferous ducts towards nipple. Before reaching the nipple, the ducts widen to form lactiferous sinuses which store milk. The lactiferous sinuses lie beneath the junction of areola and rest of breast.
The areola and nipples are extremely sensitive as they are supplied by a rich network of nerve endings. On the areola there are small swellings of glands which produce an oily fluid to keep the nipple skin soft. Since the lactiferous sinuses lie beneath the areola, a baby must suck at the nipple and areola. The gum line of the baby should rest at the junction of areola and rest of breast tissue in order to express milk stored in lactiferous sinuses.
Physiology
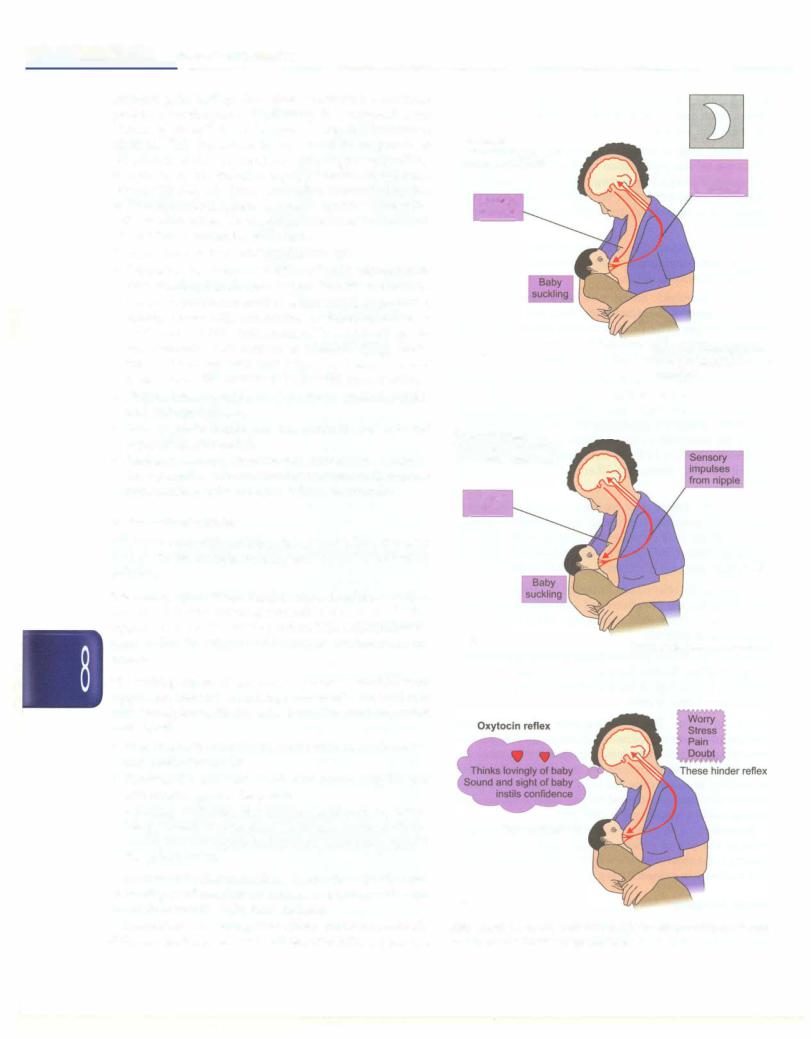
Lactogenesis is a complex phenomenon involving many hormones and reflexes. Twohormones are most important, prolactin and oxytocin.
Prolactin reflex (milk secretion reflex). Prolactin produced by the anterior pituitary gland is responsible for milk secretion by the alveolar epithelial cells (Fig. 8.30A). When the baby sucks, the nerve ending in the nipple carry impulse to the anterior pituitary which in turn release prolactin and that acts on the alveolar glands in the breast to stimulate milk secretion.
This cycle from stimulation to secretion is called the prolactin reflex or the milk secretion reflex. The more the baby sucks at the breast, the greater is the milk production. The earlier the baby is put to the breast, the sooner this reflex is initiated. The greater the demand more is the pro duction. It is, therefore, important for mothers to feed early, frequently and empty out the breasts completely at each feeding session. Since prolactin is produced during night time, breastfeeding during night is very important for maintenance of this reflex.
__E s s e n tia P e d i atrics_________________________________
_ _ _ _ _ _ _ _ _ _ _ _ _ _ _
Oxytocin reflex (milk ejection reflex). Oxytocin is a hormone
produced by the posterior pituitary. It is responsible for ejection of the milk from the glands into the lactiferous sinuses. This hormone is produced in response to stimulation to the nerve endings in the nipple by suckling as well as by the thought, sight, or sound of the baby (Figs 8.308 and C). Since this reflex is affected by the mother's emotions, a relaxed, confident attitude helps the milk ejection reflex. On the other hand, tension and lack of confidence hinder the milk flow.
Factors which reduce milk production are:
•Dummies, pacifiers and bottles not only interfere with breastfeeding but also predispose the baby to diarrhea.
•Giving supplements such as sugar water, gripe water,
honey, breast milk substitutes or formula, either as prelacteal (before initiation of breastfeeding) or supplemental (concurrent to breastfeeding) feeds. Studies have reported that even 1 or 2 supplemental feeds reduce the chances of successful breastfeeding.
•Painful breast conditions like sore or cracked nipples and engorged breast.
•Lack of night feeding, as the prolactin reflex is not adequately stimulated.
•Inadequate emptying of breast such as when baby is sick or small andthe mother does not manually express breast milk or when baby is fed less frequently.
Reflexes in the Baby
A baby is born with certain reflexes which help the baby to feed. These include rooting, sucking and swallowing reflexes.
The rooting reflex. When cheek or the side of the mouth is touched, the baby opens her mouth and searches for the nipple. This is called rooting reflex. This reflex helps the baby to find the nipple and in proper attachment to the breast.
The suckling reflex. When baby's palate is touched with nipple, the baby starts sucking movements. This reflex is very strong immediately after birth. The sucking reflex consists of:
•Drawing in the nipple and areola to form an elongated teat inside the mouth.
•Pressing the stretched nipple and areola with the jaw and tongue against the palate.
•Drawing milk from the lactiferous sinuses by wave like peristalticmovement of the tongue underneath the areola and the nipple and compressing them against the palate above.
To suckle effectively, the baby has to attach (latch) well. Obtaining good attachment at breast is a skill, which both the mother and the baby have to learn.
The method of suckling at the breast andbottle is entirely different. Suckling on a bottle filled with milk is a passive
Prolactin
Secreted after feed to
produce next feed Sensory impulses from niP.P.le
Prolaclin in blood
A |
Prolactin: secreted more |
|
at night; suppresses |
||
|
||
|
ovulation |
Oxytocin reflex
Works before or during feed to make milk flow
Oxytocin in blood
B |
Oxytocin makes uterus contract |
|
These help reflex
C
Figs 8.30A to C: (A) Prolactin and (B) oxytocin reflex; (C) factors which help and hinder oxytocin reflex
process and the baby has to control the flow of milk into the mouth with her tongue. While breastfeeding requires active efforts by the baby. A bottlefed baby develops nipple confusion and refuses to feed on the breast. Single session of bottlefeeding lessens the chances of successful breast feeding. Bottle feeding of babies is fraught with risk of serious infections and consequent ill health.
The swallowing reflex. When the mouth is filled with milk, the baby reflexly swallows the milk. It requires a couple of suckles before baby can get enough milk to trigger swallowing reflex. It requirescoordination with breathing. The suckle-swallow-breathe cycle lasts for about one second.
Composition of Breast Milk
The composition of breast milk varies at different time points of lactation to suit the needs of the baby. Milk of a mother who hasdeliveredapreterm baby isdifferentfrom milk of a mother delivered a term baby.
i.Colostrum is the milk secreted during the initial 3--4 days after delivery. It is small in quantity, yellow and thick and contains large amount of antibodies and immune-competant cells and vitamins A, D, E and K.
ii.Transitional milk is the milk secreted after 3-4 days until two weeks. The immunoglobulin and protein content decreases while the fat and sugar content increases.
iii.Mature milkfollows transitional milk. It is thinner and watery but contains all the nutrients essential for optimal growth of the baby.
iv.Preterm milk is the milk of a mother who delivers before 37 week. It contains more proteins, sodium, iron, immunoglobulins and calories as per the requirement of preterm baby.
v.Foremilk is the milk secreted at the start of a feed. It is watery and is rich in proteins, sugar, vitamins, minerals and water that quenches the baby's thirst.
vi.Hindmilk comes later towards the end of feed and is richer in fat that provides more energy and gives a sense of satiety. Thus, the composition of milk also varies during the phase of feeding. For optimum growth, the baby needs both fore as well as hind milk. Therefore, the baby should be allowed to empty out one breast completely before switching over to the other.
Technique of Breastfeeding
Mothers require substantial assistance to learn the technique of breastfeeding. With correct technique, breastfeeding is natural and a pleasurable experience for the mother. However a variety of breastfeeding problems do occur in large proportion of mothers that require counselingand supportfromthehealthprovidersfortheir prevention and appropriate treatment. Provision of lactation support services by lactational counsellor or
Newborn Infants -
trained health providers greatly increase the success of breastfeeding.
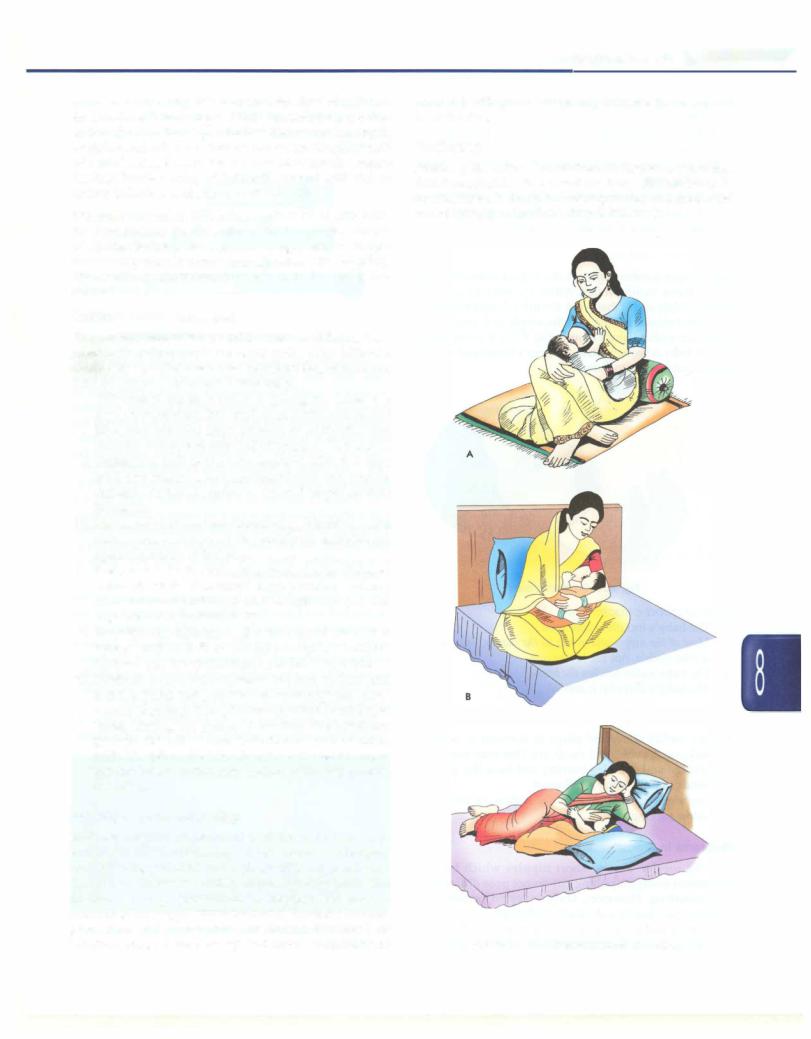
Positioning
Position ofthe mother. The mother can assume any position that is comfortable to her and the baby. She can sit or lie down. Her back should be well supported and she should not be leaning on her baby (Figs 8.31A to C).
C
Figs 8.31A to C: Different postures of feeding
__E_s_s_e_n_ti_a _l _P_e _d_ia_t_ri_cs _______________________________
Position of baby. Make sure that baby is wrapped properly in a cloth
i.Baby's whole body is supported not just neck or shoulders
ii.Baby's head and body are in one line without any twist in the neck
iii.Baby's body turned towards the mother (abdomens of the baby and the mother touching each other)
iv.Baby's nose is at the level of the nipple.
Attachment (Latching)
After proper positioning, the baby's cheek is touched and that initiates rooting reflex. Allow the baby to open his mouth widely andatthatpoint,the baby shouldbe latched on to the breast ensuring that the nipple and most of the areola are within baby's mouth (Fig. 8.32). It is important that the baby isbrought on themother'sbreast and mother should not lean on to baby.
Fig. 8.32: Good attachment
Signs of good attachment
i.The baby's mouth is wide open
ii.Most of the nipple and areola in the mouth, only upper areola visible, not the lower one
iii.The baby's chin touches the breast
iv.The baby's lower lip is everted
Effective Suckling
•Baby suckles slowly and pauses in between to swallow (suck, suck, suck.. and swallow). One may see throat cartilage and muscles moving and hear the gulping sounds of milk being swallowed.
•Baby's cheeks are full and not hollow or retracting during sucking.
Problems i n Breastfeeding
Inverted nipples. Flat or short nipples which become prominent easily on pulling out do not pose difficulty in breastfeeding. However, truly inverted or retracted nipples make latching difficult. As the baby is not able to take nipple and areola in the mouth properly, sucking on the nipples makes themsoreand excoriated. Treatment is
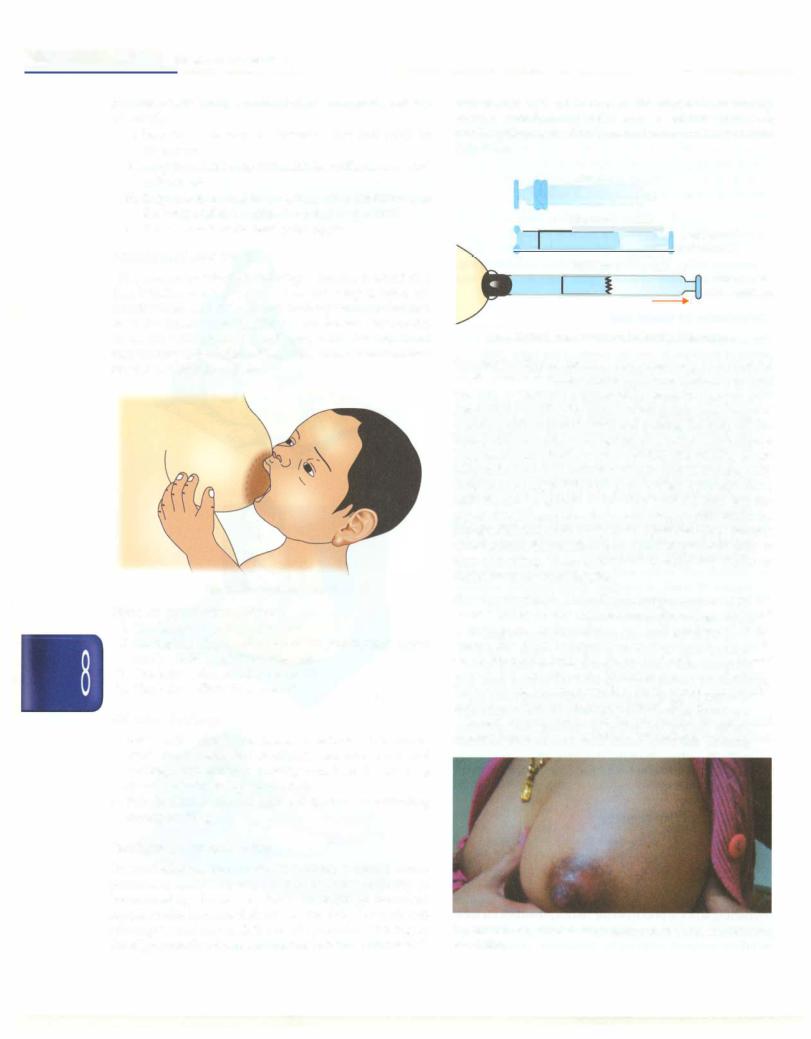
started after birth of the baby. The nipple is manually everted, stretched and rolled out several times a day. A plastic syringe is used to draw out to correct the problem (Fig. 8.33).
|
|
||||||
|
Step two |
! |
+--- |
|
|
|
|
|
|
'-fl |
|
||||
|
|
|
|
|
Insert piston |
||
|
|
|
+--ri.J |
||||
|
from cut end |
||||||
|
Step three |
||||||
|
__.. |
|
|||||
|
|
|
|
|
|
|
Mother gently |
|
|
|
|
|
|
|
pulls the piston |
Fig. 8.33: Syringe treatment for inverted/flat nipple
Sore nipple. Nipples become sore when baby suckles on the nipple rather than areola because of incorrect attachment. As the baby is unable to express milk, he sucks vigorously in frustration and bites the nipple causing soreness. Frequent washing with soap and water and pulling the baby off the breastwhileheis still suckingmay alsoresult insorenipple. Treatment consists of correct positioning and latching of the babyto thebreast. A motherwouldbe ableto feed the baby despite sore nipple if the baby is attached properly. Hind milk should be applied to the nipple after a feed and the nippleshouldbeairedandallowedtoheal inbetweenfeeds. Sheshouldbeadvised nottowash nippleeachtimebefore/ after feeding. She can clean breast and nipple once daily at time of bathing. There is no need to apply any cream or ointment to the sore nipples.
Breast engorgement. The milk production increases by the second and third day after delivery. If feeding is delayed or infrequent, or the baby is not well positioned at the breast, the milk accumulates in the alveoli. As milk production increases, the amount of milk in the breast exceeds the capacity of the alveoli to store it comfortably. Such a breast becomes swollen, hard, warm and painful and is termed as an 'engorged breast' (Fig. 8.34).
Breast engorgement can be prevented by early and frequent feeds and correct attachment ofthebabytothebreast.
Fig. 8.34: Engorged breast. Note tense and shiny skin; nipple shows excoriation
