
Ghai Essential Pediatrics8th
.pdf
Post-term neonate. A neonate born at a gestation age of 42 weeks or more (294 days or more).
Low birthweight (LBW) neonate. A neonate weighing less than 2500 g at birth irrespective of the gestational age.
Very low birthweight (VLBW) neonate. A neonate weighing lessthan 1500 g at birth irrespective of the gestational age.
Extremely low birthweight (ELBW) neonate. A neonate weighing less than 1000 g at birth irrespective of the gestational age.
Neonatal mortality rate (NMR). Deaths of infants under the first 28 days of life per 1000 live births per year.
Perinatal mortality ratio (PNMR). Number of perinatal deaths (stillbirths plus neonatal deaths before 7 days of life) per 1000 live births. It is designated as a ratio since the numerator is not part of the denominator. (For rate, like in NMR, numerator is part of denominator.)
Online Learning Resource Material
The Newborn Division of Department of Pediatrics, AllvlS, has produced excellent resource material for learning of health professionals. The material is in form of modules, posters, videos and webinars on common newborn issues and is available at: www.newbornwhocc.org.
The online material complements the information provided in this Chapter. The readers are encouraged to visit the website and use the resource to enhance their learning.
RESUSCITATION OF A NEWBORN
Of the 25 million infants born every year in India, 3-5% experience asphyxia at birth. Asphyxia is characterized by progressive hypoxia, hypercapnia, hypoperfusion and acidosis. It may lead to multiorgan dysfunction that may cause death. Hypoxic ischemic encephalopathy (HIE) resulting from asphyxia may lead to longterm neuromo tor sequelae.
There is broad consensus on the evidence based resuscitation of newborn babies at birth. The American Heart Association (AHA) and the American Academy of Pediatrics (AAP) have recently updated the resuscitation guidelines that are being propagated worldwide through the NeonatalResuscitation Program (NRP). A summary of therecommendationsof AHA-AAP (2010)isprovidedhere.
Pathophysiology of Asphyxia
When an infant is deprived of oxygen, an initial brief periodof rapidbreathingoccurs.Ifthe asphyxiacontinues, the respiratorymovements cease andthe infant enters into a period of apnea known as primary apnea. During primary apnea, the heart rate begins to fall, neuromuscular tone gradually diminishes but the blood pressure remains normal. In most instances, tactile stimulation during this period will reinitiate respiration.
Newborn Infants -
If the asphyxia continues, the infant develops deep gasping respiration, the heart rate continues to decrease, the blood pressure begins to fall and the infant becomes flacid. The breathing becomes weaker until the infant gaspsandenters into a periodof secondary apnea. Theinfant is now unresponsive to stimulation and does not spontaneouslyresume respiratory efforts unless resuscita tion in the form of positive pressure ventilation isinitiated.
It is important to note that as a result of fetal hypoxia, the infant may go through the phases of primary and secondaryapneaeven in utero. Hence, apnea at birth may be either primary or secondary apnea. These two are clinically indistinguishable; in both instances, the infant is not breathing and the heart rate may be below 100 beats per minute. Hence, when faced with an apneic infant at birth, one should assume that one is dealing with secondary apnea and be ready to undertake full resusci tation efficiently without wasting too much of time in providing tectile stimulation.
Lung Inflation
During intrauterine life, the lungs do not take part in gas exchange,which is taken care ofby theplacenta. The lung alveoli in the fetus are filled with fluid secreted by type II alveolar cells. The process of fluid removal starts with onset of labor. The fluid gets reabsorbed from the alveoli into the perivascular space and then into blood and lymphatic channels. The process of labor may facilitate removal of lung fluid, whereas removal is slowed when labor is absent (as in elective cesarean section).
Removal of lung fluid from the alveoli is facilitated by respiration soon after birth.The first few breaths after birth are effective in expanding the alveoli and replacing the lung fluid with air. Problems in clearing lung fluid may occur in infants whose lungs have not inflated well with the first few breaths, such as those who are apneic at birth or have a weak initial respiratory effort as with prema turity or sedation.
Pulmonary Circulation
Oxygenation depends not only on air reaching the alveoli, but also on pulmonary circulation. During intrauterine life,there islittle blood flow in the lungs due to pulmonary vasoconstriction. After birth, pulmonary vasodilatation takes place resulting in fall in pulmonary vascular resistance and increased blood flow in the pulmonary circuit.
An asphyxiated infant has hypoxemia (low-oxygen content of the blood) and acidosis (low pH). In the presence of hypoxemia and acidosis, the pulmonary arterioles remain constricted and ductus arteriosus remains open (persistence of fetal circulation). As long as there is poor pulmonary blood flow, proper oxy genation of the tissues of the body is impossible because there is inadequate uptake of oxygen, even when the infant is being properly ventilated.
_ |
E ss entia1Pe diatrics------------------------------ |
-- |
|
|
In mildly asphyxiated babies whose oxygen and pH are only slightly lowered, it may be possible to increase pulmonary blood flow by quickly restoring ventilation. However, pulmonary perfusion in severely asphyxiated infants may not improve with ventilation alone. The combination of oxygenation and correction of metabolic acidosis would be necessary to open the pulmonary arterioles that would improve pulmonary blood flow.
Cardiac Function and Systemic Circulation
Inasphyxia,thereisredistributionofbloodflowtopreserve blood supply to vital organs. There is vasoconstriction in thebowel,kidney,musclesandskin,thuspreservingblood flow to the heart and brain (diving-in reflex).
As asphyxia is prolonged, myocardial function and cardiac output too deteriorate and blood flow toall organs is further reduced. This sets in the stage for progressive organ damage. At this point, it maybe necessary to provide cardiac stimulants (epinephrine) and volume expanders (normal saline) to support the heart and circulation.
Preparing for Resuscitation
Withcarefulconsiderationof antepartum andintrapartum risk factors, asphyxia can be anticipated in up to only half of the newborns who will eventually require some form of resuscitation. In others, the need for resuscitation can come as a complete surprise. Therefore, each delivery should be viewed as an emergency and basic readiness must be ensured to manage asphyxia. Preparation for delivery should include:
i.A radiant heat source ready for use
ii.All resuscitation equipments immediately available and in working order (Table 8.1)
iii.At least one person skilled in neonatal resuscitation
Evaluation
Evaluationis basedprimarily on the following three signs: respiration, heart rate (HR) and color. Though all three signs are evaluated simultaneously, low heart rate is the most important sign for proceeding to the next step.
Role of Apgar Scores in Resuscitation
The Apgar score is an objective method of evaluating the newborn's condition (Table 8.2). It is generally performed at 1 minute and again at 5 minutes after birth. However, resuscitation must be initiated before the 1-minute score
Table 8.1: Neonatal resuscitation supplies and equipment Suction equipment
Mechanical suction
Suction catheters 10, 12 or 14 F
Meconium aspirator
Bag and mask equipment
Neonatal resuscitation bags (self-inflating)
Face-masks (for both term and preterm babies)
Oxygen with flow meter and tubing
Intubation equipment
Laryngoscope with straight blades no. 0 (preterm) and no. 1 (term)
Extra bulbs and batteries (for laryngoscope)
Endotracheal tubes (internal diameter of 2.5, 3.0, 3.5 and 4.0 mm)
Medications
Epinephrine
Normal saline or Ringer lactate
Naloxone hydrochloride
Miscellaneous
Linen, shoulder roll, gauze
Radiant warmer
Stethoscope
Syringes 1, 2, 5, 10, 20, 50 ml
Feeding tube 6 F
Umbilical catheters 3.5, 5 F
Three way stopcocks
Gloves
is assigned. Therefore, the Apgar score is not used to guide the resuscitation.
While the Apgar score is not useful for decision making at the beginning of resuscitation, the change of score at sequentialtime points following birth canreflecthow well the baby is responding to resuscitative efforts. Hence, Apgar scores should be obtained every 5 minutes for up to 20 minutes, if the 5-minute Apgar score is less than 7.
TABC of Resuscitation
The components of the neonatal resuscitation procedure related to the TABC of resuscitation are shown here:
T-Temperature: Provide warmth, dry the baby and remove the wet linen.
A-Airway: Position the infant, clear the airway (wipe baby's mouth and nose or suction mouth, nose and in
|
|
Table 8.2: Apgar score |
|
Sign |
0 |
1 |
2 |
Heart rate |
Absent |
Slow (<100 beats/min) |
Normal (>100 beats/min) |
Respiration |
Absent |
Weak cry |
Good strong cry |
Muscle tone |
Limp |
Some flexion |
Active movements |
Reflex irritability |
No response |
Grimace |
Cough or sneeze |
Color |
Blue or pale |
Body pink, extremities blue |
Completely pink |
Newborn Infants -
some instances, the trachea in non-vigorous baby born through meconium stained liqor). If necessary, insert an endotracheal (ET) tube to ensure an open airway.
B-Breathing: Tactile stimulation to initiate respirations, positive-pressure breaths using either bag and mask or bag and ET tube when necessary.
C-Circulation: Stimulate and maintain the circulation of blood with chest compressions and medications as indicated.
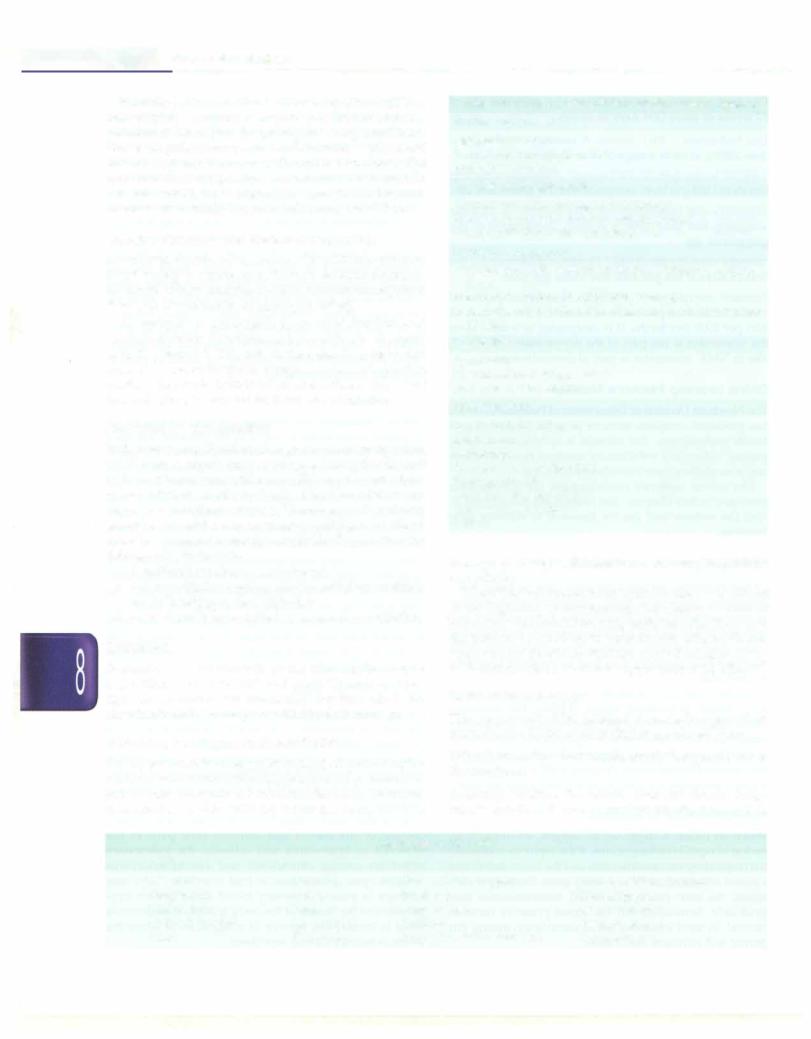
Resuscitation Algorithm
Figure 8.2presentsthe algorithmof neonatalresuscitation. At the time of birth, one should ask three questions about the newborn:
i.Term gestation?
ii.Breathing or crying?
iii.Good muscle tone? (flexed posture and active movement of baby denotes good tone)
If answers to all the three questions are 'Yes', the baby does not require any active resuscitation and "Routine care" should be provided. Routine care consists of four steps:
i. Warmth: Provided by putting the baby directly on the mother's chest in skin-to-skin contact.
ii. Clearingofairway ifrequired: Done bywipingthe baby's
mouthand noseusing a clean cloth. No needto suction routinely.
iii.Dry the baby
iv.Ongoing evaluation for vital parameters. Helping mother in breastfeeding will facilitate easy transition to extrauterine environment.
If answer to any of the three questions is "No", the baby requires resuscitation. After cutting the cord, the baby should be subjected to a set of interventions known as
Initial steps.
BirthI |
|
|
|
|
|
|
|
|
|
|
|
|
Rout ne c e |
|
|
|
|
|
|||
|
|
|
Term gestation? |
|
Yes |
|
|
|
Providewarmth |
|
Assessment |
||||||||||
I |
|
|
|
Breathing or crying? |
|
|
|
|
|
|
Clear airway, if necessary |
|
|||||||||
I |
|
|
|
Good tone? |
|
|
|
|
|
Dry |
|
|
|
|
|
|
|
|
|||
I |
|
|
|
|
|
|
|
|
|
|
|
|
Keep with mother |
|
|
||||||
I |
|
|
|
No |
|
|
|
|
|
|
|
|
Ongoing evaluation |
|
|
||||||
I |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
I |
|
Provide warmth, clear airway |
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
I |
|
|
if necessary, dry, stimulate |
|
|
|
|
|
|
|
r |
No |
|
|
|||||||
I |
|
|
|
|
|
|
|
|
|
|
|
||||||||||
I |
|
|
|
Heart rate below 100, |
|
No |
|
|
|
|
|
|
|
|
|
|
|||||
I |
|
|
|
|
|
|
|
,"Labored breathing |
|
|
|||||||||||
I |
|
|
|
|
|
|
|
|
Evaluation |
||||||||||||
30 sec |
|
|
|
gasping or apnea? |
|
|
|
|
|
pe2!.stent cyanosis? |
|
|
|
||||||||
I |
|
|
|
|
|
|
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
||||||||||||
I |
|
|
|
Yes |
1 |
|
|
|
|
|
|
|
|
|
|
Yes |
|
|
|||
I |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||||||
I |
|
|
|
|
|
|
|
|
Clear airway, SpO, monitoring |
|
|
||||||||||
I |
|
|
Positive pressure ventilation |
|
|
] |
|||||||||||||||
I |
|
|
|
|
|
|
|
|
Co |
erCPAP |
|||||||||||
60 sec |
[ |
|
SpO, monitoring |
] |
|
|
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|||||||||||||
|
|
|
|
|
! |
|
|
|
No |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
1Heart rate below 100?1 |
|
|
|
|
|
|
|
|
|
|
|
|
|
Evaluation |
||||
|
|
|
|
Yes |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
[ Take ven ective step7") |
|
|
|
|
|
|
|
|
|
|
|
|
||||||||
|
|
|
|
|
|
care |
|
|
|||||||||||||
|
|
|
|
_! |
|
|
|
|
|
|
|
|
|
|
|
||||||
|
|
|
|
Heart rate below 60? |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
|
|
|
Yes!___ - |
::i |
|
|
|
|
|
|
|
|
|
|
|
|
||||
|
r-- |
|
ChestConsidercompressionsintubation |
|
|
|
|
|
|
|
|
|
|
|
|
||||||
|
Coordinate with positive pressure ventilation |
|
|
|
Targeted SpO,after birth |
|
|
||||||||||||||
|
|
|
|
|
! |
|
|
|
|
|
|
|
|
|
|||||||
|
|
|
L!:!.eart rate below 60?J |
|
|
|
|
|
1 minute: 60-65% |
|
|
||||||||||
|
|
|
|
|
|
|
|
2 minutes: 65-70% |
|
Evaluation |
|||||||||||
|
|
|
|
Yesu |
|
|
|
|
|
3 minutes: 70-75% |
|
||||||||||
|
|
|
|
|
|
|
|
|
4 minutes: 75-80% |
|
|
||||||||||
|
|
|
|
IV epinephrine |
|
|
|
|
|
5 minutes: 80-85% |
|
|
|||||||||
|
|
|
|
|
|
|
10 minutes: 85-95% |
|
|
||||||||||||
The algorithm of neonatal resuscitation. CPAP continuous positive airwaypressure; PPV positive ventilation; Sp02 saturation of oxygen. (AdaptedFig. 8.2: with permission from American Academy of Pediatrics 2010)

|
|
n il |
i |
i |
|
|
_______ |
|
Esse__ta Ped__a_tr-cs |
______________ |
_ |
||||
|
__ |
|
|
|
___________ |
|
|
|
|
|
|
|
|
||
InitialSteps
Warmth
The baby should be placed under the heat source, preferably a radiant warmer. The baby should not be covered with blanketsortowels to ensurefull visualization and to permit the radiant heat to reach the baby.
Positioning
The baby should be placed on her back or side with the neck slightly extended. This brings the posterior pharynx, larynx and trachea in line and facilitates breathing. Care should be taken to prevent hyperextension or flexion of the neck, since either may interfere with respiration.
To help maintain the correct position, place a rolled blanket or towel under the shoulders, elevating them % or 1 inch off the mattress. This shoulder roll is particularly helpful if the infant has a large occiput resulting from molding, edema, or prematurity (Fig. 8.3).
5--
Fig. 8.3: Rolled towel under the shoulders
Clear Airway if Necessary
The appropriate method for clearing the airway will depend on the presence or absence of meconium.
If no meconium is present, secretion may be removed from theairwaybywipingthe noseandmouthwithaclean cloth or by suctioning with a bulb syringe or suction catheter. The mouth is suctioned before nose ('M' before 'N') to ensure the infant does not aspirate, if she should gasp when the nose is suctioned. If the infant has copious secretion from the mouth, the head should be turned to the side. This will allow secretions to collect in the side of mouth, where they can be easily removed.
For suctioning, the size of suction catheter should be 12 or 14 Fr. The suction pressure should be kept around 80 mm Hg (100 cm water) and should not exceed 100 mm Hg (130 cm water). One should not insert the catheter too deepin mouth ornoseforsuctionasstimulationof posterior pharynx can produce vagal response resulting in brady cardia or apnea. The maximum time limit for suctioning is 15 seconds.
Clearing of the airways in babies born through meconium stained liquor is discussed later.
Dry, Stimulate and Reposition
After suctioning, the baby should be dried adequately usingpre-warmedlinentopreventheat loss. The wet linen should be removed away from the baby. The act of suctioning and drying itself provides enough stimulation toinitiatebreathing.If the newborncontinuestohavepoor respiratory efforts, additional tactile stimulation in form of flicking the soles or rubbing the back gently may be provided briefly to stimulate the breathing. However, one should not waste too much of time in providing tactile stimulation.
Management o f Infant Born Through
Meconium-taS inedLiquor(MSL)
When baby passes meconium in utero, meconium may be aspirated into infant's mouth and potentially into the trachea and lungs. Steps must be taken after delivery to reduce serious consequences of aspiration of meconium (Fig. 8.4). (Note: Intrapartum suctioning of the mouth and nose after delivery of the head and before delivering the shoulders is no longer recommended).
No need for lntrapartum suction
Birth: assess heart rate, breathing and tone
|
|
Vigorous: |
Heart |
Non-vigorous: |
|
||
Heart rate 100/min or more, |
|
rate<100/min or weak/no |
|||||
strong respiratory efforts and |
respiratory efforts |
or |
poor |
||||
|
|
|
|
|
|||
|
good muscle tone |
|
muscle tone |
|
|||
|
Only initial steps |
|
Tracheal suction; |
||||
|
|
|
|
|
repeat if necessary |
||
|
|
|
|
|
|||
Fig 8.4: Management of a babyborn through meconium stained liquor
After delivery, the first step is to identify whether the infant is vigorous or non-vigorous. A newborn infant is classified as vigorous if he has all the three signs namely strong respiratory efforts, good muscle tone and a heart rate greater than 100/min. Absence of any sign would imply a non-vigorous baby.
The vigorous baby does not require any tracheal suctioning and the routine care or initial steps are provided.
For non-vigorous babies, the initial steps are modified as below:
•Place the baby under radiant warmer. Postpone drying and suctioning to prevent stimulation.
•Remove the residual meconium in the mouth and posterior pharynx by suctioning under direct vision using a laryngoscope.
•Intubate and suction out meconium from the lower
airway.
Tracheal suctioning is best done by applying suction directlyto the endotracheal tube (ET). Continuous suction is applied to the ET tube as it is withdrawn. Tracheal suctioning can be repeated if the previous suctioning has
revealedmeconiumandbabyhasnotdevelopedsignificant bradycardia.
Evaluation
Afterprovidinginitial steps, the baby should beevaluated by assessing respiration, HR and color (or oxygen saturation by pulse oximetry).
Respiration is evaluated by observing the infant's chest movements. HR can be assessed by auscultating the heart or by palpating the umbilical cord pulsation for 6 seconds. The number of beats or pulsation is multiplied by 10 to obtain the HR per minute (e.g. a count of 12 in 6 seconds is a HR of 120 per minute). Color is evaluated by looking at tongue, mucous membranes and trunk. A blue hue to the lips, tongue and central trunk indicates central cyanosis. Presence of cyanosis inextremities (acrocyanosis) does not have any significance.
•If the baby has good breathing, HR 100/min or more and no cyanosis, then she does not require any addi tional intervention and the baby should be monitored frequently.
•If the baby has labored breathing or persistent central cyanosis,administration of CPAP in pretermbabiesand supplemental oxygen in term babies is recommended. Baby should have its oxygen saturation monitored and supplemental oxygen is titrated to achieve the targeted saturations (Fig. 8.2).
•If the baby is apneic, has gasping breathing or heart rate is below 100 min, positive pressure ventilation (PPV) is needed.
Supplemental Oxygen
Central cyanosisrequiressupplementaloxygen, which can be provided by an oxygen mask or oxygen tube held in cupped hand over baby's face or by flow inflating bag and mask. The flow of oxygen should be at least 5 1/ minute. Supplemental oxygen cannot be provided by self inflating bags.
Positive Pressure Ventilation (PPV)
PPV is usually given by using a self-inflating bag and face mask (bag and mask ventilation or BMV). The self inflating bag is easy to use as it reinflates completely without any external compressed source of gas. The disadvantage of such bag is that it cannot be used to administer free-flow of oxygen.
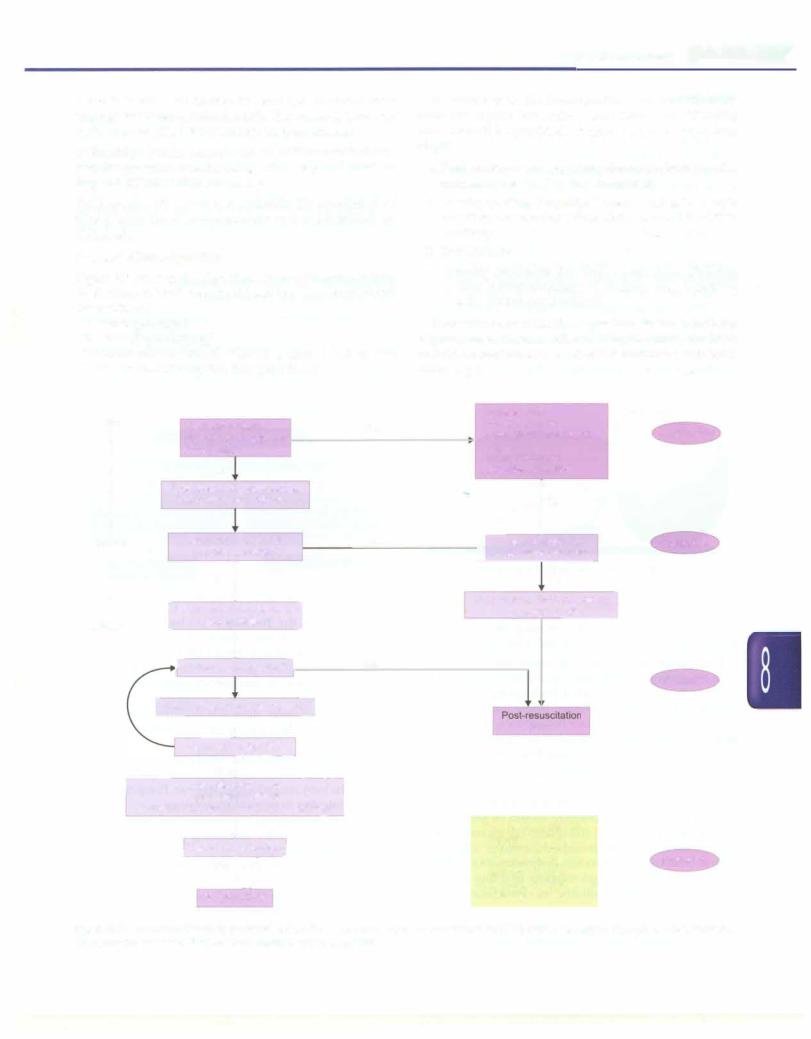
The resuscitation bag (Fig. 8.5) should have a capacity of 240 to 750 ml. If the bag is attached to an oxygen source (at 5-6 liter/min) and a reservoir, it delivers 90-100% oxygen. In absence of reservoir, it delivers 40% to 50% oxygen.
Oxygen should be treated as a drug. Both too little or too much of oxygen is bad for the baby. Even a brief exposure to high concentration of oxygen can have detrimental effect on the baby. Studies have shown that
Newborn Infants -
Oxygen |
Pressure gauge |
|
Pressure release (pop-off) valve
Valve assembly
Patient outlet Fig. 8.5: Self-inflating bag
(Adapted with premission from AAP 2005)
term babies resuscitated with room air compared to 100% oxygen have better survival and longterm outcomes. The evidence in favor or against the use of oxygen in preterm babies is yet lacking.
It is therefore recommended that term babies should be initiated on room air resuscitation. Ideally, oxygen satu ration shouldbe monitoredby pulse oxirnetry and oxygen delivery should be titrated to maintain the oxygen satura tion in the targeted range (Fig 8.2). In absence of pulse oxirnetry, room air should be substituted by 100% oxygen if the baby fails to improve (improvement in HR and breathing) by 90 seconds.
PPV in preterm babies is recommended using inter mediateconcentration of oxygen (30%to 60%). The oxygen concentration should be titrated by continuously moni toring of oxygen saturation by pulse oximetry. BMV is indicated if:
i.The infant is apneic or gasping
ii.HR is less than 100 beats per minute
iii.Persistent central cyanosis despite administration of 100% free flow oxygen
In suspected or confirmed diaphragmatic hernia, bag and mask ventilation is contraindicated. Similarly, in non vigorous babies born through MSL, bag and mask venti lation is carried out only after tracheal suctioning.
Procedure
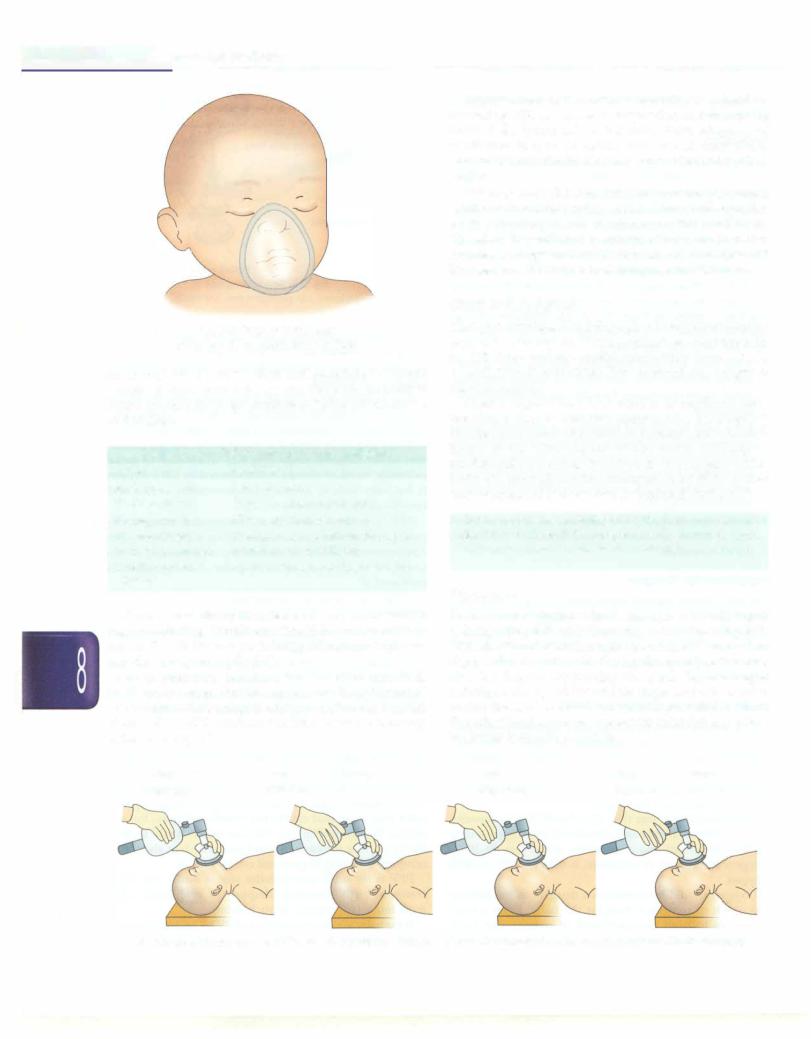
The infant's neck should be slightly extended to ensure an open airway. The care provider should be positioned at headendoratthesideofbabysoastohaveanunobstructed view of infant's chest and abdomen. Select an appropriate sized face mask that covers the mouth and nose, but not eyes of the infant (Fig. 8.6). The face mask should be held firmly on face to obtain a good seal. The bag should be compressed using fingers and not by hands.
PPV is the single most effective step in babies who fail to breathe at birth. Ensuring adequacy of ventilation is the most important priority in such babies.
If the baby is not responding to PPV by prompt increase in HR, ventilation corrective steps are taken: observe for
. __E_s_s_e_n_ t_ia_l_P_e_d_i_a _tr_ic_s_________________________________
Fig. 8.6: Properly fitting mask (Adapted with permission from AAP 2005)
an appropriate rise of the chest and auscultate for breath sounds. If chest does not rise and there are no audible breath sounds, the steps outlines in Table 8.3 should be undertaken.
Table 8.3: Ventilation corrective steps (MRSOPA)
Action |
Condition |
Inadequate seal |
Re apply mask |
Blocked airway |
Reposition the infant's head |
Blocked airway |
Clear secretions by suction |
Blocked airway |
Ventilate with mouth slightly open |
Inadequate pressure |
Increase pressure slightly |
Consider alternate |
Blocked airway(endotracheal tube) |
airway |
|
When normal rise of the chest is observed, one should begin ventilating. Ventilation should be carried out at a rate of 40 to 60 breaths per minute, following a 'squeeze, two, three' sequence (Fig. 8.7).
Usual pressure required for the first breath is 30-40 cm of water. For subsequent breaths, pressure of 15-20 cm of waterisadequate.After theinfanthasreceived 30 seconds of PPV, evaluate the HR and take a followup action as in Fig. 8.2.
One |
Two |
Three |
(Squeeze) |
(Release |
......) |
Improvement in the infant's condition is judged by increasing HR, spontaneous respiration and improving color. If the infant fails to improve, check adequacy of ventilation in form of visible chest rise. If chest rise is inadequate, one shouldtake necessary action as described earlier.
PPV may cause abdominal distension as the gas escapes intothestomachviaesophagus.Distendedstomachpresses on the diaphragm and compromises the ventilation. Therefore, if ventilation is continued for more than two minutes,anorogastrictube (feeding tubesize6-8Fr)should be inserted and left open to decompress the abdomen.
Chest Compressions
The heart circulates blood throughout the body delivering oxygen to vital organs. When an infant becomes hypoxic, the HR slows and myocardial contractility decreases. As a result there is diminished flow of blood and oxygen to the vital organs.
Chest compressions (CC) consist of rhythmic com pression of the sternum that compress the heart against the spine, increase intrathoracic pressure and circulate blood to the vital organs of the body. CC help in mechanically pumping the blood to vital organs of the body. CC must always be accompanied by BMV so that only oxygenated blood is being circulated during CC.
Chest compressions are indicatedif HR is below 60/min even after 30 seconds of PPV. Once the HR is 60/min or more, chest compressions should be discontinued.
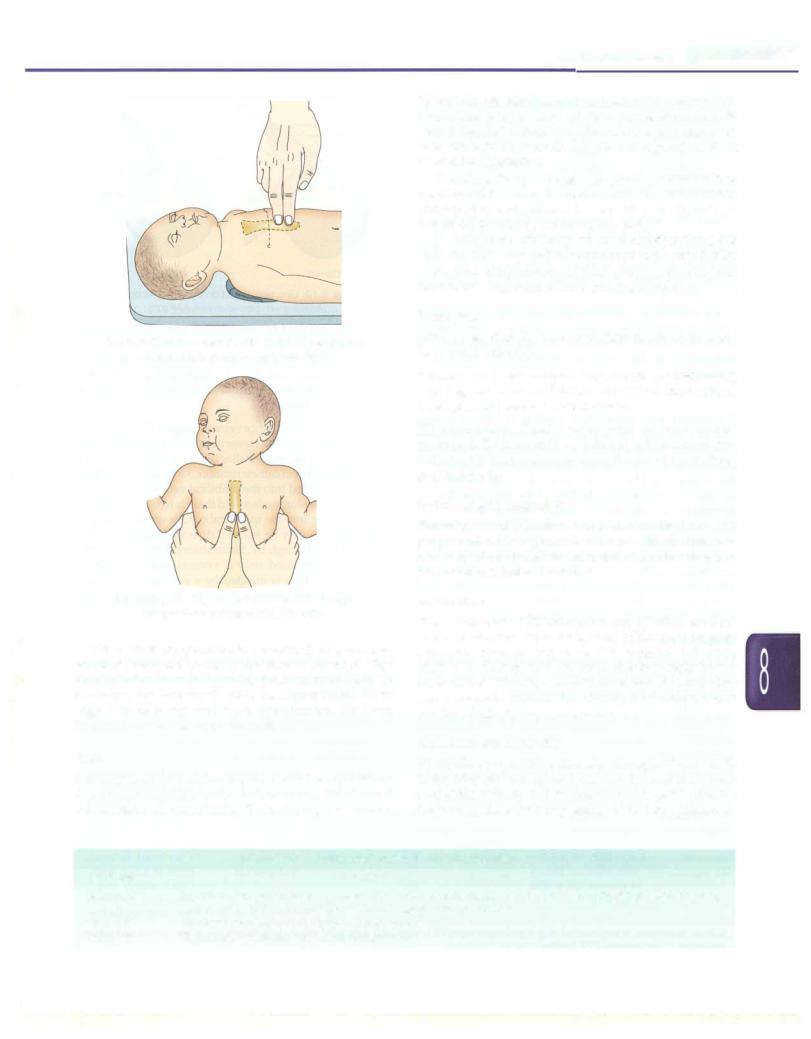
Procedure
There aretwotechniquesforchestcompressions: (i) thumb technique (Fig. 8.8), and (ii) two-fingertechnique (Fig.8.9). With the thumb technique, the two thumbs are used to depress the sternum, with the hands encircling the torso and the fingers supporting the back. In two-finger technique, the tips of the middle finger and either index or ring finger of one hand is used to depress the sternum. The otherhandis used to support the infant's back, unless the infant is on a firm surface.
One |
Two |
Three |
(Squeeze) |
(Release ...... |
) |
Fig. 8.7: Correct rhythm of providing positive pressure ventilation.(Adapted with permission from American Academy of Pediatrics 2005)
Newborn Infants -
Fig. 8.8: Chest compression with two finger technique (Adapted with permission from AAP 2005)
Fig. 8.9: Chest compression with thumb technique (Adapted with permission from AAP 2005)
When chest compression is performed on a neonate, pressure is applied to the lower third of sternum. Care must be taken to avoid applying pressure to xiphoid. To locate the area, one should slide the fingers on the lower edge of thoracic cage and locate xiphisternum. The lower third of the sternum is just above it.
Rate
It is important to ventilate between chest compressions. A positive breath should follow every third chest compression. In one minute, 90 chest compressions and
30 breaths are administered (a total of 120 events). To obtain the proper ratio of 90 compressions and 30 ventilations in1minute(3:1),chestshould be compressed three times in 1h seconds, leaving out approximately h second for ventilation.
Thumbs or the tipsoffingers (dependingonthe method used) should remain in contact with the chest during compression and release. Do not lift your thumbs or fingers off the chest between compressions.
To determine efficiency of chest compressions, the carotidorfemoralpulsationshouldbecheckedperiodically.
Possible complications of chest compressions include broken ribs, laceration of liver and pneumothorax.
Evaluation
After a period of 30 seconds of chest compressions, the heart rate is checked:
HR below 60. Chest compressions should continue along with bag and mask ventilation. In addition, medications (epinephrine) have to be administered.
HR 60 or above. Chest compressions should be dis continued. BMV should be continued until the heart rate is above 100 beats per minute and the infant is breathing spontaneously.
Endotracheal Intubation
Endotracheal (ET) intubation is required only in a small proportion of asphyxiated neonates. Intubation is a relatively difficult skill to learn and it requires frequent practice to maintain the skill.
Indications
The indications of ET intubation are: (i) when tracheal suction is required (in non-vigorous babies born through MSL), (ii) when prolonged BMV is required, (iii) when BMV is ineffective, and (iv) when diaphragmatic hernia is suspected. The other conditions where ET intubation may be considered are: beforestartingchest compressions and for administering epinephrine.
Endotracheal Tube (ET)
ET should be of uniform diameter throughout the length of the tube (and not tapered near the tip) and have vocal cord guide at the tip andcentimetermarkings. ETtube size depends on the weight or gestation of the baby (Table 8.5).
|
Table 8.4: Followup action for heart rate response |
Heart rate |
Action |
Above 100 |
If spontaneous respiration is present, discontinue ventilation gradually: provide tactile stimulation by gently |
|
rubbing the body, and monitor heart rate, respiration and color |
60 to 100 |
Continue ventilation; take ventilation corrective steps |
Below 60 |
Continue to ventilate; start chest compressions |
__E_ssen_t ialP_ed_ iatrics_________________________________
Table 8.5: Appropriate endotracheal tube size
Inner diameter |
Weight |
Gestational age |
oftube (mm) |
(g) |
(weeks) |
2.5 |
<1000 |
<28 |
3.0 |
1000-2000 |
28-34 |
3.5 |
2000-3000 |
34-38 |
|
||
4.0 |
>3000 |
>38 |
Most ET currently manufactured for neonates have a black line near the tip of the tube which is called a vocal cord guide. Such tubes are meant to be inserted so that the vocal cord guide is placed at the level of the vocal cords. This helps position the tip of ET above the bifurcation of trachea.
For intubation, a neonatal laryngoscope, with straight blades of sizes 'O' (for preterm babies) and 'l' (term babies) is required. Before intubating, the appropriate blade is attached to the handle of laryngoscope and the light is turned on.
Procedure
The infant's head should be in rnidline and the neck kept
slightly extended. The laryngoscope is held in the left hand betweenthe thumb andthefirst threefingers, with theblade
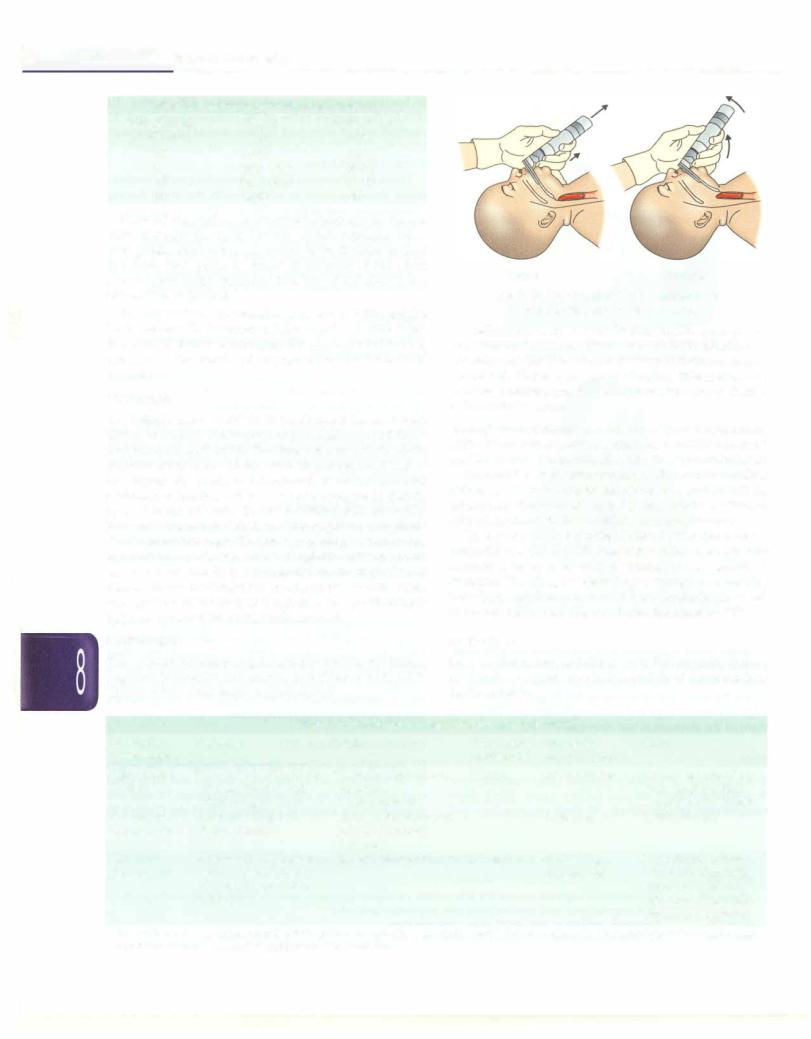
pointing away from oneself. Standing at the head end of the infant, the blade is introduced in the mouth and advanced to just beyond the base of the tongue so that its tiprests in the vallecula. Thebladeis lifted asshownin Fig.
8.10 and landmarks looked for; the epiglottis and glottis should come into view. The glottic opening is surrounded by vocal cords onthe sides. Once the glottis and vocal cords are visualized, the ET is introduced from the right side of the mouth and its tip inserted into the glottis until the vocal cord guide is at the level of the glottis, thus positioning it half way between the vocal cords and carina.
Medications
The majority of infants requiring resuscitation will have a response to prompt and effective ventilation with 100% oxygen. Only a few require medications.
Correct |
Incorrect |
Fig. 8.10: Direction of pull on the laryngoscope
(Adapted with permission from AN> 2005)
Medications used in resuscitation include epinephrine and volume expanders (Table 8.6). Sodium bicarbonate and naloxone are indicated only for special circumstances (Table 8.6). There is no role of atropine, dexamethasone, calcium, mannitol and dextrose for newborn resuscitation in the delivery room.
Routeofadministration: Sinceveins inscalporextremities are difficult to access during resuscitation, umbilical vein is the preferred route. No intracardiac injection is recommended.
Forumbilicalveincatheterization, 3.5 Fr or 5 Frumbilical catheter, is inserted into the umbilical vein such that its tip is just inside the skinsurfaceand there is free flow of blood.
Direct injection into the umbilical cord is undesirable. Epinephrine may be injected directly into the tracheo
bronchial tree through ET. Since absorption is erratic, this method is to be used only if venous access cannot be obtained. The drug is injected by a syringe or a feeding tube (5 Fr) into the endotracheal tube, flushed with 0.5 ml of normal saline and dispersed into the lungs by PPV.
Indications
Use of adrenaline is indicated if HR remains below
60 despite adequate ventilation and chest compressions for 30 seconds.
|
Table 8.6: Medications: indication, dosage and effects |
|
|||
Medication |
Indication |
Effects |
Concentration |
Dose ofthe |
Route |
(concentration) |
|
|
administered |
prepared solution |
|
Epinephrine |
HR <60/min after 30 sec |
Inotropic; chronotropic; |
1:10000 |
0.1-0.3 ml/kg |
IV; through umbilical |
(1:1000) |
of effective PPV and |
peripheral |
|
|
vein (endotracheal |
|
chest compressions |
vasoconstrictor |
|
|
route if no N access) |
Normal saline, |
Acute bleeding with |
Increased intravascular |
|
10 ml/kg |
Umbilical vein |
Ringer lactate |
hypovolemia |
volume improves |
|
|
|
|
|
perfusion |
|
|
|
Naloxone |
Respiratory depression |
Narcotic antagonist |
0.4 mg/ml |
0.25 ml/kg |
N preferred; delayed |
(0.4 mg/ml) |
with maternal history |
|
|
(0.1 mg/kg) |
onset of action with |
|
of narcotic use within |
|
|
|
intramuscular use; |
|
4 hr of birth |
|
|
|
administer only after |
|
|
|
|
|
restoring ventilation |
Sodium bicarbonate is administered only if prolonged asphyxia is associated with metabolic acidosis despite use of epinephrine and volume expanders. IV intravenous; PPV positive pressure ventilation

Suggested Reading
Kattwinkel J. Textbook of Neonatal Resuscitation. In: Kattwinkel J (ed). 6th ed. American Academy of Pediatrics and American Heart As sociation, 2010
ROUTINE CARE
Care at Birth
Personnel and equipment to be available at delivery. Onehealth provider (physician or nurse) trained in neonatal resuscitation must be physically available at time of birth of all infant irrespective of its risk status (high or low). It is not good enough to have someone on call.
If high risk delivery is anticipated because of presence of risk factors identified before birth, more advanced resuscitation may be required. In such cases, 2 persons should be present solely to manage the baby. The goal shouldbe to provide a 'resuscitationteam', with specified leaderand an identified roleofeachmember. For multiple births, there should be separate teams.
The resuscitation comer must be physically located in the delivery room itself. The health professional designated to care for the baby at birth should check for the 'Resuscitation Preparedness' at the birthing placewell in time before the baby is delivered. Details on neonatal resuscitation have been provided in the previous section.
Standard precautions and asepsis at birth. The personnel attending the delivery must exercise all the universal/ standard precautions in all cases. All fluid fromthebaby/ mothershouldbetreatedas potentiallyinfectious. Gloves, masks and gowns should be worn when resuscitating the newborn. The protective eye wear or face shields should be worn during procedures that are likely to generate droplets of blood or other body fluids.
Observe 'five cleans' to prevent sepsis at birth:
i.Clean hands: Hand-hygiene and wear sterile gloves
ii.Clean surface: Use clean and sterile towel to dry and cover the baby
iii.Clean blade: The umbilical cord to be cut with a clean and sterile blade/scissor
iv.Clean tie: The cord should be clamped with a clean and sterile clamp or tie
v.Nothing to be applied on the cord. Keep it dry.
Prevention and management of hypothermia. Immediately after birth the newborn is at high risk of hypothermia. This early hypothermia may have a detrimental effect on the health of the infant. Special care should be taken to prevent and manage hypothermia. The temperature of delivery room should be 25°C and it should be free from draft of air. The baby should be received in a pre-warmed sterile linen sheet at birth. The infant should be dried thoroughlyincludingthe headandface, and any wetlinen should not beallowed to remain incontactwiththe infant. The infant may be placed on the mother's abdomen immediately after the birth for early skin-to-skin (STS)
Newborn Infants -
contact. This will not only maintain the newborn's temperature, but also promote early breastfeeding and decreases the pain and bleeding in the mother. The baby shouldbeobservedduringthetransitionperiodand made to wear the caps and socks.
Delayed clampingofumbilical cord. Umbilical cord clamping must be delayed for 1 to 2 minutes in order to allow transfer of additional amount of blood from placenta to the infant. This delayed cord clamping in term babies is associated with improved hematologic status, iron status and clinical anemia at 2 to 6 months. In preterm infants, delayed cord clamping is associated with reduced IVH and other morbidities.
Cleaning ofbaby. The baby should be dried and cleaned at birth with a clean and sterile cloth. The cleaning should be gentle and should only wipe out the blood and the meconium and not be vigorous enough to remove the vernix caseosa (white greasy material on the skin). The vemix, protects skin of the infant and helps maintain temperature.Thisgetsabsorbedonitsownaftersometime.
Clamping ofthe cord. The umbilical cord shouldbe clamped at 2-3 cm away from the abdomen using a commercially available clamp, a clean and autoclaved thread or a sterile rubber band (Fig 8.11). The stump should be away from the genitals to avoid contamination. The cord should be inspected every 15-30 minutes during initial few hours after birth for early detection of any oozing.
Placement ofidentity band: Eachinfantmust haveanidentity band containing name of the mother, hospital registration number, gender and birth weight.
Care of Baby In the Initial Few Hours After Birth
Recording of weight. The baby should be weighed after stabilization andwhenthetemperature is documented to benormal. Asterilepre-heatedsheet (orasingleusepaper towel) should be placed on weighing machine with 10 g
Fig. 8.11: Correct application of the umbilical clamp
___E_ssen_t ialP_ed_ iatrics_________________________________
sensitivity. Electronicweighingscales areideal. Zeroingof the machine should be performed. The babyis thengently placedontheweighingmachineandtheweightisrecorded.
First examination. Thebaby shouldbethoroughlyexamined at birth from head to toe and the findings should be recorded in neonatal record sheet. Examine midline structures for malformations (e.g. cleft lip, neck masses, chest abnormality, omphalocele, meningocele, cloaca! abnormality). Special attention should be given to identify and document the patent anal opening. There is no need for routine passage of catheter in the stomach, nostrils and the rectum for detection of esophageal atresia, choanal atresia and anorectal malformation, respectively. Thebaby should be examined for presence of birth injuries. The axillarytemperature of the baby shouldbe recorded before the baby is shifted out from the birthing place.
Initiation of breastfeeding. The breastfeeding should be initiated at the earliest, but certainly within one hour of birth. The health provider should assist the mother to put the baby on breast irrespective of the mode of delivery.
Breastfeedingcounselingalone withoutproactivesupport is unlikely to result in high rates of successful breast feeding. Extra support is provided to primipara mothers and small babies.
Vitamin K. It should be administered to all the babies (0.5 mg for babies less than 1000 g and 1 mg for babies more than 1000 g). It is preferable to administer the Kl pre paration, however, if not available, vitamin K3 may be administered. Vitamin K3 can cause hemolysis in G6PD deficient babies.
Communication with the family. Before leaving the birthing place, the health professional should communicate with the mother and the family members. The following facts should be clearlytold to the family: (i) gender of the baby,
(ii) birth weight and (iii) well-being of the baby. One should ensure that the family members and the mother get to witness the gender and the identity number of the baby.
Rooming in. Under no circumstances a normal newborn should be separated from the mother. In the initial few hours of life, the baby is very active and the closeness of the baby to the mother will facilitate early breastfeeding and bonding. Studies have shown that any separation during initial hours may have a deterimental effect on successful breastfeeding.
Care of Baby Beyond Few Hours After Birth
Care of the cord. The umbilical stump should be kept dry and devoid of any application. The nappy of the baby should be folded well below the stump to avoid any contamination.
Oil massage. The benefits of oil application have been described for low birth weight babies in both developed
and developing countries. Oil massage is a low cost traditional practice that is well ingrained into the Indian culture,with noreportedadverseoutcome.The same may be allowed in a gentle way and with clean hands. Care should betaken not to use oilswithadditivesor the irritant oils (such as mustard oil) for this purpose. Coconut oil makes a good choice.
Exclusive breastfeeding. A proactive and a systematic approach should be followed to initiate, support and maintain breastfeeding. The various advantages of the breastfeeding should be discussed with the mother to motivate her. Availability of dedicated lactation nurse or counseler significantlyimproves the chances of successful breastfeeding.
Position ofsleep. Evidence has linked prone position to the occurrence of sudden infant death syndrome (SIDS). All healthy term newborns should be put to sleep on their back (supine position).
Traditional practices that should be discouraged. The applicationof kajal or surma in the eyes, putting oilin the ear or applying cow-dung on cord must be strongly discouraged.
Timing of discharge in a normal newborn. A normal baby should stay in the healthfacility for at least 24 hr. Smaller babies or those with feeding problems or sickness should remain in hospital as required.
The following criteria should be met in all the babies prior to discharge:
•The routine formal examination of the newborn has been performed and documented
•The newborn is breastfeeding properly. The adequacy of feeds can be determined by:
-Passage of urine 6 to 8 times every 24 hr
-Baby sleeping well for 2-3 hr after feeds
•The newborn has received the immunization as per schedule
•The mother is confident and trained to take care of the neonate
•The newborn is not having significant jaundice or any other illness requiring closer observation by a health provider
•The mother has been counseled regarding routine newborn care and her queries are answered
•Followup advice should be communicated to the mother. Babies, particularly born to primigravida mothers should be called for followup visit at 48 hr of discharge if discharged before 48 hr
•Parents have been explained the following 'danger signs'when they need to bring the babyto the hospital:
i.Difficulty in feeding
ii.Convulsion
iii.Lethargy (movement only when stimulated)
iv.Fast breathing (RR >60/min)
