
Ghai Essential Pediatrics8th
.pdf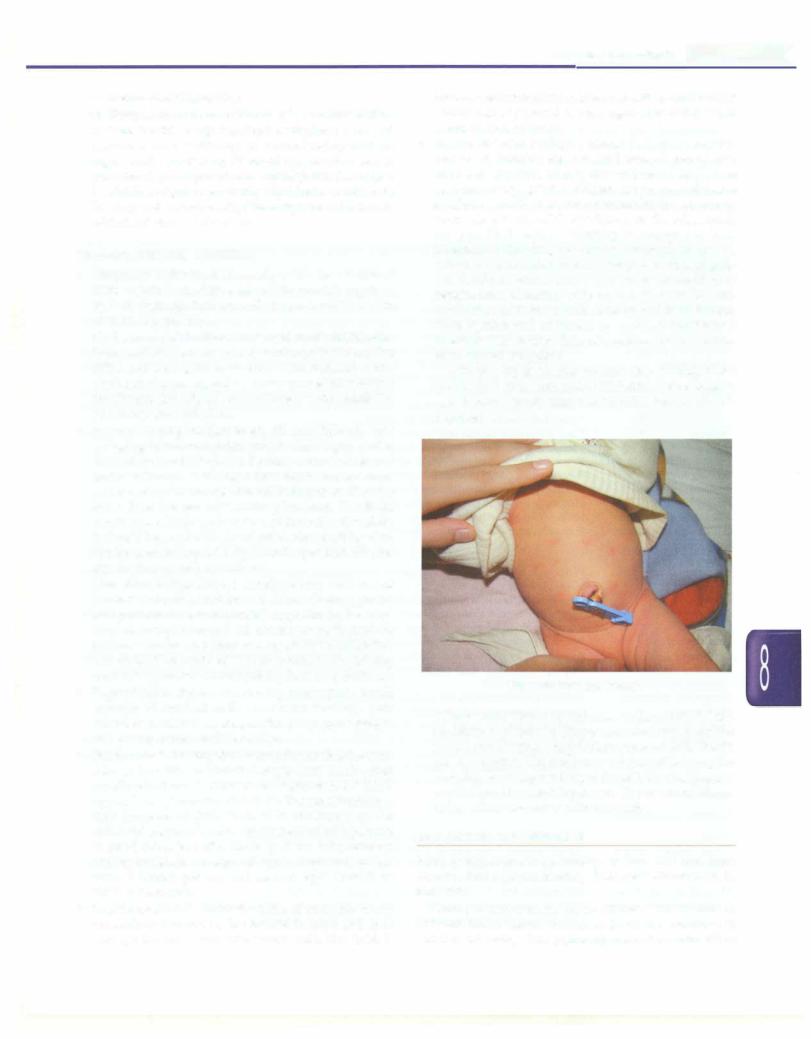
v.Severe chest indrawing
vi.Temperature of more than 37.5°C or below 35.5°C
•A date for followup has been assigned. A normal newborn with adequacy of breastfeeding and no significant jaundice by 72 hr of age can be seen at 6 weeks of age. In presence of any high risk factor (e.g. low birth weight, prematurity significant jaundice, or feeding not established), the baby should be seen within 2-3 days of discharge.
Common Parental Concerns
•Weight loss in first week: Normally babies lose 8-10% of birth weight in the first week of life which is regained by 7-10 days age. Subsequently there should be a gain of 20 to 40 g per day.
•Cryingduring micturition: The sensation of a full bladder is uncomfortable to many babies who cry before passing urine and they quieten as soon as micturition starts. Crying during passage of urine as opposed to before the act of rnicturitionshouldalert clinician to thepossibility of urinary tract infection.
•Bathing: During the first week, till cord falls off, only sponging is recommended which can be given after the first 24 hr of life. Later, bathing every 2-3 days is quite sufficient. A draught-free warm room, warm water and quick completion of bath ensure that the baby does not get cold during bathing. The head constitutes a large surface area of the baby; therefore, it should be washed last and dried first. Bathing time can be used to inspect baby's cord, eyes and skin for any discharge, rash or redness.
•Cosmetics: Babies have a sensitive skin and use of cosmetics should beminimized.A low alkalinity, mild, non-perfumed/non-medicated soap should be used. Any oil except mustard oil can be used. Sprinkling talcum powder on babies can result in its inhalation and should be avoided. Avoid products containing boric acid (present in most prickly heat preparations).
•Regurgitation: Babies commonly regurgitate small amount of curdled milk soon after feeding. This behavior is normal as long as the baby gains weight and passes urine 6-8 times a day.
•Frequent stools: During the first few days oflife, thestool color in breastfed neonates changes from black-green to yellow by the end offirst week. In between, thestools appear loose ('transitional stools'). The stool frequency may increase at this time. It is attributed to the enhanced gastrocolic reflex which results inthepassage of small stools just after feeding. If the baby remains well hydrated, has no signs of sepsis, feeds well, passes urine 6-8 times per day and gains weight, there is no cause for concern.
•Breast engorgement: Under the effect of transplacentally transmitted hormones, the breasts in boys and girls may get hypertrophied and secrete milk like fluid. It
Newborn Infants -
resolvesspontaneouslyin a few days. Engorgedbreasts should not be sqeezed or massaged as it could lead to soreness and infection.
•Rashes and skin peeling: Papular lesions on erythe matous basecanbe seeninmanybabies; dispersed over the trunk and face, on day two or three of life. These lesions, called erythema toxicum, are eosinophil-laden sterile lesions. Theyresolve spontaneously andrequire no treatment (Fig. 8.12). Pyoderma, on the other hand, are pus-filled lesions occurring in response to local infection of the skin, commonly occurring in creases where dirtaccumulatessuch as thigh fold, backof neck, etc. If boils are <10 in number and there are no signs of sepsis, local cleaning with antiseptic solution and application of 1.0% gentian violet is sufficient. Further investigation and treatment for sepsis is indicated if there are >10 lesions, signs of sepsis or non-resolution after topical treatment.
Skin peeling is another normal skin finding noted especiallyinpost-termand IUGRbabies.Oilmassaging can decrease the flaking and no other intervention is required.
Fig. 8.12: Erythema toxicum
•Diaper rash: There is redness, inflammation and excoriation of skin in diaper area due to maceration by stools and urine. The problem is more frequent with plastic nappies. The treatment consists of keeping the area dry, avoiding rubbing of the skin for cleaning and application of a soothing cream. Use of cotton diaper is less often associated with this rash.
EVALUATION OF NEWBORN
Most neonates are born healthy, normal and free from disease. Some (approximately 10%) need observation in nursery.
Newborn examination yields different information at different times. Hence, newborns should be examined in detail at following time points: (i) soon after birth, (ii) at
|
Essent iatPed iatrics |
______________ |
_______ |
|
|
__ |
_ _ _ _ _ _ _ _ _ _ _ _ _ _ _ ____________ |
|
|
|
|
|
||
24 hr of birth, (iii) before discharge from hospital, and again (iv) at followup visit.
Immediately after birth, the Apgar scores are assigned at 1 and 5 minutes (Table 8.2). If the score is less than 7, it is assigned every 5 minutes until 20 minutes or till two successive score are 7 or greater. These scores rapidly assess the cardiopulmonary status. Apgar scores may be falsely low in infants born very preterm and those with
maternal drug intake, sepsis, congenital heart disease and central nervoussystem malformations. Low Apgar scores are poor predictor of long term neurodevelopmental outcome.
If systemic examination reveals an abnormal finding, laboratory evaluation may be warranted. Table 8.7 provides a schema for the comprehensive history and examination of the newborn.
|
Table 8.7: Newborn history and examination: Format for case presentation |
History |
|
General |
Mother's name and age, parity, last menstrual period, expected date of delivery |
Past obstetric history |
Past pregnancies: when, gestation, fetal or neonatal problems, current status of children |
Antenatal |
Number of antenatal visits, tests (hemoglobin; urinealbumin, sugar; ultrasound; blood group, VDRL, |
|
HIV), tetanus toxoid immunization, supplements (iron, folic acid, calcium, iodine) |
Obstetric or medical |
Obstetric complications (toxemia, urinary tract infections, twins/triplets, placenta previa, accidental |
complications |
hemorrhage); fetal problems (IUGR, hydrops, Rh isoimmunization); medical problems (diabetes, |
|
hypertension); investigations, medications, course |
Labor |
Presentation, lie, onset of labor (spontaneous/induced), rupture of membranes (spontaneous/ |
|
artificial), liquor (clear/meconium stained); duration of first and second stage of labor; fetal heart |
|
rate (tachycardia, bradycardia, irregular) |
Delivery |
Place of delivery, vaginal (spontaneous/forceps/vacuum), cesarean (indication, elective/emergency); |
|
local/general anesthesia; other drugs; duration of third stage; postpartum hemorrhage |
Immediate care at birth |
Resuscitation; time of first breath and cry; Apgar score; cord care; passage of urine/stool |
Feeding history |
Breastfeeding (when initiated, frequency, adequacy); other feeds |
Postnatal problems |
Feeding problems, jaundice, eye discharge, fever; current problems |
Family history |
History of perinatal illness in other siblings |
Past medical problems |
History of past medical problems, if any |
Personal/social history |
Socioeconomic status, family support |
General examination |
|
Immediately after birth |
Weight, gestation,congenitalanomalies, sexassigning, Apgar scores,examination of umbilical vessel, |
|
and placenta |
Appearance |
Overall appearance: well or sick looking; alert/unconscious |
Vital signs |
Temperature, cold stress; respiratory rate, retractions, grunt/stridor; heart rate, palpable femoral |
|
arteries; blood pressure, capillary refill time; cry; apneic spells |
Anthropometry |
Weight, length, head circumference, chest circumference |
Gestation |
Assessment by physical criteria; more detailed assessment by expanded New Ballard examination |
Classification by |
Appropriate/small/large for gestational age; symmetric or asymmetric small for gestational |
intrauterine growth |
age; signs of IUGR |
Congenital anomalies |
Head to toe examination for malformations or abnormalities |
Birth trauma |
Signs of trauma; cephalohematoma |
Common signs |
Cyanosis, jaundice, pallor, bleed, pustules, edema, depressed fontanel |
Special signs |
Caput; eye discharge; umbilical stump: discharge or redness; jitteriness; eye discharge; oral thrush; |
|
development peculiarities (toxic erythema, Epstein pearls, breast engorgement, vaginal bleeding, |
|
capillary hemangioma, mongolian spot) |
Feeding |
Observe feeding on breast (check positioning and attachment) |
Reflexes |
Moro, grasp, rooting |
Systemic examination |
|
Chest |
Shape; respiratory rate; retractions; air entry; adventitious sounds |
Cardiovascular system |
Apical impulse, heart sounds, murmur |
Abdomen |
Distension, wall edema, tenderness, palpable liver/spleen/kidneys, any other lump, ascites, hernial |
|
sites, gonads, genitalia |
Musculoskeletal system |
Deformities; tests for developmental dysplasia of hip; club foot |
Central nervous system |
State of consciousness; vision, pupils, eye movements; facial sensation; hearing; sucking and |
|
swallowing; muscle tone and posture; power; tendon reflexes |
IUGR intrauterine growth retardation

General Observation
The least disturbing examination should be done first; this gives an opportunity to assess the state of alertness, posture, spontaneous activity, color, any obvious respiratory distress or malformation. The newborns should be examined when they are inlightsleep or awake but quiet (happens after 1-1.5 hr of feeding).
A newborn with hypotonia has an extended posture as in a baby with hypoxic encephalopathy. A clear note of the color of the baby, including cyanosis, pallor, jaundice and plethora should be made. One should also look at the spontaneous movements shown by the baby.
Vital Signs
In a sick baby, assessment of vitalparameterstakespriority over all other examination. Temperature is measured in the apex of the baby's axilla by holding the thermometer for at least 3 minutes. The finding of hypothermia (tempe rature of less than 36.5°C) in neonate has very important connotations. Neonates have a normal respiratory rate of 40-60 breaths/minute. The heart rate is faster in preterm babies compared to term babies. The normal range is 110-160 beats per minute. Bradycardia (rate <100/min) may be associated with heart disease while tachycardia (rate >160/min) may be due to sepsis, anemia, fever or congestive cardiac failure. Capillary refill time is assessed by applying firm pressure on the sternum area for 5 seconds than releasing and observing the time taken to refill. The refill time isprolonged (more than3 sec)because of poor peripheral circulation as in the shock or hypothermia.
Assessment of Size and Growth
Depending on the weight, the neonates are termed as low birthweight (LBW, less than 2500 g), very low birthweight (VLBW, less than 1500 g) or extremely low birth weight (ELBW, less than 1000 g). The aberrant growth pattern is assessed by plotting the weight against the gestational age on astandardintrauterinegrowthcurve (which is different from postnatal growth curves for assessing growth after birth), as shown in Fig. 8.13. A neonate whose weight falls between the 10th and <90th percentile is considered as appropriate for gestational age (AGA); if the weight falls below 10th percentile, the neonate is classified as small for gestational age (SGA); theneonate is classified as large for gestational age (LGA), if the weight falls at 90th percentile or above for gestational age.
Anthropometry
The weight is measured in grams (g). Length is measured using aninfantometer. The newborn baby at birth is about 50 cm long. Head circumference is measured by placing a soft non-stretchable tape around the head just above the eyebrows and finding the largest circumference over the occiput. This is 33-37 cm at birth in term babies. A large
|
|
|
|
|
f |
t |
Newborn Infants |
- |
||||
4000 |
|
|
|
|
|
... -- |
|
|
|
|||
3800 |
|
·l |
.. |
- |
f |
|
|
|
97 centile |
|||
3600 |
|
|
|
|
|
|
|
90 centile |
||||
3400 |
|
|
|
|
I |
|
|
|
|
I |
- |
|
|
|
|
|
|
|
|
|
|
-r I |
|
|
|
3200 |
|
|
-+ |
|
|
|
|
|
|
-1- |
|
|
|
|
|
|
|
|
|
|
|
||||
3000 |
|
|
|
|
|
|
|
|
|
|
|
50 centile |
|
|
|
|
|
|
|
|
|
|
|
|
|
2800 |
|
|
|
|
|
|
|
|
|
|
|
|
2600 |
|
|
|
|
|
|
|
|
|
|
|
10 centile |
2400 |
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
||
:E 2200 |
|
|
|
|
|
|
|
|
|
|
-2 SD |
|
|
|
|
|
|
|
|
|
|
|
|
||
- 2000 |
|
|
|
|
|
|
|
t.. -t- |
|
|
||
1800 |
|
|
|
|
|
1 |
|
|
|
|||
co |
|
|
|
|
|
|
|
|
||||
1600 |
|
|
|
|
|
|
|
|
|
|||
1400 |
|
|
|
|
|
|
t + |
|
.. |
T |
|
|
1200 |
|
|
|
|
|
|
..... |
|
+ |
|
|
|
1000 |
|
|
|
|
|
l |
t- ;.._ |
.. |
+ |
|
|
|
800 |
|
|
|
|
|
|
|
|
|
|
|
|
600 |
|
|
Preterm |
|
Term |
|
|
Post-term |
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
31 32 33 34 35 36 37 38 39 40 41 42 43 44
Gestation, weeks
Fig. 8.13: Intrauterine growth curves. SD standard deviation
head may be due to macrocephaly (Fig. 8.14), the causes includehydrocephalusandcerebralparenchymaldiseases. Chest circumference isabout3cmlesserthanheadcircum ference and if the difference is more than 3 cm it is an indication of intrauterine growth retardation (IUGR). The Pondera!index (Pl)iscalculatedbymultiplyingtheweight in grams by hundred and then dividing by cube of length in cm. This parameter is usually less than 2 in asymmetric IUGR baby and2 or more in a baby who has either normal growth or has symmetrical IUGR.
Fig. 8.14: A newborn infant with large head (macrocephaly). Note bossings of both frontal eminences

E |
ss__entia i Pediatrics------------------------------ |
- |
|
Assessment of Gestational Age
Based on gestation, neonates can be classified as preterm (<37 week), post-term ( 42 week) or term (37-41 completed weeks).
The detailed evaluation requires examination of physicalfeatures andneurological maturity (Fig. 8.15). The scoring system commonly used is the Expanded New Ballard Scores (ENBS), which has an accuracy of 1 week.
Regional General Examination
Skin and hair. The skin is examined with regard to thickness,transparency and edema, rashes andlesionslike hemangioma. Jaundice is detected by pressing on the skin so that the yellow color of subcutaneous tissue due to billirubin deposition is highlighted. The skin may exhibit minor clinical problems that are innocuous and self limiting. Ecchymoses or petechiae may relate to birth trauma,especially if presenton head andneck region. The hair shouldbe observed carefully. Lanugo are the fine hair of fetal period that shed in two periods; one at 28 weeks and later at term. The common finding on examination of nails is the presence of hypoplastic nails that may be transient in the toe, but, if present in fingers, may indicate
exposure to valproate.
Head and fontanel. The size and shape of the head along with sutures and fontanels should be examined carefully. Upon palpation, molding gives the impression of a cliff with rise on one side and a sharp fall on the other side, whereas a synostosis (fusion of bones) feelslike a mountain range with rise on both sides of elevation. Some neonates have delayed ossification and resorption of bones making the skull feel soft like a ping pong ball. This condition, termed craniotabes, is benign in neonates and it resolves spontaneously. The most common findings after birth are
caput succedaneum and cephalohematoma (Fig. 8.16). These
should be differentiated as shown in Table 8.8. A full and tense fontanel is abnormal in a quiet neonate. Large fontanels and split sutures are mostoftennormal variants but they can be associated with increased intracranial pressure, certain chromosomal abnormalities, hypo thyroidism and impaired bone growth like osteogenesis imperfecta.
Neck,face, eyes and ears. Newborns have short necks. The neck is examined for masses such as enlarged thyroid gland, sternomastoid tumor and cystic hygroma. Facial nerve paresis may occur due to birth injury; this is identified by the presence of asymmetric fades while the baby is crying with open eyes and the inability to move the lips. This should be differentiated from the absence of depressor anguli oris in which asymmetric crying fades is observed; however, in this condition, the eyes remain tightlyshutwhilecrying (Fig. 8.17A and B). Nose is looked for its size, shape, secretions, patency and flaring. The flaring of the nostrils indicates an increase in respiratory efforts regardless of the cause.
The alveolar ridge may have natal teeth or retention cysts (also called Epstein pearls) that disappear in few weeks. It is very important to examine the palate for cleft.
Subconjunctival hemorrhages are common after vaginal delivery and resolve spontaneously. The cornea should be clear. Pupils should be equal in size, reactive to light and symmetrical.
Gross hearing is often assessed by looking for blink on response to noise. More formal hearing screening for all newborns is now recommended. Accessory auricles and preauricular tags are common finding that may be associated with renal anomalies.
Umbilicus, anus and spine: Inspect the number of vessels in the umbilical cord. A single umbilical artery may be found in 0.7% of live births; this may be associated with renal and gastrointestinal tract anomalies.
One should palpate the base of the umbilical cord for a hernia and estimate the diameter of the fascial opening (Fig. 8.18). The spine should be palpated with a finger to exclude spina bifida, masses and any scoliosis. The anal opening should be examined for its patency and position.
Genitalia (male and female): The genital area is examined
by the hips abducted in the supine position. The urethra and clitoris are examined for patency and cliteromegally respectively.
Extremities: One should make surethat the arms and limbs are fully movable with no evidence of dislocation or asymmetry of movements. The fingers are counted and any abnormality noted like nail hypoplasia, syndactyly, polydactyly, oligodactyly or unequal limbs. A calcaneo valgus deformity is usually self-correcting within the next few months but equinovarus is much more sinister and shouldbe brought to the notice of an orthopedic specialist (Fig. 8.19).
Systemic Examination
Chest The anteroposteriordiameterof theneonate'schest is roughly same as the transverse diameter. Respiratory distress is indicated by nasal flaring, grunting, tachypnea and intercostal and subcostal retractions. Such distress may indicate pneumonia, respiratory distress syndrome (RDS), delayed reabsorption of lung fluid or any other cardiorespiratory cause. Stridor may be inspiratory, indicating large airway obstruction, or there may be expiratory prolongation, indicating a small airway obstruction.
Cardiovascular system An infant with heart disease manifests with tachypnea, cyanosis or both. The position of apical impulse may give idea regarding presence of conditions likecongenital diaphragmatichernia(CDH)and pneumothorax.
Abdomen Inspection of abdomen may reveal unusual flatness or scaphoid shape of abdomen that may be
Newborn Infants -
Term Babies |
Preterm Babies |
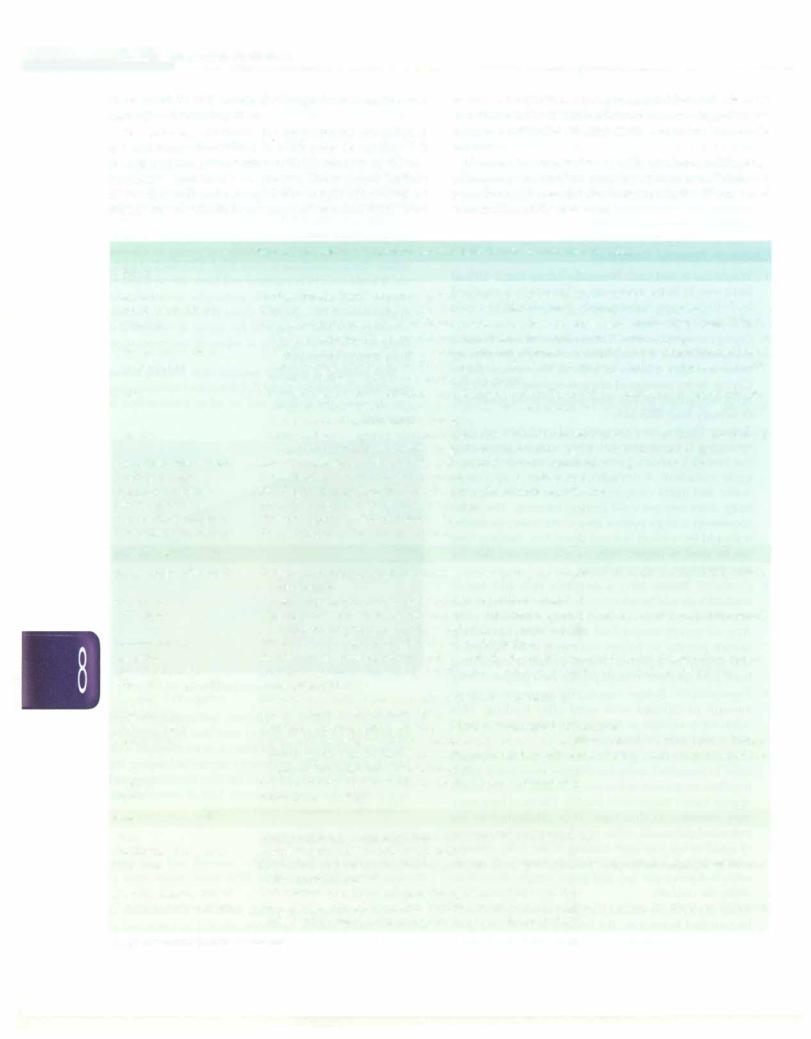
Figs 8,1 SA to F: Salient difference in physical characteristics of preterm and term neonates: (A) Well-curved pinna, cartilage reaching up to periphery; (B) flat and soft pinna, cartilage not reaching up to periphery; (C) well pigmented and pendulous scrotal sacs, with fully descended testes; (D) light pigmentation and not yet descended testes; (E) deep transverse creases on the soles; (F) faint marks on the sole, no deep creases

__Essent iaiPed iatrics________________________________ _
_______________
Term Babies |
Preterm Babies |
Figs 8.1 SG to L: Salient difference in physical characteristics of preterm and term neonates: CG) Well formed breast bud C>S mm); CH) Poorly developed breast bud; Cl) silky hair, where individual strands can be made out; (J) fuzzy hair; CK) labia majora covering clitoris and labia minora; CL) prominent labia minora and clitoris

|
|
|
Newborn Infants - |
|
Table 8.8: Differences between caput succedaneum and cephalohematoma |
||
Characteristic |
Caput succedaneum |
Cephalohematoma |
|
Incidence |
Common |
Less common |
|
Location |
Subcutaneous plane |
Over parietal bones, between skull and periosteum |
|
Time of presentation |
Maximum size and firmness at birth |
Increasing size for 12-24 hr and then stable |
|
Time course |
Softens progressively from birth |
Takes 3----6 weeks to resolve |
|
|
and resolves within 2-3 days |
|
|
Characteristic findings |
Diffuse; crosses suture line |
Does not cross suture line; has distinct margins |
|
Association |
None |
Linear skull fracture (5-25%); hyperbilirubinernia |
|
back with the knees fully flexed and the hips flexed to arightangle. Boththehipsshouldbetestedseparately. Pelvisisstabilizedwithonehand withthumbbeingon the medial side of thigh and fingers on greater
Fig. 8.16: Cephalohematoma. Note the overlying bruising
associated with CDH. Visible gastric or bowel patterns may indicate ileus or other obstruction. Normally 1-2 cm of liver, tip of the spleen and the lower pole of the left kidney may be palpated. Tenderness of abdomen is an important sign in necrotizing enterocolitis (NEC).
Musculoskeletal system The common alterations are deformations caused by adverse mechanical factors in utero. Most positional deformities are mild and resolve in time. The hipsare tobe examined to detect hipproblems before permanent damage occurs by one year of age.
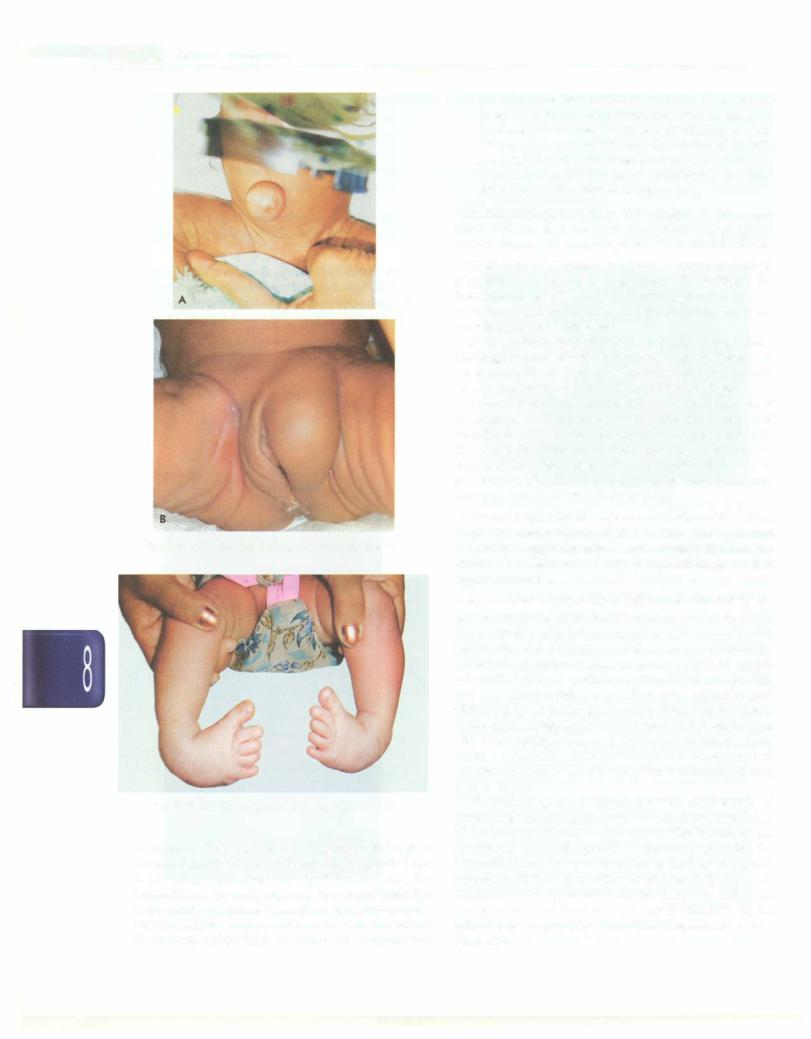
Developmental dysplasia of hips (DOH) occurs in 1 of 800 livebirths, more commonlyin girls, those with a family history and deliveredby breech. There are two major tests to detect developmental dysplasia of hip (DOH).
i.Barlow maneuver: Barlow test is done to dislocate the unstable hip joint. Both the hips should be tested separately. Pelvis is stabilized with one hand with thumb being on the medial side of thigh and fingers on greater trochanter. With the other hand, opposite hip is flexed and adducted, and posterior pressure is applied with thumb so as to dislocate hip. If the hip is dislocatable, a distinct outward movement of the hip is felt. Once pressure is released, hip moves again in the acetabulurn.
ii.OrtoZani's sign. This maneuver helps to judgeif thehip has already been dislocated. The baby is placed on its
Figs 8.17A and B: (A) Absent depressor anguli oris muscle. Note asymmetry of face on crying, presence of nasolabial folds and closed eyes. (B) newborn with right sided lower motor nerve facial palsy secondary to forceps application. Note absence of nasolabial fold
E |
_s_s_e_n_ti_a _i _P_e _d_ia_t_ri_cs--------- |
--------- |
|
- |
|||
|
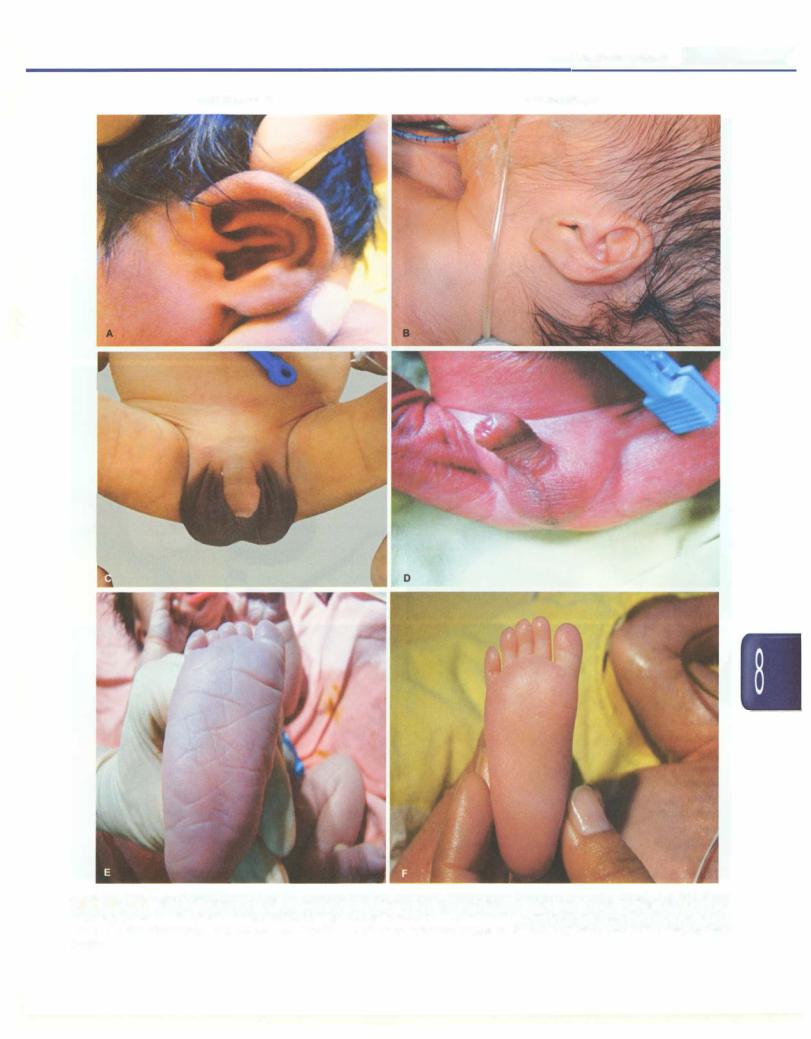
Figs 8.18: (A) Umbilical hernia; and (B) Inguinal hernia
Fig. 8.19: Congenital talipes equinovarus deformity
trochanter. With the other hand, opposite thigh is abductedand thefingersoftheexamininghandspush the femoral head anteriorly. In dislocated hip, the femoral head suddenly slipsintothe acetabulum with a distinctly palpable "clunk". If pressure is now applied with the thumbs outwards and backwards of theinnersideof the thigh,thefemoralheadagainslips
overtheposteriorlip of the acetabulum. Ifthefemoral headslipsintotheacetabulumagainwhenthepressure isreleased, itismerelyunstable,ratherthandislocated. This test is important because the treatment in early neonatallifeissimpleandefficientandconsistssimply in maintaining the hips in full abduction and at least 90° flexion with malleablemetal splints.
Neurological examination This consists of the assess ment of the level of alertness and examination of cranial nerves, motor and sensory system and neonatal reflexes.
Cranial nerves. Neonates respond to cotton soaked in peppermint by 32 weeks of gestation. By 26 weeks the infant consistently blinks in response to light and by term gestation, fixation and following (tested using fluffy red yarn ball) is well established.
By 28 weeks the infant startles or blinks to loud noise. Suckingandswallowing areimportantaspectsthatshould be examined as they give insight into the proper functioning of the V, VII, IX, X and XII cranial nerves.
The act of sucking requires the coordinated action of breathing, sucking and swallowing. Suck-swallow coordination so asto accept paladai feeding is present by 32 weeks. Suck-swallow and breathing coordination occurs by 34 weeks when baby can breastfeed. However, perfect coordination of suck-swallow and breathing develops only by 38 weeks of gestation.
Motor examination. By28 weeks there is minimal resistance to passive manipulation of all the limbs and a distinct flexortoneisappreciatedin lowerextremities by32 weeks. By 36 weeks, flexor tone is palpable in both the lower and upper extremities.
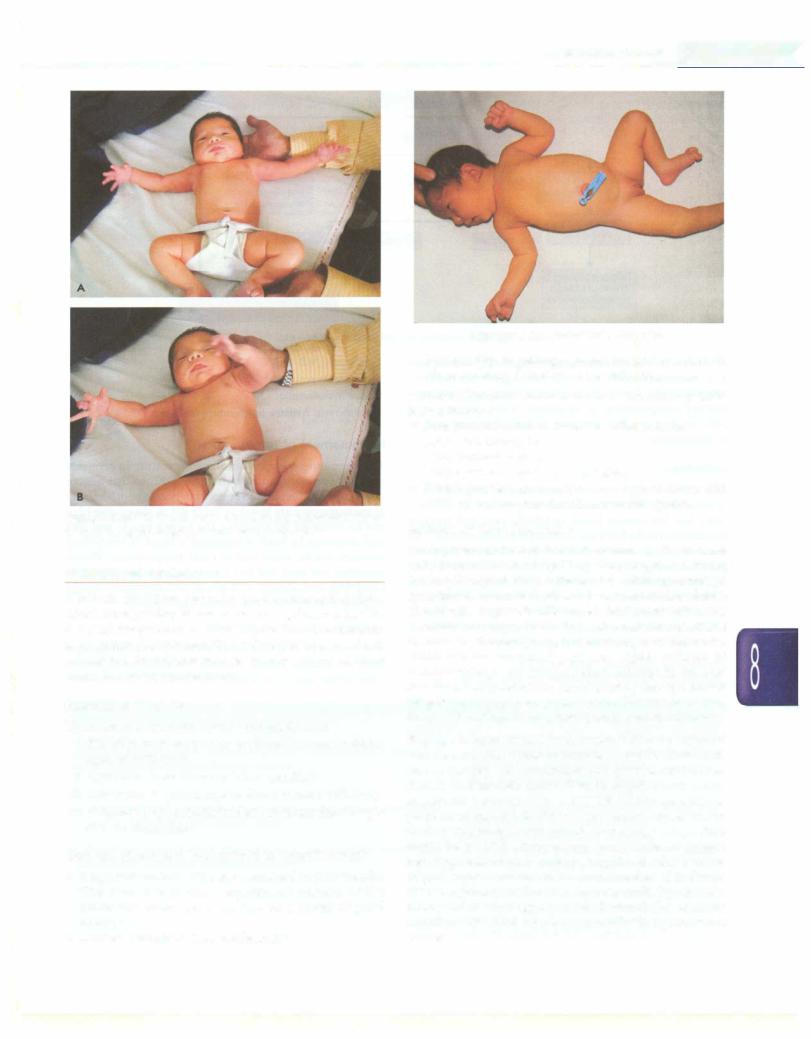
Primary neonatal reflexes. Moro reflex is best elicited by the sudden dropping of the baby's head in relation to trunk; the response consists of opening of the hands and extension and abduction of the upper extremities, followed by anterior flexion (embracing) of upper extremities with an audible cry (Figs 8.20A and B). The hand opening is present by 28 weeks, extension and abduction by 32 weeks and anterior flexion by 37weeks. Moro reflex disappears by 3-6 months in normal infants. The most common cause of depressed or absent Moro reflex is a generalized disturbance of the central nervous system. An asymmetrical Moro reflex is indicative of root plexus injury.
The palmar grasp is clearly present at 28 weeks of gestation and is strong by 32 weeks. This allows the lifting of the baby at 37 weeks of gestation. This becomes less consistent on development of voluntary grasping by 2 months. The tonic neck response is another important response elicited by rotation of the head, that causes extension of the upper extremity on theside to which the face is rotated and flexion of the upper extremity on the side of the occiput (Fig. 8.21). This disappears by 6 to 7months.
-----------------------------------Newborn infan ts.....-
Figs 8.20A and B: Moro reflex (A) Abduction and extension of arms is followed by (B) Adduction and flexion component
THERMAL PROTECTION
Newborn babies are prone to hypothermia as they have poorheatregulating mechanisms. During intrauterinelife, the fetal temperature is 0.5°C higher than the maternal temperature due to metabolic reactions that generate heat. After birth, the infant is exposed to outside environment which has lower temperature.
Sources of Heat Loss
Heat loss in a newborn occurs through 4 ways:
i.Radiation to surrounding environment not in direct contact with baby
ii.Convection to air flowing in surrounding
iii.Conduction to substances in direct contact with baby
iv.Evaporation ofamnioticfluidandmoisturefrom baby's skin to atmosphere
Why are Ne wborns Susceptible to Hypothermia?
•Large surface area of babies compared to their weight: The head constitutes a significant portion of the newborn's surface area and can be a source of great heat loss
•Limited heat generating mechanisms
Fig. 8.21: Asymmetrical tonic neck reflex
•Vulnerability to getting exposed, being dependant on others for early detection and rectification
Additional factors that contribute to heat loss in LBW babies include:
•Poor insulation due to lower subcutaneous fat
•Decreased brown fat
•More permeable skin
•Larger surface area than term babies
•Poorer physiological response to hypothermia and early exhaustion of metabolic stores like glucose.
Sources of Heat Production
On exposure to cold and wet environment, the neonate tries to generate heat by increasing physical activity (crying, increased body movements) and by mounting a
sympathetic surge that causes vasoconstriction and non shivering thermogenesis in the brownfat. Brown fat is richly
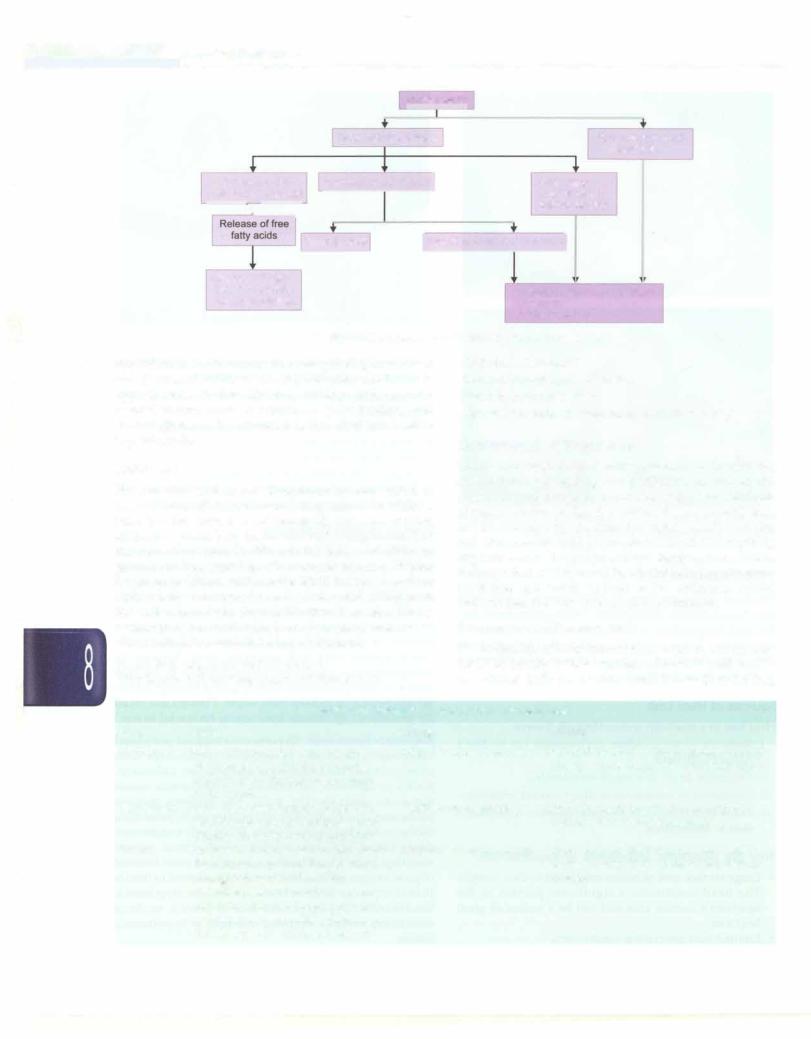
vascularized, sympathetically innervated fat collections located in the axillae, groin and nape of the neck, interscapular area and perirenal area. Release of norepinephrine uncouples beta-oxidation in fat that results in heat production. Blood passing through brown fat gets heated up to keep baby warm. Preterm and small for gestational age infants have scanty brown fat stores. Response to hypothermia. Hypothermiainduced peripheral vasoconstriction leads to increased metabolism with excess oxygen consummation and glucose utilization. Switch to anaerobic metabolism in hypothermia causes metabolic acidosis (Fig. 8.22). The acidosis induces pulmonary vasoconstrictionandpulmonary hypertension furtherworseningthehypoxemia. Whenbodytemperature drops below 32°C, hemoglobin cannot release oxygen resulting in the blood having a bright red color because of good oxygen content but it cannot be released to tissues (tissue hypoxia). With severe hypothermia, hypoxemia, bradycardia, hypoglycemia and metabolic acidosis contributes towards increased mortality in hypothermic babies.
|
|
n |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
|
Ess_e__tia_i_P_edia_trics |
|
|
|
|
|
____________________ |
||||||||||||||
|
__ |
|
|
|
|
____________ |
|
|
|
|
|
||||||||||
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
Hypothermia |
|
|
|
|
|
||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Catecholamine release |
|
|
|
Reduced surfactant |
|||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
production |
|
|
|
|
Uncoupling of-I} |
|
|
Increased metabolic ratej |
|
Pulmonary |
|
||||||||||||
|
|
oxidation in brown fat |
|
|
|
|
|
|
|
and peripheral |
|
||||||||||
|
|
|
|
|
|
|
|
|
|
||||||||||||
|
|
|
|
I |
|
|
|
|
|
|
|
|
vasoconstriction |
|
|||||||
|
|
|
|
_ |
|
|
|
|
|
|
|
|
|||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Hypoglycemia |
|
I Increased oxygen requirementj |
|
|
|||||||||
|
|
|
Displace bilirubin |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
bound to albumin |
|
|
|
|
|
|
|
|
|
|
|
Anerobic metabolism, glycolysis |
||||||
|
|
|
Hyperbilirubinemia |
|
|
|
|
|
Hypoxemia |
||||||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Metabolic acidosis |
||||
Fig. 8.22: Response to cold stress in sick neonate
Hyperthemiia. An immature thermoregulating mechanism and decreased ability to sweat predispose newborns to hyperthermia. Factors like overclothing, high environ mental temperature in summers, poor feeding and dehydration are the common factors that can lead to hyperthermia.
Defintions
Thermoneutral environment. Thermoneutral zone refers to narrow range of environmental temperature in which a baby has the lowest basal metabolic rate and oxygen utilizationandthebabyhas normal body temperature. The thermoneutral zone is different for babies of different gestation and postnatal age. Thermoneutral zone is higher for lower gestation and smaller birth weight; lower for clothed babies compared to naked ones and is higher in the earlier hours and days of life than later age. This is because preterm, small, naked and younger neonates need extra warmth to maintain body temperature.
Normal body temperature: 36.5°C to 37.5°C
Hypothermia: Axillary temperature less than 36.5°C
Cold stress: 36.0-36.4°C Moderate hypothermia: 32-35.9°C Severe hypothermia: <32°C
Hyperthermia: Axillary temperature more than 37.5°C
Measurement of Temperature
The thermometer for measuring temperature in neonates should have low reading values till 30°C, so that degree ofseverehypothermiacan beaccuratelyassessed.Methods of measurement are listed in Table 8.9. A reasonable idea can be obtained by touching the baby's hands and feet and abdomen by back of examiner's hand. If everything appears warm, baby has normal temperature. Warm abdomen but cold feet and hands indicate hypothermia. Cold feet and hands as well as the abdomen would indicate that the baby has severe hypothermia.
Frequency of Measurement
The frequency of temperature measurement can be once daily for healthy babies who are otherwise well, two to three times daily for healthy small babies (2 to 2.5 kg),
|
Table 8.9: Methods of temperature measurement |
||
Name |
Method |
Timing |
Comment |
Axillary |
Bulb of thermometer is placed in |
Intermittent measurement |
Standard method of temperature recording; |
|
the roof of dry ax.ilia for 3 minutes |
|
closely approximates the core temperature |
|
while holding the baby's arm close |
|
|
|
to the trunk |
|
|
Skin probe |
Probe of thermal sensor is placed on |
Continuous monitoring |
Useful in regulating the heater output in |
|
the skin over upper abdomen; panel |
|
radiant warmer and incubators |
|
displays the measured temperature |
|
|
Touch |
The back of hand is used to appreciate |
Intermittent measurement |
Crude method; helps mothers and health |
|
the skin temperature. Temperature is |
|
workers estimate the baby's temperature |
|
considered normal if the baby's |
|
quickly |
|
abdomen, feet and hands are warm; |
|
|
cold if the abdomen is warm but feet and hands are cold; and hypothermia if abdomen, feet and hands are cold
