Ghai Essential Pediatrics8th
.pdf

|
Diseases of Gastrointestinal System and Liver |
||
Table 11.1: Causes of vomiting |
or photophobia. These patients need immediate |
||
Gastrointestinal |
Nongastrointestinal |
investigation in a hospital. |
|
Workup for chronic vomiting should include evaluation |
|||
|
|
||
Acute |
|
for cause with blood chemistry (blood sugar, electrolytes, |
|
|
|
||
Gastroenteritis |
Infections, e.g. urinary tract |
serum amylase and liver enzymes); ultrasound abdomen, |
|
Hepatitis |
infection, meningitis, ence |
upper gastrointestinal endoscopy and, as indicated by |
|
Appendicitis |
phalitis, pertussis |
available clues, barium studies (meal and small bowel |
|
Small intestinal obstruction, |
Raised intracranial tension |
follow-through), gastric emptying scan, CT or MRI brain, |
|
(malrotation, volvulus, |
Diabetic ketoacidosis |
metabolic testing or urine analysis. It is important to |
|
intussusception) |
Defects in fatty acid oxidation |
||
remember that children with cyclic vomiting should be |
|||
Cholecystitis |
or respiratory chain |
||
evaluated during symptomatic attack before starting |
|||
Pancreatitis |
Drug or toxin induced |
||
intravenous fluids since test results are typically non |
|||
|
|
||
Chronic |
|
contributory during asymptomatic periods. |
|
|
|
||
Gastroesophageal reflux |
Raised intracranial tension |
Evaluation of a child with acute vomiting should |
|
include assessment of hydration, electrolytes, creatinine |
|||
Gastritis |
Chronic sinusitis |
||
Gastric outlet obstruction |
Uremia |
and plain X-ray abdomen (in suspected surgical causes). |
|
(hypertrophic pyloric |
Overfeeding |
Promethazine andondansetron are usefulin postoperative |
|
stenosis, peptic ulcer) |
|
vomiting and to abort episodes of cyclical vomiting. |
|
Small bowel obstruction |
|
Ondansetron, given alone or with dexamethasone, is |
|
(duodenal stenosis, annular |
|
preferred for chemotherapy related vomiting. Domperi |
|
pancreas, superior |
|
done and metoclopramide are useful in patients with |
|
mesenteric artery syndrome) |
|
||
|
gastroparesis.Antihistaminicslikediphenhydraminehelp |
||
Food allergy |
|
||
|
in motion sickness. Management of the underlying |
||
Achalasia cardia |
|
||
|
condition is essential. |
||
Gastroparesis |
|
||
|
Some common disorders presenting with vomiting are |
||
Eosinophilic esophagitis |
|
||
|
described below: |
||
Recurrent |
|
||
|
|
||
Cyclic vomiting |
Urea cycle defects |
Idiopathic Hypertrophlc Pyloric Stenosls |
|
Abdominal migraine |
Diabetic ketoacidosis |
Hypertrophicpyloricstenosisisthe mostcommonsurgical |
|
Malrotation with volvulus |
Addison disease |
||
disorder of thegastrointestinal tract in infants. The pylorus |
|||
|
|
||
(>2/week) at low intensity (1-2 emesis/hr). While chronic |
is thickened and elongated with narrowing of its lumen |
||
due to hypertrophy of the circularmusclefibersof pylorus. |
|||
vomiting is usually caused by a gastrointestinal etiology, |
Clinical presentation. The classical presentation is with non |
||
cyclic vomiting is predominantly due to neurologic, |
|||
bilious vomiting that gradually increases infrequency and |
|||
metabolic and endocrine causes. |
|||
severity to become projectile in nature. The disorder is |
|||
|
|
||
Evaluation |
|
4-6 times more common in boys than girls. Most patients |
|
A detailed history and examination often gives clue to the |
present with vomiting starting beyond 3 weeks of age; |
||
however, about 20% are symptomatic since birth and |
|||
diagnosis. The etiology of vomiting varies according to |
|||
presentation is delayed until 5 months of age in others. |
|||
age; while infectious causes occur across all ages, most |
|||
Constipation is common.Recurrent and persistent vomi |
|||
congenitalanomalies,e.g. atresiaor stenosis andmetabolic |
|||
ting causes dehydration, malnutrition and hypochloremic |
|||
disorders, present in the neonatal period or infancy. The |
|||
alkalosis. As the stomach muscles contract forcibly to |
|||
first step is to find out whether the vomitus is bilious or |
|||
overcome the obstruction, a vigorous peristaltic wave can |
|||
nonbilious. This determines the site of disease. Lesions |
|||
be seen to move from left hypochondrium to umbilicus, |
|||
beyond the ampulla of Vater cause bilious vomiting and |
|||
particularly on examination after feeding. A firm olive |
|||
those proximal to it lead to nonbilious vomiting. Asso |
|||
shaped mass is palpable in the midepigastrium in 75-80% |
|||
ciated features may indicate etiology, e.g. vomitus con |
|||
infants, especially after feeds. |
|||
taining stale food of previous day (suggests gastric outlet |
|||
|
|||
obstruction), visible peristalsis (obstruction), vomiting in |
Evaluation. Ultrasound abdomen is the diagnostic |
||
early morning (intracranial neoplasm or cyclic vomiting |
investigation and shows muscle thickness of >4 mm and |
||
syndrome), vertigo (middle ear disorder) and hypotonia |
pyloruslengthof>16mm. Theultrasoundis100%sensitive |
||
(mitochondrial disorders). The 'red flag' symptoms and |
and nearly 90% specific in diagnosis of hypertrophic |
||
signs in a child with vomiting are the presence of blood |
pyloric stenosis. However, in case of doubt, an upper GI |
||
or bile in the vomitus, severe abdominal pain with |
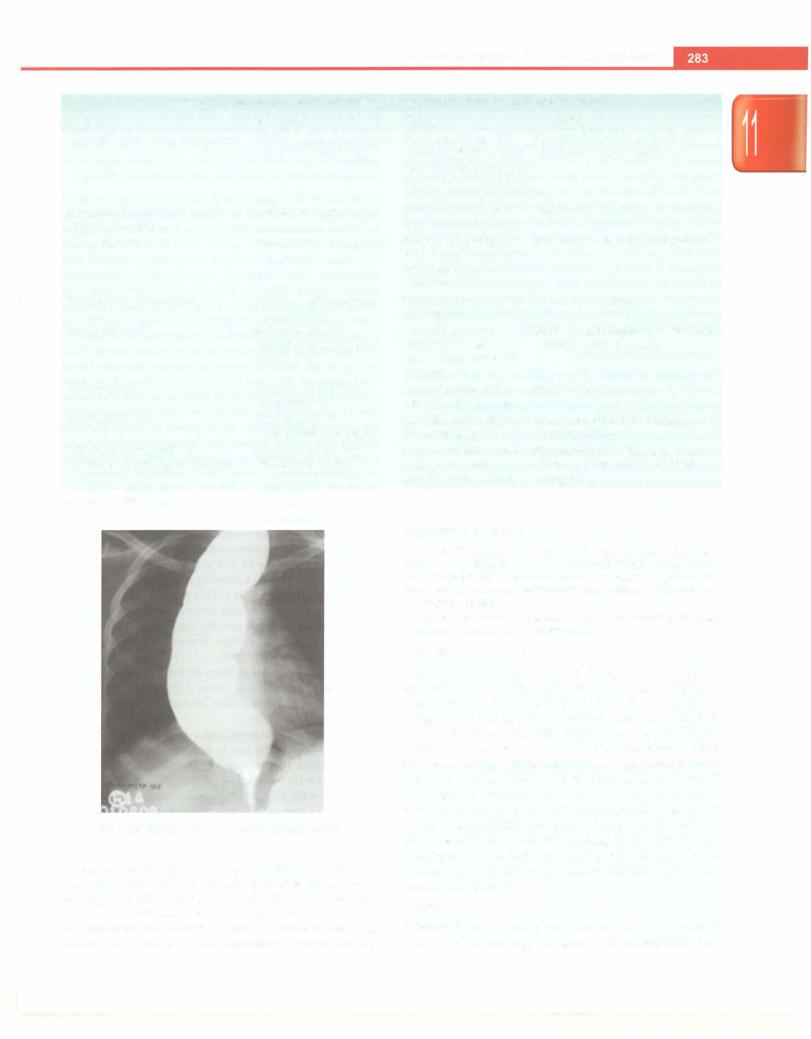
barium study can show a consistent elongation of the |
||
abdominal distension or tenderness, projectile vomiting, |
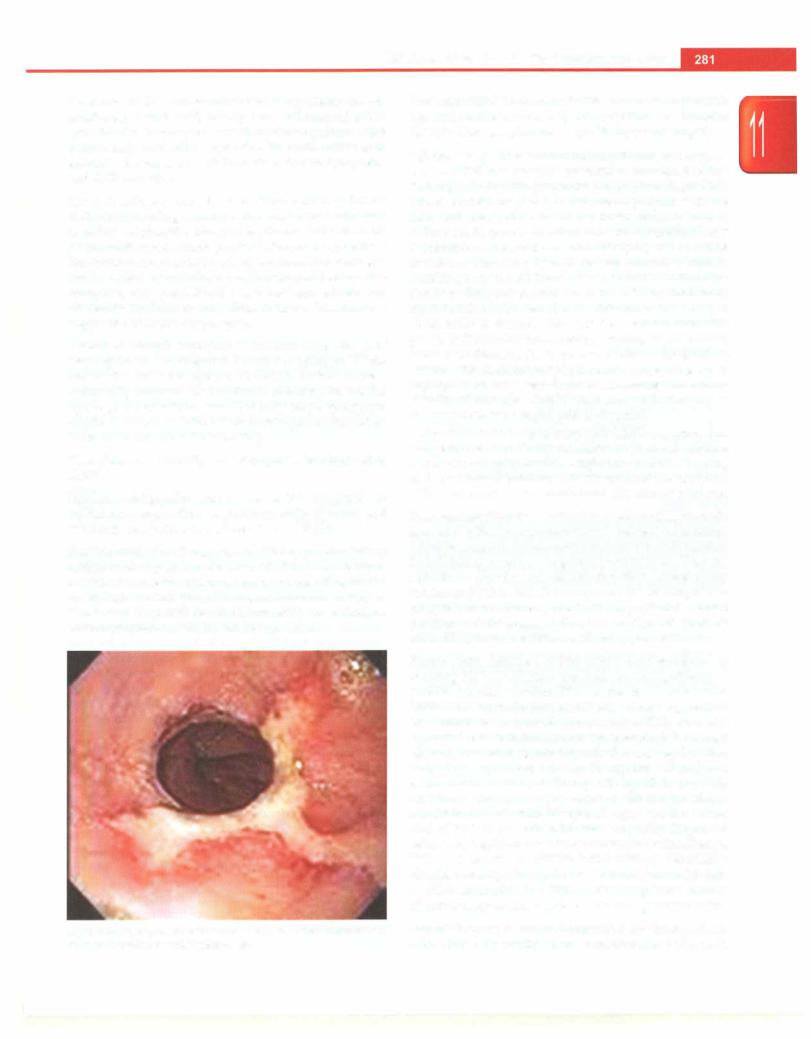
pyloric channel (Fig. 11.1) or an upper GI endoscopy is |
||
persistent tachycardia or hypotension, neckstiffness and/ |
performed. |
||