
Intermediate Physics for Medicine and Biology - Russell K. Hobbie & Bradley J. Roth
.pdf
474 |
16. Medical Use of X Rays |
|
|
|
|
|
|
|
|
Symbol |
Use |
Units |
|
First |
Q |
Quality factor |
|
468 |
|
|
|
|
|
used on |
R |
Resistance |
Ohm (Ω) |
444 |
|
|
|
|
|
page |
S |
Area |
m2 |
452 |
|
k |
Minimum |
|
|
452 |
S |
Surviving fraction |
J m−1 |
462 |
|
|
signal-to-noise ratio |
|
|
|
Se (or Sc) |
Collision stopping |
467 |
||
kB |
Boltzmann factor |
J K−1 |
|
445 |
|
power |
|
|
|
l |
Orbital angular |
|
|
438 |
T |
Kinetic energy |
J |
438 |
|
|
momentum quantum |
|
|
|
T0 |
Initial kinetic energy |
J |
439 |
|
|
number |
|
|
|
T |
Optical transmission |
|
441 |
|
m |
Mass |
kg |
|
440 |
T |
Temperature |
K |
445 |
|
me |
Mass of electron |
kg |
|
443 |
W |
Mean energy expended |
J or eV |
439 |
|
m |
Mean number |
|
|
451 |
|
per ion pair formed |
|
|
|
m |
Number of scans |
|
|
457 |
WR |
Radiation weight factor |
|
468 |
|
n |
Principal quantum |
|
|
438 |
WT |
Tissue weighting factor |
C kg−1 |
469 |
|
|
number |
|
|
|
X |
Exposure |
440 |
||
n |
Number of slices in a |
|
|
456 |
Z |
Atomic number |
|
437 |
|
|
scan |
|
|
|
α |
Integral of attenuation |
Gy−1 |
454 |
|
n |
Number of moles of a |
mol |
|
439 |
α |
Dose proportionality |
460 |
||
|
substance |
|
|
|
|
constant |
Gy−1 |
|
|
n |
Number of fractions |
|
|
462 |
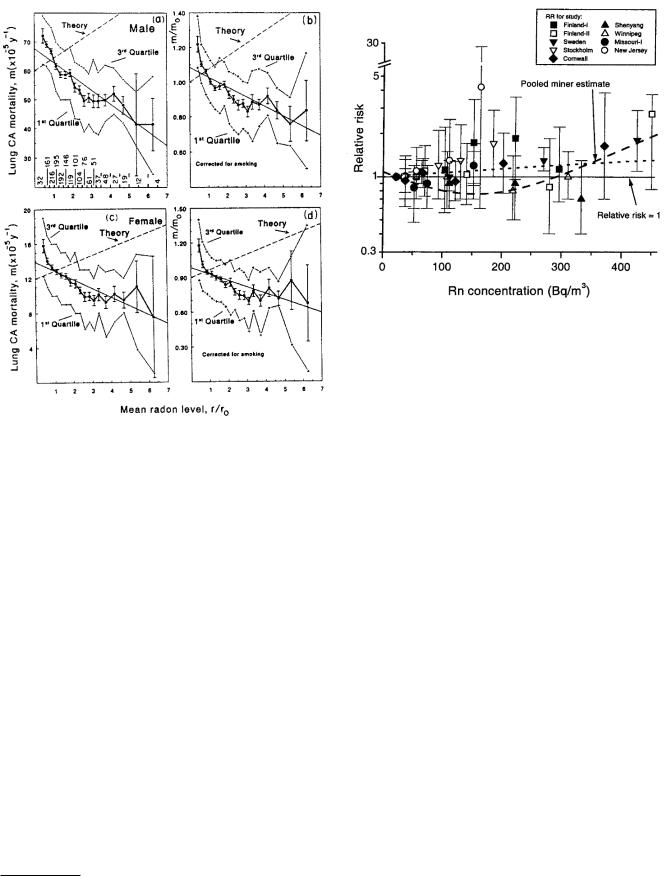
α |
Excess risk |
471 |
||
p |
Probability |
|
|
463 |
|
proportionality |
|
|
|
q |
Charge |
C |
|
440 |
|
constant |
|
|
|
r |
Distance |
m |
|
447 |
β |
Coe cient |
Gy−2 |
457 |
|
r |
Risk or probability |
varies |
|
470 |
β |
Squared dose |
460 |
||
r, r0 |
Radon concentrations |
Bq m−3 |
472 |
|
proportionality |
|
|
||
v |
Voltage di erence |
V |
|
444 |
|
constant |
|
|
|
w |
Width of picture |
m |
|
456 |
γ |
Fraction |
|
457 |
|
|
element |
|
|
|
γ |
Film contrast |
m−1 |
441 |
|
wi |
Mass fraction of ith |
|
|
447 |
µ, µatten |
Attenuation coe cient |
447 |
||
|
constituent |
|
|
|
µen |
Energy absorption |
m−1 |
440 |
|
x |
Photon |
|
|
443 |
|
coe cient |
|
|
|
|
energy/electron rest |
|
|
|
ν, ν0 |
Frequency |
Hz |
438 |
|
|
mass energy |
|
|
|
ρ |
Density |
kg m−3 |
440 |
|
x, y, z |
Coordinates |
m |
|
441 |
σ |
Standard deviation |
m−2 |
471 |
|
A |
Proportionality |
C m2 kg−1 |
451 |
Φ |
Particle fluence |
438 |
|||
|
constant |
|
|
|
ΦT |
Particle fluence per |
m−2 J−1 or |
467 |
|
C |
Constant |
J−1 m−2 |
438 |
|
unit energy interval |
m−2 eV−1 |
|
||
C |
Capacitance |
F |
|
444 |
Ψ |
Energy fluence |
J m−2 |
438 |
|
Cin |
Exposure contrast |
|
|
451 |
|
|
|
|
|
Cout |
Brightness contrast |
|
|
451 |
Problems |
|
|
||
D |
Absorbed dose |
Gy (J kg−1) |
440 |
|
|
||||
|
|
|
|
||||||
D |
Absorbed dose in one |
Gy |
|
457 |
Section 16.1 |
|
|
||
|
scan |
|
|
|
|
|
|||
D0 |
Reciprocal of |
Gy |
|
460 |
Problem 1 Use Eqs. 15.3 and 16.2 to answer the follow- |
||||
|
proportionality |
|
|
|
|||||
|
constant α |
|
|
|
ing questions. Then compare your answers to values given |
||||
DR,T |
Absorbed dose of |
Gy |
|
468 |
in tables, such as those in the Handbook of Chemistry and |
||||
|
radiation type R to |
|
|
|
Physics. What is the minimum energy of electrons strik- |
||||
|
target organ T |
|
|
|
|||||
|
|
|
|
ing a copper target that will cause the K x-ray lines to |
|||||
E |
Energy |
J or eV |
438 |
||||||
appear? What is the approximate energy of the Kα line? |
|||||||||
E |
E ective dose to an or- |
Sv (J kg−1) |
468 |
||||||
|
gan |
|
|
|
Repeat for iodine, molybdenum, and tungsten. |
|
|||
F |
Projection (integral) of |
|
|
455 |
Problem 2 When tungsten is used for the anode of an x- |
||||
|
f along some direction |
|
|
|
|||||
G |
Radiation chemical |
mol J−1 |
439 |
ray tube, the characteristic tungsten Kα line has a wave- |
|||||
|
yield |
kg C− |
1 |
|
length of 2.1 × 10−11 m. Yet a voltage of 69, 525 V must |
||||
G |
Large signal transfer |
|
442 |
be applied to the tube before the line appears. Explain the |
|||||
|
factor |
|
|
|
discrepancy in terms of an energy-level diagram for tung- |
||||
H |
Hounsfield CT unit |
|
|
456 |
|||||
|
|
sten. |
|
|
|
||||
H |
Dose equivalent |
Sv (J kg−1) |
468 |
|
|
|
|||
HE |
E ective dose |
Sv |
|
469 |
Problem 3 Henry Moseley first assigned atomic num- |
||||
|
equivalent |
|
|
|
|||||
|
|
|
|
bers to elements by discovering that the square root of the |
|||||
HT |
Equivalent dose |
Sv (J kg−1) |
468 |
||||||
Kc |
Collision kerma |
J kg−1 |
440 |
frequency of the Kα photon is linearly related to Z. Solve |
|||||
L |
Length of object |
m |
|
452 |
Eq. 16.2 for Z and show that this is true. Plot Z vs the |
||||
N |
Number |
|
|
439 |
square root of the frequency and compare it to data you |
||||
OD |
Optical density |
|
|
441 |
|||||
|
|
look up. |
|
|
|
||||
P |
Probability |
|
|
462 |
|
|
|
||
|
|
|
|
|
|
||||


