
Biomolecular Sensing Processing and Analysis - Rashid Bashir and Steve Wereley
.pdf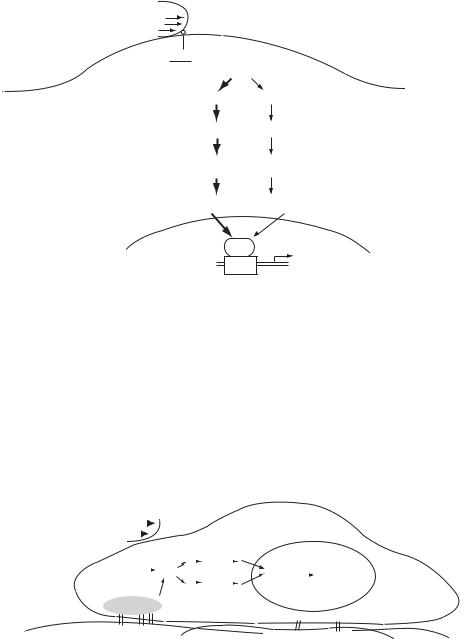
VASCULAR CELL RESPONSES TO FLUID SHEAR STRESS |
391 |
Once activated, p21ras triggers Raf-1 and MEKK (MAPK kinase kinase); in turn these stimulate ERK (extracellular signal regulated kinases) and JNK (c-Jun NH2-terminal kinases), respectively (Figure 18.8). ERK and JNK are MAPKs; ERK mediates cell growth while JNK mediates programmed cell death. When shear stress alone is the extracellular stimulus, JNK is activated to a much greater extent than ERK. In the case of JNK activation, c-Jun is expressed and crosses into the nucleus where it interacts with the transcription factor AP-1. AP-1 then interacts with the 12-O-tetradecanoyl-phorbol-13-acetate-responsive element (TRE) which mediates gene expression [42]; for example, MCP-1 expression is mediated through TRE [72]. Activation of ERK1 and ERK2 result in up regulation of Elk-1, [28] which crosses into the nucleus to interact with SRE. In turn, SRE affects gene expression of such molecules as c-fos [85].
18.10.2. IKK-NF · κ B Pathway
The IKK-NK- κB pathway is likely initiated by the αvβ3 integrin, which is stimulated by shear stress as was previously discussed. NF·κB is a transcription factor which mediates gene expression [12]; laminar shear stress up regulates its transcriptional activity [73]. NF·κB activation requires phosphorylation and then degradation of the I κB proteins, which inhibit NF·κ B activity. This process is mediated by the IKKs (IkB kinases), which are in part mediated by αvβ3 integrin expression in response to flow (Bhullar, 1998). The IKKs phosphorylate I κB, which subsequently degrades, allowing NF κB to translocate into the nucleus where it affects gene expression. It has also been suggested that MEKK is capable of stimulating this pathway, demonstrating the intricate and complex network involved in mechanotransduction [42].
18.11. APPLICATIONS TO CLINICAL TREATMENT
Understanding these critical signaling mechanisms involved in disease progression may allow for the design of pharmacological treatments with increased efficacy. In addition, knowledge of the relationship between gene expression and cardiovascular disease development may lead to gene manipulation strategies to restore or prevent specific gene expression (Heiko, 2001). As an example, it may be possible to restore the effects of NO via ecNOS gene transfer. Whatever the strategy, ultimately, results obtained from the fluid shear stress studies outlined in this chapter will aid physicians in diagnosing and treating the clinical presentation of atherosclerosis.
18.12. SUMMARY
Vascular cell responses to hemodynamic forces and biochemical stimulation dictate vessel behavior. For this reason, endothelial cell responses to fluid flow have been widely studied using flow models (e.g., the parallel plate flow chamber) which allow scientists and engineers to investigate cell functions under well defined flows. In such models, cells sense the flow via surface receptors, which activate one to many intracellular signaling cascades, thereby affecting the cell nucleus. In turn, cell functions including cell growth,
392 |
JENNIFER A. McCANN, THOMAS J. WEBSTER, AND KAREN M. HABERSTROH |
mRNA expression, and protein production are altered. These responses are directly related to the flow environment; laminar fluid flow yields healthy/physiological cell functions, while disturbed flow patterns favor cardiovascular disease development. Understanding the relationships between such intracellular signaling pathways and cell functions in response to these flow types (through studies such as those outlined in this chapter) will aid in understanding disease initiation and progression, as well as in the development of clinical treatment strategies.
REFERENCES
[1]S. Akimoto, M. Mitsumata, T. Sasaguri, and Y. Yoshida. Circ. Res., 86:185, 2000.
[2]B.R. Alevriadou, S.G. Eskin, L.V. McIntire, and W.P. Schilling. Ann. Biomed. Eng., 21:1, 1993.
[3]S.N. Alshihabi, Y.S. Chang, J.A. Frangos, and J.M. Tarbell. Biochem. Biophys. Res. Commun., 224:808, 1996.
[4]American Heart Association. (2002) Heart and Stroke Statistical Update. Dallas, Texas, American Heart Association, 2001.
[5]J. Ando, H. Tsuboi, R. Korenga,Y. Takada, N. Toyama-Sorimachi, M. Miyasaka, and A. Kamiya. Am. J. Physiol. Cell Physiol., 267:679, 1994.
[6]A.E. Aplin, S.M. Short, and R.L. Juliano. J. Biol. Chem., 274:31223, 1999.
[7]O. Araim, A.H. Chen, and B. Sumpio. New Surgery, 1:92, 2001.
[8]M.A. Awolesi, W.C. Sessa, and B.E. Sumpio. J. Clin. Invest., 96:1449, 1995.
[9]X. Bao, C. Lu, and J.A. Frangos. Arterioscler. Thromb. Vascul. Biol., 19:996, 1999.
[10]R.M. Berne and M.N. Levy. Physiology, (4th Ed.), Chapters 21 and 25, Mosby Inc, St. Louis, 1998.
[11]I.S. Bhullar, Y.S. Li, H. Miao, E. Zandi, M. Kim, J.Y. Shyy, and S. Chien. J. Biol. Chem., 273:30544, 1999.
[12]D.R. Blake, P.G. Winyard, and R. Marok. Ann. NY Acad. Sci., 723:308, 1994.
[13]G.J. Blake and P.M. Ridker. Circ. Res., 89:763, 2001.
[14]S.R. Bussolari, C.F. Dewey, and M.A. Gimbrone. Rev. Sci. Instrum., 53:1851, 1982.
[15]C.G. Caro, J.M. Fitz-Gerald, and R.C. Schroter. Proc. Roy. Soc. Lond. Ser. B: Biol. Sci., 177:109, 1971.
[16]J.A. Carosi, S.G. Eskin, and L.V. McIntire. J. Cell Physiol., 151:29, 1992.
[17]K.D. Chen, Y.S. Li, M. Kim, S. Li, S.Yuan, S. Chien, and J.Y.J. Shyy. J. Biol. Chem., 274:18393, 1999.
[18]B.J. Chung, A.M. Robertson, and D.G. Peters. Comp. Struct., 81:535, 2003.
[19]A. Cucina, A.V. Sterpetti, G. Pupelis, A. Fragale, S. Lepid, A. Cavallaro, Q. Giustiniani, and L.S. D’Angelo.
Eur J. Vasc. Sur., 9:86, 1995.
[20]P.F. Davies, A. Remuzzi, E.J. Gordon, C.F. Dewey, and M.A. Gimbrone. Proc. Natl. Acad. Sci., 83:2114, 1986.
[21]C.F. Dewey, S.R. Bussolari, M.A. Gimbrone, and P.F. Davies. J. Biomech. Eng., 103:177, 1981.
[22]S. Dimmeler, B. Fisslthaler, I. Fleming, C. Hermann, R. Busse, and A.M. Zeiher. Nature, 399:601, 1999.
[23]R.P. Dring. J. Fluids Eng., 104:15, 1982.
[24]A. Farzaneh-Far, J. Rudd, and P.L. Weissberg. Brit. Med. Bull., 59:55, 2001.
[25]J.A. Frangos, L.V. McIntire, and S.G. Eskin. Biotechnol. Bioeng., 32:1053, 1988.
[26]M.A. Freyberg, D. Kaiser, R. Graf, J. Buttenbender, and P. Friedl. Biochem. Biophys. Res. Commun., 286:141, 2001.
[27]M.G. Frid, E.C. Dempsey, A.G. Durmowicz, and K.R. Stenmark. Arteriosler. Thromb. Vascul. Biol., 17:1203, 1997.
[28]H. Gille, M. Kortenjann, O. Thomas, C. Moomaw, C. Slaughter, M.H. Cobb, and P.E. Shaw. Euro. Mol. Biol. Organ. J., 14:951, 1995.
[29]T. Gloe, S. Riedmayr, H.Y. Sohn, and U. Pohl. J. Biolog. Chem., 274:1599, 1999.
[30]S. Gudi, C.B. Clark, and J.A. Frangos. Circ. Res., 79:834, 1996.
[31]S. Gudi, J.P. Nolan, and J.A. Frangos. Proc. Natl. Acad. Sci., 95:2515, 1998.
[32]G.K. Hansson. Arteriosler. Thromb. Vascul. Biol., 21:1876, 2001.
[33]P.A. Holme, U. Orvim, M. Hamers, N.O. Solum, F.R. Brosstad, R.M. Barstad, and K.S. Sakariassen.
Arterioscler. Thromb. Vascul. Biol., 17:646, 1997.
VASCULAR CELL RESPONSES TO FLUID SHEAR STRESS |
393 |
[34]S. Jalali, Y.S. Li, M. Sotoudeh, S.Yuan, S. Li, S. Chien, and J.Y.J. Shyy. Arterioscler. Thromb. and Vascul. Biol., 18:227, 1998.
[35]L.M. Khachigian, N. Resnick, M.A. Gimbrone, and T. Collins. J. Clin. Invest., 96:1169, 1995.
[36]L.M. Khachigian, K.R. Anderson, N.J. Halnon, M.A. Gimbrone Jr., N. Resnick, and T. Collins. Arteriosler. Thromb. Vascul. Biol., 17:2280, 1997.
[37]L.W. Kraiss, A.S. Weyrich, N.M. Alto, D.A. Dixon, T.M. Ennis, V. Modur, T.M. McIntyre, S.M. Prescott, and G.A. Zimmerman. Am. J. Physiol. Heart Circulat. Physiol., 278:1537, 2000.
[38]M.J. Kuchan and J.A. Frangos. Am. J. Physiol. Heart Circulat. Physiol., 264:150, 1993.
[39]A.A. Lee, D.A. Graham, S.D. Cruz, A. Ratcliffe, and W.J. Karlon. J. Biomech. Eng., 124:37, 2002.
[40]S. Lehoux and A. Tedgui. Hypertension, 32:338, 1998.
[41]S. Li, M. Kim, Y.L. Hu, S. Jalali, D.D. Schlaepfer, T. Hunter, S. Chien, and J.Y.J. Shyy. J. Biolog. Chem., 272:30455, 1997.
[42]Y.S. Li, J.Y.J. Shyy, S. Li, J. Lee, B. Su, M. Karin, and S. Chien. Mol. Cell. Biol., 16:5947, 1996.
[43]J.K. Liao. Clin. Chem., 44:1799, 1998.
[44]D.M. Lloyd-Jones and K.D. Bloch. Ann. Rev. Med., 47:365 1996.
[45]A.J. Lusis. Nature, 407:233, 2000.
[46]A.M. Malek, A.L. Greene, and S. Izumo. Proc. Natl. Acad. Sci. USA, 90:5999, 1993.
[47]A.M. Malek, S.L. Apler, and S.I. Izumo. J. Am. Med. Assoc., 282:2035, 1999.
[48]J.A. McCann, S.D. Peterson, T.J.Webster, M.W. Plesniak, and K.M. Haberstroh. Ann. Biomed. Eng., 33:327, 2005.
[49]S.M. McCormick, S.G. Eskin, L.V. McIntire, C.L. Teng, C.M. Lu, C.G. Russell, and K.K. Chittur. Proc. Natl. Acad. Sci., 98:8995, 2001.
[50]S. Mohan, N. Mohan, and E.A. Sprague. Am. J. Physiol. Cell Physiol., 273:572, 1997.
[51]J.E. Moore and D.N. Ku. J. Biomech. Eng., 116:337, 1994.
[52]L. Moro, M. Venturino, C. Bozzo, L. Silengo, F. Altruda, L. Beguinot, G. Tarone, and P. Defilippi. Euro. Mol. Biol. Organ. J., 17:6622, 1998.
[53]T. Murase, N. Kume, R. Korenga, J. Ando, T. Sawamura, T. Masaki, and T. Kita. Circul. Res., 83:328, 1998.
[54]T. Nagel, N. Resnick, W.J. Atkinson, C.F. Dewey, and M.A. Gimbrone Jr. J. Clini. Invest., 94:885, 1994.
[55]E.A. Nauman, K.J. Risic, T.M. Keaveny, and R.L. Satcher. Ann. Biomed. Eng., 27:194, 1999.
[56]R.M. Nerem, P.R. Girard, G. Helmlinger, O. Thoumine, T.F. Wiesner, and T. Ziegler. Cell mechanics and cellular engineering. Cell Mechanics and Cellular Engineering, Chapter 5. Springer-Verlag, New York, 1994.
[57]M. Noris, M. Morigi, R. Donadelli, S. Aiello, M. Foppolo, M.Todeschini, G. Remuzzi, and A. Remuzzi. Circul. Res., 76:536–543, 1995.
[58]M. Ohno, J.P. Cooke, V.J. Dzau, and G.H. Gibbons. J. Clin. Invest., 95:1363, 1995.
[59]S.P. Olesen, D.E. Clapham, and P.F. Davies. Nature, 331:168, 1988.
[60]M. Papadaki, L.V. McIntire, and S.G. Eskin. Biotechnol. Bioeng., 50:555, 1996.
[61]E.M. Pederson, O. S. Agerbaek, and I.B. Kristensen. Euro. J. Vascul. Endovascul. Surg., 18:238, 1999.
[62]W.K. Purves, G.H. Orians, and H.C. Raig Heller. In Sinauer Associates and WH Freeman, Life: The Science of Biology, 4th Ed. New York, 1995.
[63]M. Raffel, C.Willert, and J.Kompenhans. Particle Image Velocimetry: A Practical Guide. Springer Press, Germany, 1998.
[64]G.E. Rainger and G.B. Nash. Circul. Res., 88:615, 2001.
[65]N.T. Resnick, T. Collins, W. Atkinson, D.T. Bonthron, C.F. Dewey Jr., and M.A. Gimbrone. Proc. Natl. Acad. Sci. USA, 90:4591, 1993.
[66]D.N. Rhoads, S.G. Eskin, and L.V. McIntire. Arteriosler. Thromb. Vascul. Biol., 20:416, 2000.
[67]M.J. Rieder, R. Carmona, J.E. Krieger, K.A. Pritchard, Jr, and A.S. Greene. Circul. Res., 80:312, 1997.
[68]H. Robenek and N.J. Severs. Cell Interactions in Atherosclerosis. CRC Press, Boca Raton, 1992.
[69a] R. Ross. Endothelial Dysfunction and Atherosclerosis. Plenum Press, New York, 1992. [69b] M. Samimy and S.K. Lele. Physics of Fluids A, 3:1915, 1991.
[70]E.A. Schwartz, R. Bizios, M.S. Medow, and M.E. Gerritsen. Circul. Res., 84:315, 1999.
[71]K. Shigematsu, H. Yasuhara, H. Shigematsu, and T. Muto. Internat. Angiol., 19:39, 2000.
[72]J.Y.J. Shyy, H.J. Hsieh, S. Usami, and S. Chien. Proc. Natl. Acad. Sci., 91:4678, 1994.
[73]J.Y.J. Shyy, M. Lin, J. Han, Y. Lu, M. Petrime, and S. Chien. Proc. Natl. Acad. Sci., 92:8069, 1995.
[74]J.Y.J. Shyy, Y.S. Li, M.C. Lin, W. Chen, S. Yuan, S. Usami, and S. Chien. J. Biomech., 28:1451, 1995.
394 |
JENNIFER A. McCANN, THOMAS J. WEBSTER, AND KAREN M. HABERSTROH |
[75]E.A. Sprague and J. Luo. Circulation, 90:I-84, (Abstract) 1994.
[76]A.V. Sterpetti, A. Cucina, L. Santoro D’Angelo, B. Cardillo, and A. Cavallaro. J. Cardiovascul. Surg., 33:619, 1992.
[77]A.V. Sterpetti, A. Cucina, A. Fragale, S. Lepidi, A. Cavallaro, and L. Santoro-D’Angelo. Euro. J. Vascul. Surg., 8:138, 1994.
[78]S. Tada and J.M. Tarbell. Am. J. Physiol. Heart Circulat. Physiol., 278:1589, 2000.
[79]S. Tada and J.M. Tarbell. Am. J. Physiol. Heart Circulat. Physiol., 282:576, 2001.
[80]M. Takahashi and B.C. Berk. J. Clini. Invest., 98:2623, 1996.
[81]J.N. Topper, J. Cai, D. Falb, and M.A. Gimbrone. Proc. Natl. Acad. Sci., 93:10417, 1996.
[82]J.N. Topper and M.A. Gimbrone. Mol. Med. Today, 5:40, 1999.
[83]O. Traub and B.C. Berk. Arterioscler. Thromb. Vascul. Biol., 18:677, 1998.
[84]R. Treisman. Trends Biochem. Sci., 17:423, 1992.
[85]H. Ueba, M. Kawakami, and T. Yaginuma. Arteriosler. Thromb. Vascul. Biol., 17:1512, 1997.
[86]M. Uematsu, Y. Ohara, J.P. Navas, K. Nishida, T.J. Murphy, R.W. Alexander, R.M. Nerem, and D.G. Harrison. Am. J. Cell Physiol., 269:1371, 1995.
[87]C. Urbich, D.H. Walter, A.M. Zeiher, and S. Dimmeler. Circul. Res., 87:683, 2000.
[88]J.R. Vane and R.M. Botting. J. Lipid Med., 6:395, 1993.
[89]H.E. von der Leyen and V.J. Dzau. Circulation, 103:2760, 2001.
[90]D.M. Wang and J.M. Tarbell. J. Biomech. Eng., 117:358, 1995.
[91]R.A. White. Atherosclerosis and Arteriosclerosis. CRC Press, Boca Raton, 1989.
[92]C.R. White, M. Haidekker, X. Bao, and J.A. Frangos. Circulation, 103:2508, 2001.
[93]T. Ziegler, P. Silacci, V.J. Harrison, and D. Hayoz. Hypertension, 32:351, 1998.
[94]T. Ziegler, K. Bouzourene, V.J. Harrison, and D. Hayoz. Arterioscler. Thromb. Vascul. Biol., 18:686, 1998.
About the Editors
Professor Mauro Ferrari is a pioneer in the fields of bioMEMS and biomedical nanotechnology. As a leading academic, a dedicated entrepreneur, and a vision setter for the Nation’s premier Federal programs in nanomedicine, he brings a three-fold vantage perspective to his roles as Editor-in-Chief for this work. Dr. Ferrari has authored or co-authored over 150 scientific publications, 6 books, and over 20 US and International patents. Dr. Ferrari is also Editor-in-Chief of Biomedical Microdevices and series editor of the new Springer series on Emerging Biomedical Technologies.
Several private sector companies originated from his laboratories at the Ohio State University and the University of California at Berkeley over the years. On a Federal assignment as Special Expert in Nanotechnology and Eminent Scholar, he has provided the scientific leadership for the development of the Alliance for Cancer Nanotechnology of the National Cancer Institute, the world-largest medical nanotechnology operation to date. Dr. Ferrari trained in mathematical physics in Italy, obtained his Master’s and Ph.D. in Mechanical Engineering at Berkeley, attended medical school at The Ohio State University, and served in faculty positions in Materials Science and Engineering, and Civil and Environmental Engineering in Berkeley, where he was first tenured. At Ohio State he currently serves as Professor of Internal Medicine, Division of Hematology and Oncology, as Edgar Hendrickson Professor of Biomedical Engineering, and as Professor of Mechanical Engineering. He is Associate Director of the Dorothy M. Davis Heart and Lung Research Institute, and the University’s Associate Vice President for Health Science, Technology and Commercialization.
Rashid Bashir completed his Ph.D. in 1992. From Oct 1992 to Oct 1998, he worked at National Semiconductor in the Process Technology Development Group as Sr. Engineering Manager. He is currently a Professor of Electrical and Computer Engineering and Courtesy Professor of Biomedical Engineering at Purdue University. He has authored or coauthored over 100 journal and conference papers, has over 25 patents, and has given over 30 invited talks. His research interests include biomedical microelectromechanical systems, applications of semiconductor fabrication to biomedical engineering, advanced semiconductor fabrication techniques, and nano-biotechnology. In 2000, he received the NSF Career Award for his work in Biosensors and BioMEMS. He also received the Joel and Spira Outstanding Teaching award from School of ECE at Purdue University, and the Technology Translation Award from the 2001 BioMEMS and Nanobiotechnology World Congress Meeting in
396 |
ABOUT THE EDITORS |
Columbus, OH. He was also selected by National Academy of Engineering to attend the Frontiers in Engineering Workshop in Fall 2003. https://engineering.purdue.edu/LIBNA
Professor Steve Wereley completed his masters and doctoral research at Northwestern University and joined the Purdue University faculty in August of 1999 after a two-year postdoctoral appointment at the University of California Santa Barbara in the Department of Mechanical and Environmental Engineering. At UCSB he focused exclusively on developing diagnostic techniques for microscale systems, work which ultimately led to developing, patenting, and licensing to TSI, Inc., the micro-Particle Image Velocimetry technique. His current research interests include designing and testing microfluidic MEMS devices, investigating biological flows at the cellular level, improving micro-scale laminar mixing, and developing new micro/nano flow diagnostic techniques. Professor Wereley has co-authored Fundamentals and Applications of Microfluidics, Artech House, 2002.

