
MusculoSkeletal Exam
.pdf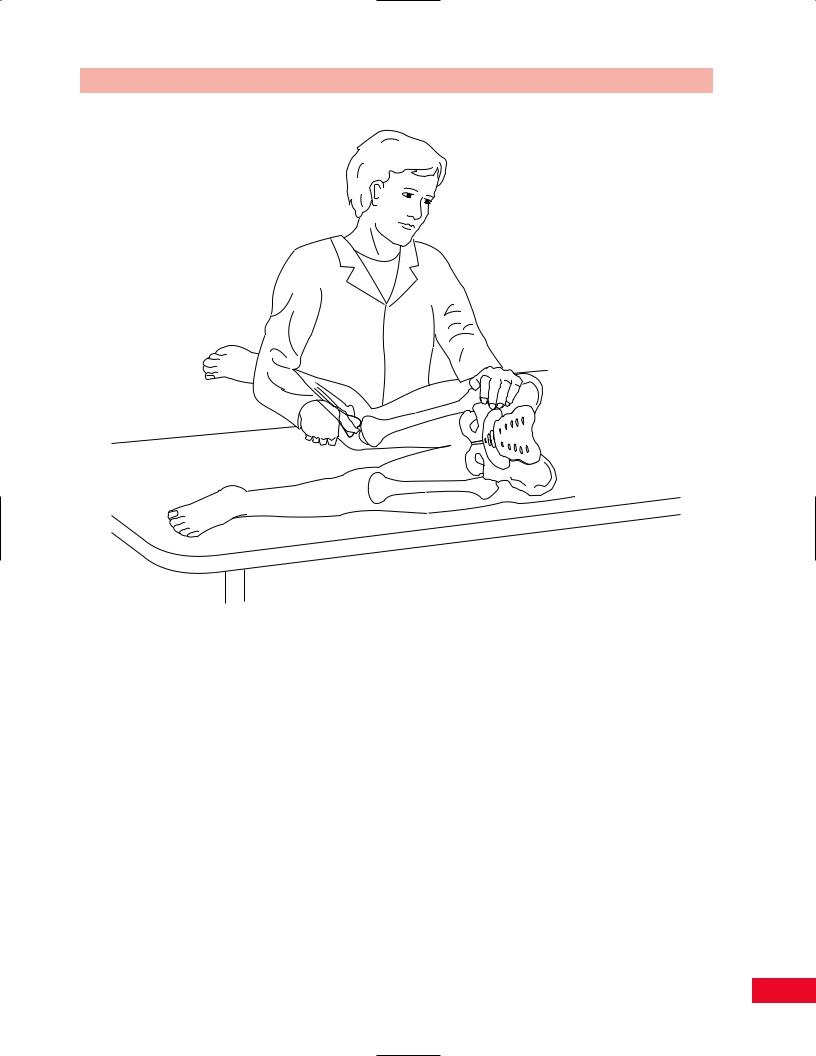
Chapter 6 The Lumbosacral Spine
Figure 6.62 The femoral stretch test. The test leg is extended at the hip first, and then the knee is flexed.
Tests to Increase Intrathecal Pressure
These tests are performed in an effort to determine whether the patient’s back pain is caused by intrathecal pathology, such as a tumor. By increasing the volume of the epidural veins, the pressure within the intrathecal compartment is elevated.
Valsalva’s Maneuver
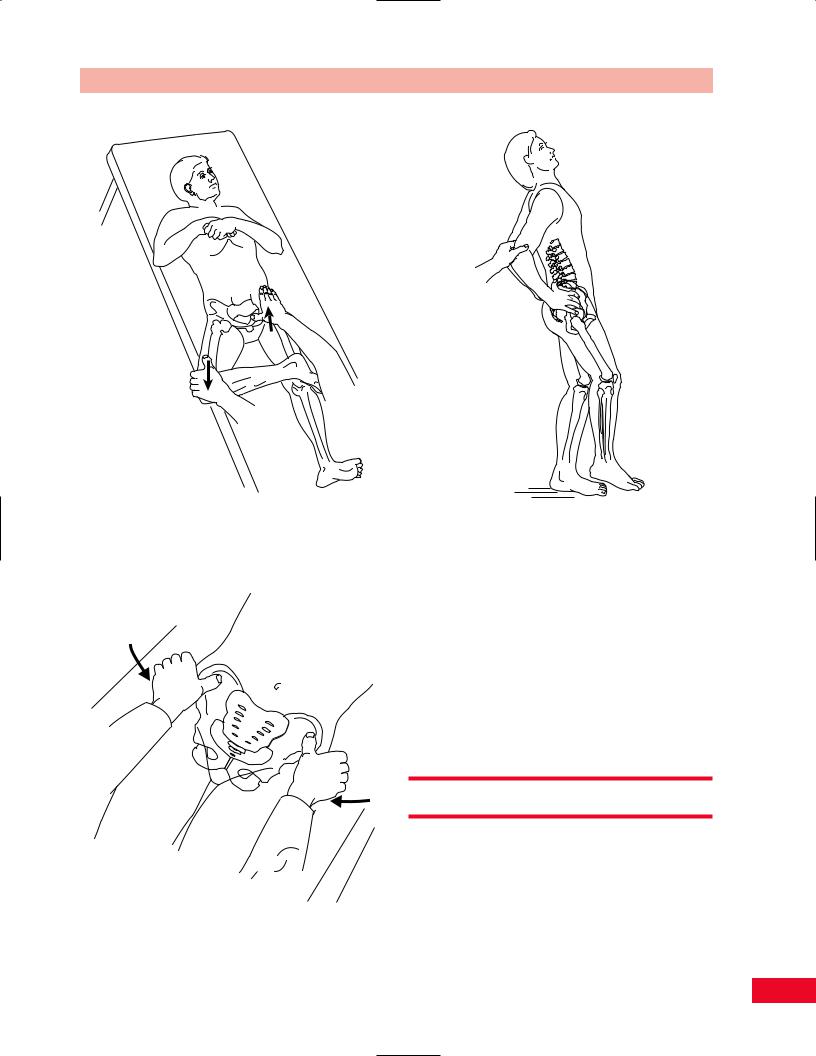
The patient is seated. Ask the patient to take a full breath and then bear down as if he or she were trying to have a bowel movement. This increases intrathecal pressure and may cause the patient to have increased back pain or increased pain down the legs. This is a positive Valsalva’s maneuver (Figure 6.63).
Sacroiliac Joint Tests
Gaenslen’s Sign
This test is used to determine ipsilateral sacroiliac joint disease by stressing the sacroiliac joint. The test is performed with the patient supine on the examining table with both knees flexed and drawn toward the chest. Move the patient toward the edge of the examining table so that one buttock (the test side) is off the table (Figure 6.64). Support the patient carefully and ask him or her to lower the free thigh and leg down to the floor (Figure 6.65). This stresses the sacroiliac joint, and if it is painful, the patient probably has sacroiliac joint dysfunction or pathology.
135

The Lumbosacral Spine Chapter 6
Figure 6.63 Valsalva’s maneuver.
Figure 6.65 Allow the patient’s thigh and leg to move downward to stress the sacroiliac join on that side. Pain on this maneuver reflects sacroiliac joint pathology.
Figure 6.64 Gaenslen’s sign. Bring the patient to the edge of the table with the test-side buttock over the edge.
Patrick’s (Fabere) Test
This test (Figure 6.66) is described in more detail on pp. 330–331. It is useful in determining whether there is sacroiliac joint pathology, as well as hip pathology. The patient is supine in a figure-of-four position. Press downward on the patient’s bent knee with one hand and with your other hand apply pressure over the iliac bone on the opposite side of the pelvis. This compresses the sacroiliac joint, and if it is painful, the patient has sacroiliac joint pathology. If pressure on the knee alone is painful, this indicates hip pathology on the same side.
Sacroiliac Distraction Test
This test is performed to distract the sacroiliac joints. The patient is lying supine and your thumbs are placed over the anterolateral aspect of the iliac crest bilaterally. With both hands, compress the pelvis toward the midline. The test result is positive for sacroiliac joint pathology if the patient complains of pain in the region of the sacroiliac joint (Figure 6.67).
136
Chapter 6 The Lumbosacral Spine
Figure 6.66 Patrick’s or Fabere test. The hip is flexed, abducted, |
Figure 6.68 Test for spondylolysis (extension in one-leg |
|
and externally rotated. |
||
standing). |
||
|
Figure 6.67 The sacroiliac distraction test. By compressing the pelvis medially and distracting the sacroiliac joints, this test determines whether sacroiliac pathology is present.
Spondylolysis Test (Extension in One-Leg Standing)
This test (Figure 6.68) is performed to identify a stress fracture of the pars interarticularis, which may cause a spondylolisthesis. Ask the patient to stand on one leg and extend the lumbar spine. If the patient complains of pain in the back, the test result is positive and may represent a stress fracture (spondylolysis). This posture stresses the facet joints and will also be painful if there is pathology of the facet joints.
Radiological Views
Radiological views are shown in Figures 6.69 through 6.74.
A= L2 vertebral body
B= L3/4 disc space
C= Spinous process
D= Transverse process
DG = Dorsal root ganglion of L2 in intervertebral foramen
137

Figure 6.69 Anteroposterior view of the |
Figure 6.71 Oblique view of the lumbosacral spine. |
lumbosacral spine. |
|
Figure 6.70 Lateral view of the lumbosacral |
Figure 6.72 Magnetic resonance image of the |
spine. |
lumbosacral spine, sagittal view. |

Chapter 6 The Lumbosacral Spine
E= Sacroiliac (S–I) joint ES = Erector spinae muscle
F= Articular facet
ID |
= Intervertebral disc |
L |
= Lamina of vertebral arch |
L5 |
= L5 Vertebral body |
N |
= Nerve root |
PI |
= Pars interarticularis |
PL |
= Pedicle |
S |
= Spinal canal, cauda equina (C) |
V |
= L2 vertebral body |
Figure 6.74 Magnetic resonance view of the lumbosacral spine, sagittal view.
Figure 6.73 Magnetic resonance image of the lumbosacral spine, transverse view.
139
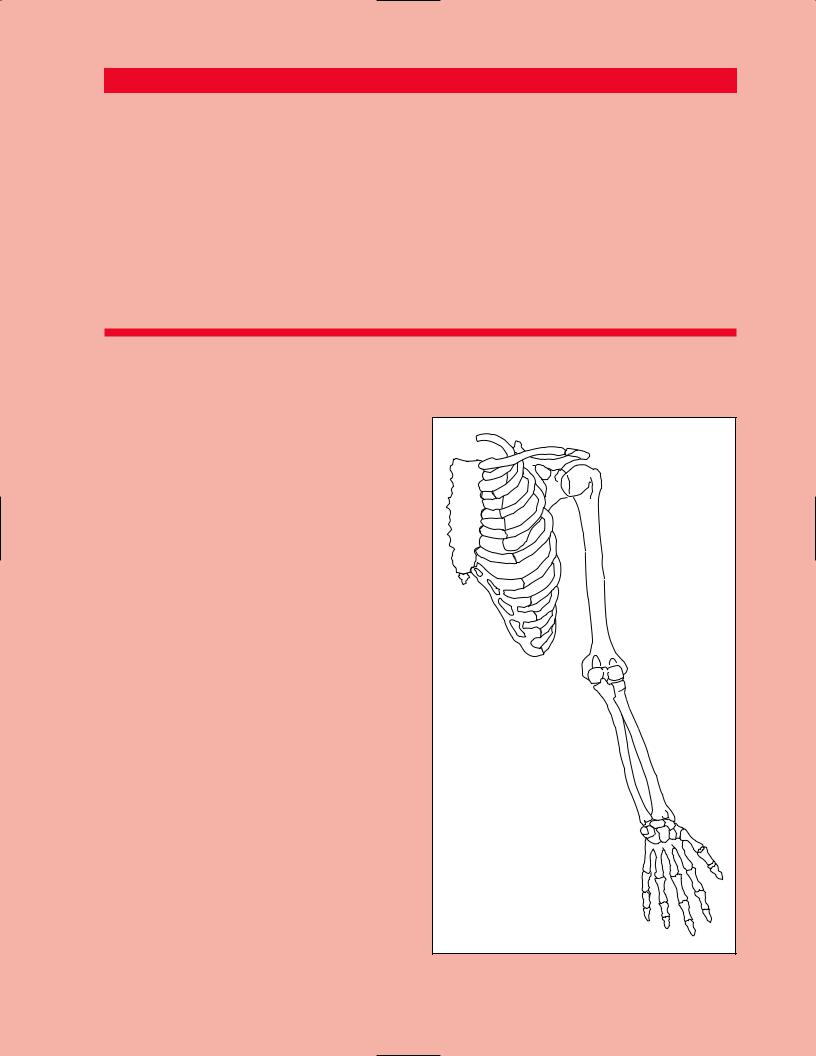
Chapter 7
Overview of the
Upper Extremity
The usefulness of the human upper extremity is defined by its complex end-organ, the hand. The sole purpose of the upper extremity is to position and move the hand in space. The upper extremity is attached to the remainder of the body through only one small articulation, called the sternoclavicular joint. Otherwise, it is suspended from the neck and held fast to the torso by soft tissues (muscles and fasciae). The clavicle, or collar bone, acts as a cantilever, projecting the upper extremity laterally and posteriorly from the midline. The upper extremity gains leverage against the posterior aspect of the thorax by virtue of the broad, flat body of the scapula. The scapula lies flatly on the posterior aspect of the thorax; as such, it is directed approximately 45 degrees forward from the midsagittal plane. At the superolateral corner of the scapula is a shallow socket, the glenoid. The glenoid is aligned perpendicularly to the body of the scapula. The socket faces obliquely forward and laterally. The spherical head of the humerus is normally directed posteromedially (retroverted 40 degrees) so as to be centered within the glenoid socket. The result is that the shoulder is a highly mobile, but extremely unstable configuration that permits a tremendous degree of freedom of movement in space (Figure 7.1).
Midway along the upper extremity, there is a complex modified hinge articulation called the elbow. As will be discussed, the elbow accommodates flexion as well as rotation movements of the forearm. Unlike the shoulder, the elbow has a much more stable configuration. The primary purpose of the elbow is to approximate the hand to other parts of the body, particularly the head.
At the terminus of the upper extremity is the hand. It is connected to the upper extremity by a complex hinge articulation termed the wrist. The wrist serves to modify the grosser movements of the elbow and shoulder. The importance of the wrist and complexity of the hand can best be appreciated when its function has been compromised. There is no single tool or appliance that can duplicate the function of the
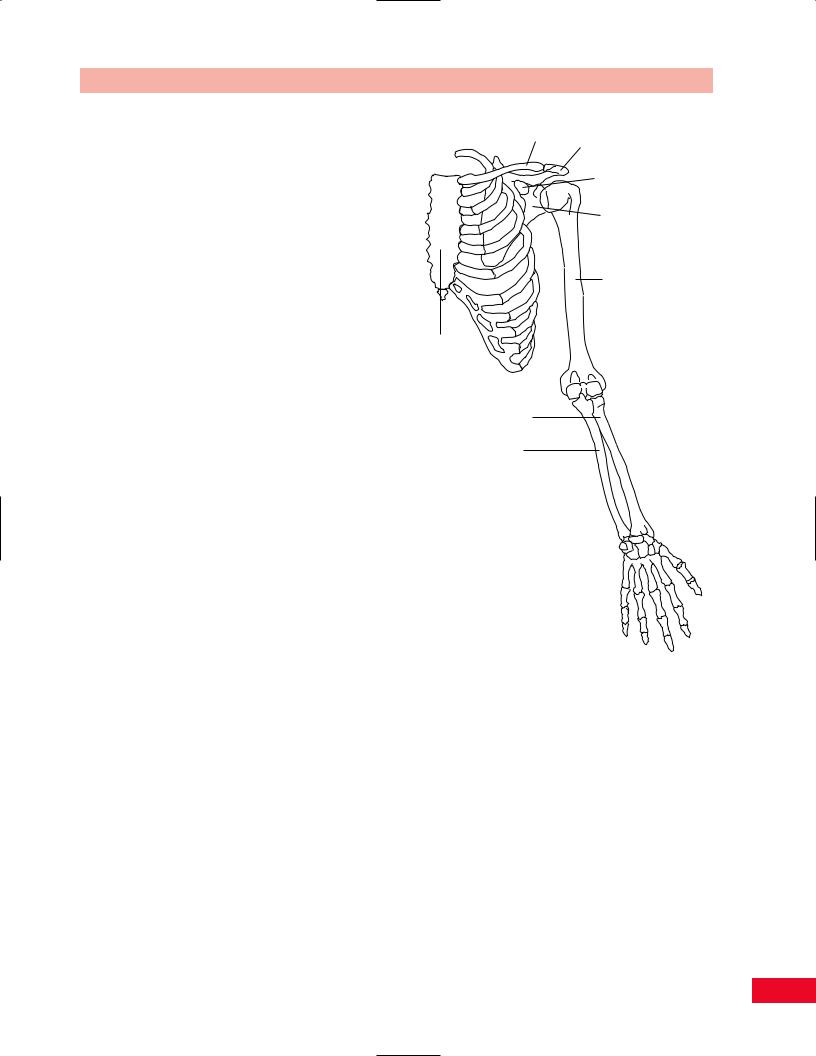
Chapter 7 Overview of the Upper Extremity
Clavicle Acromion
process
Corocoid process
Scapula
Humerus
Sternum
Radius
Ulna
Figure 7.1 Overview of the upper extremity.
hand. The disproportionate amount of motor cortex that the brain has allocated to control hand movements emphasizes both the hand’s importance and its complexity.
141
Chapter 8
The Shoulder
Sternum |
Acromion |
Clavicle
Coracoid
process
Scapula
Humerus
Xiphoid process
Please refer to Chapter 2 for an overview of the sequence of a physical examination. For purposes of length and to avoid having to repeat anatomy more than once, the palpation section appears directly after the section on subjective examination and before any section on testing, rather than at the end of each chapter. The order in which the examination is performed should be based on your experience and personal preference as well as the presentation of the patient.
Functional Anatomy
The shoulder contains four articulations: the sternoclavicular, the acromioclavicular, the scapulothoracic, and the glenohumeral.
The shoulder girdle facilitates the placement of the hand in space. It accomplishes this through the complementary movements of the scapula on the thorax and the glenohumeral articulation. This complementary movement is termed the scapulohumeral rhythm.
Historically, movements of the shoulder girdle have been subdivided into the specific responsibilities of each of the shoulder’s four articulations. However, such an artificial fragmentation of shoulder function is not an accurate portrayal of reality. In fact, under normal circumstances, the articulations work in synchrony, not isolation. The corollary of this fact is that the pathology of any single articulation will have significant adverse consequences on the functioning of the other remaining articulations and the entire upper extremity.
The entire upper extremity is attached to the torso through the small sternoclavicular articulation. It affords limited movement but must withstand significant loads. Therefore, it is not unusual to observe osteoarthritic degeneration of this joint, associated with significant soft-tissue swelling and osteophyte formation.
The acromioclavicular joint, like the sternoclavicular, is a small synovial articulation that has limited range of motion and frequently undergoes osteoarthritic degeneration. More importantly than in the case of the sternoclavicular joint, enlargement of the acromioclavicular articulation has significant adverse consequences on shoulder movement and integrity (see below).
The scapulothoracic articulation is a nonsynovial articulation. It is comprised of the broad, flat, triangular scapula overlying the thoracic cage and is separated
Chapter 8 The Shoulder
from the thoracic cage by a large bursa. Its stability is strictly dependent upon the soft tissue attachments of the scapula to the thorax. The plane of the scapula lies 45 degrees forward from the midcoronal plane of the body. Thus, the scapulothoracic articulation serves to supplement the large ball-and-socket articulation of the true shoulder joint.
The glenohumeral joint, or shoulder joint, is a shallow ball-and-socket articulation. As such, it enjoys tremendous freedom of movement. However, this freedom comes at a cost. It is inherently an unstable joint. The glenoid is so shallow that the ball (humeral head), if unprotected, can easily slip inferiorly out of the socket, creating a shoulder dislocation.
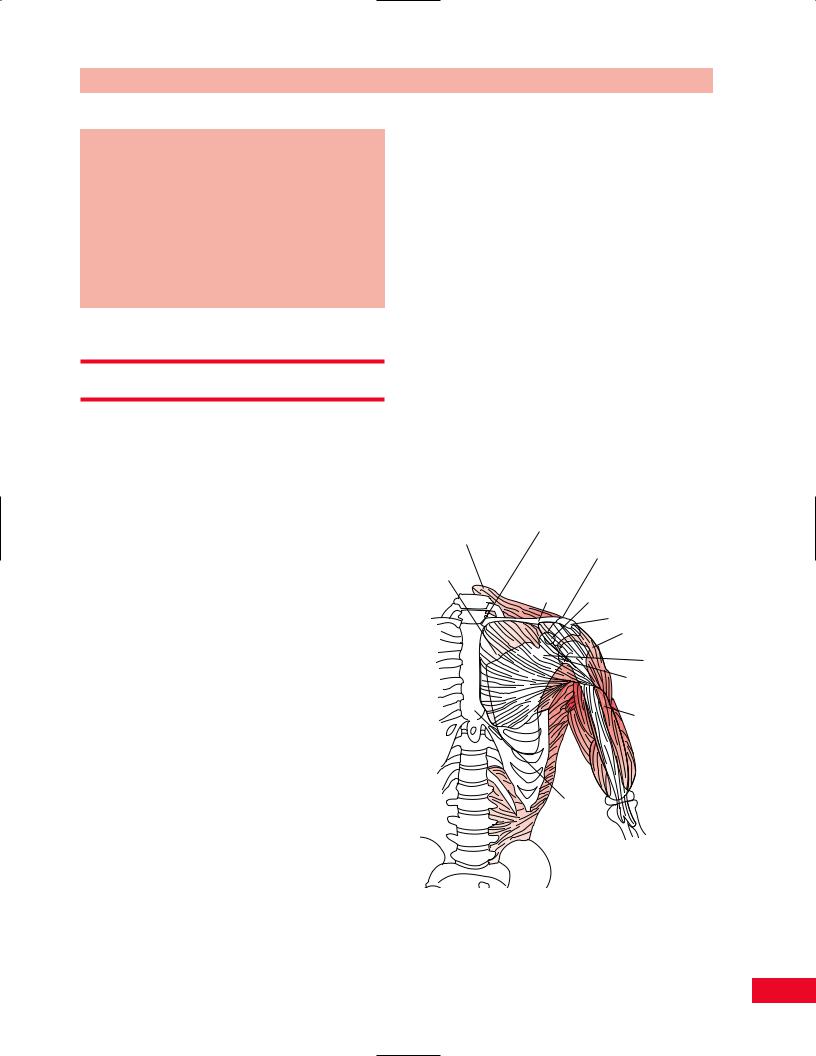
Normally, this is prevented by soft tissues (Figure 8.1). Anteriorly, there is the subscapularis tendon. Superiorly, there are the tendons of the supraspinatus and long head of the biceps. Posteriorly are the tendons of the infraspinatus and teres minor muscles. These tendons surround the humeral head, forming a “cuff,” and the corresponding muscles are responsible for rotating the humeral head within the glenoid socket. Hence, they are referred to as the rotator cuff. The purpose of
Trapezius Sternoclavicular joint muscle
Acromioclavicular joint
Pectoralis Major
Clavicle Coracoid process
Acromion Deltoid muscle
Scapula
Glenohumeral joint
Biceps muscle
Sternum
Figure 8.1 Overview of the shoulder showing the importance of the soft tissues in maintaining the round humeral head in the flattened glenoid process of the scapula. The other joints of the shoulder are also shown.
143

The Shoulder Chapter 8
Clavicle
Acromion
Inferior gleno-humeral ligament
Figure 8.2 Action of the humerus is limited by the acromion. Abduction force applied after this limit has been reached creates a fulcrum, forcing the humeral head inferiorly against the inferior glenohumeral ligament, thereby threatening glenohumeral stability.
the rotator cuff is to stabilize the humeral head within the glenoid socket, thereby creating a stable pivot point on which the larger shoulder muscles (deltoid and pectoralis major) can efficiently exert force.
The rotator cuff does not extend to the inferior (axillary) aspect of the glenohumeral articulation. Here, the only soft-tissue connection between the ball and socket is the capsular ligaments, the strongest of which is the inferior glenohumeral ligament. This ligament is important because as the arm moves overhead, abduction and external rotation of the humerus are limited by the acromion process (Figure 8.2). When the shaft of the humerus reaches the acromion, a fulcrum is created. Further attempts to abduct the arm will force the humeral head out of the glenoid socket inferiorly against the glenohumeral ligament. If the tolerance of the inferior capsular ligament to resist this movement is exceeded, either due to the magnitude of the acute force being applied or due to the inherent stretchability of a genetically determined lax ligament, a classic anterior–inferior shoulder dislocation will result (Figure 8.3). The consequent elongation of the inferior glenohumeral ligament is irreversible. Unless corrected, the glenohumeral joint becomes vulnerable to repeat episodes of instability with movement of the arm above the shoulder height (apprehension sign).
The superior aspect of the shoulder is protected by the acromioclavicular bony arch and the coracoacromial ligament (Figure 8.4). The latter represents the fibrous vestigial remnant of the coracoacromial bony arch of quadripeds. Beneath this protective roof passes the superior portion of the rotator cuff, the supraspinatus tendon and the long head of the biceps tendon. The biceps is the only part of the rotator cuff
Clavicle Acromion
Dislocation
Sternum |
Scapula Inferior |
|
gleno-humeral |
|
ligament |
Figure 8.3 Inferior dislocation of the glenohumeral articulation, with attenuation of the inferior glenohumeral ligament.
Supraspinatus |
|
muscle |
Acromion |
|
Clavicle
|
|
Humeral |
|
|
head |
Coracoid |
Coraco-acromial |
Biceps |
|
ligament |
tendon |
Figure 8.4 Superior view of the shoulder, showing the acromioclavicular joint and the coracoacromial ligament overlying the humeral head.
that depresses the humeral head. As the humerus moves, these tendons slide through a space defined by the bony-ligamentous roof above and the humeral head below (Figure 8.5). To reduce friction there is a bursal sac, the subacromial bursa, positioned between the tendons below and the roof above.
The subacromial space can be absolutely narrowed by osteophytes extending inferiorly from the clavicle, acromion, or acromioclavicular joint. Swelling of the soft tissues within the space (i.e., bursitis and tendinitis) can also relatively narrow the space. These soft-tissue swellings may arise as the result of acute injuries or chronic overuse syndromes. In either case, the result is insufficient space for the free passage of the rotator cuff beneath the coracoacromial arch. This creates a painful pinching of the tissues between the roof above and the humeral head below. This condition has been termed an impingement syndrome. The resulting pain
144
