
MusculoSkeletal Exam
.pdf
Chapter 4 The Cervical Spine and Thoracic Spine
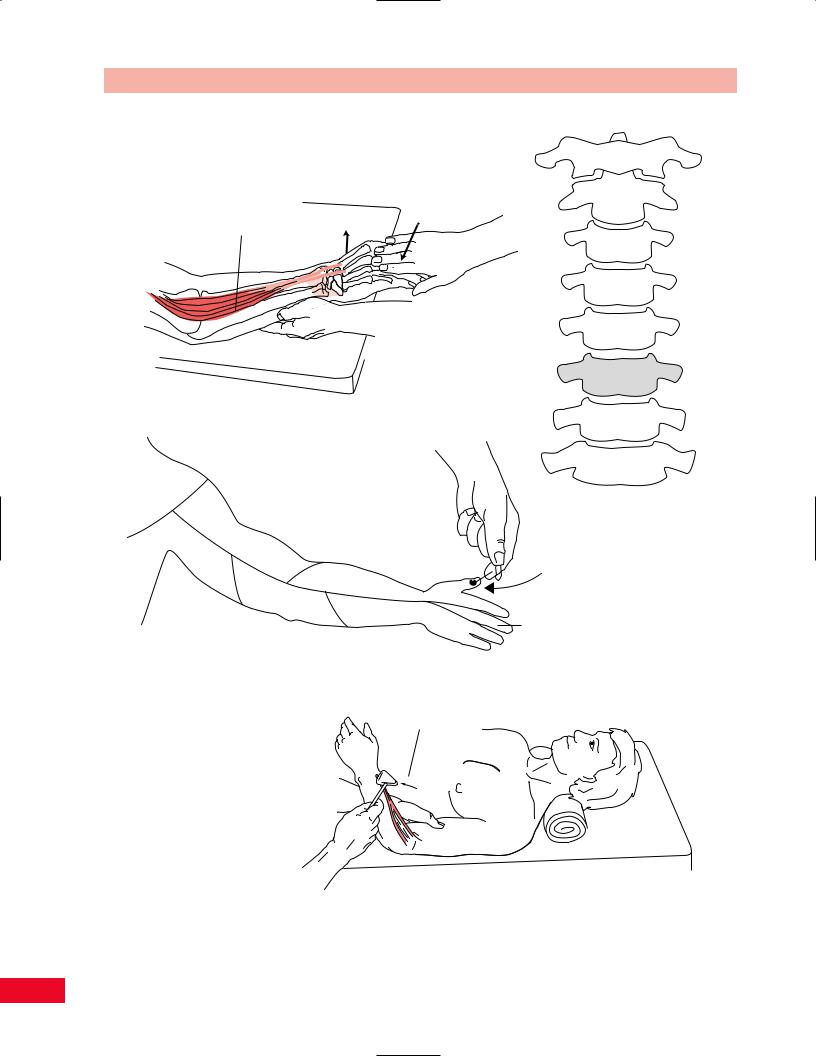
Figure 4.49 Mobility testing of the posteroanterior pressure on the transverse process.
vertebral body away from the side that you are contacting (Figure 4.49).
Transverse Pressure on the Spinous Process
Place the patient in the prone position with the neck in neutral rotation midway between flexion and extension. Stand on the side of the patient so that your dominant eye is centered over the spine, with your body turned so that you are facing the side of the patient. Place your thumbs on the lateral aspect of the spinous process. Push the process away from you until you have taken up all the slack. This will cause rotation of the vertebral body toward the direction that you are contacting (Figure 4.50).
First Rib Ventral-Caudal Glide
Place the patient in the sitting position either on a stool or on a low table, with the head and neck rotated to the right. Stand behind the patient. Support the patient by placing your left hand over the patient’s head and rest your elbow on the shoulder. Place the lateral aspect of your index finger of the right hand over the superiordorsal aspect of the first rib. Press in a ventral and caudal direction until all the slack is taken up (Figure 4.51).
Resistive Testing
Movements of the head and neck are flexion, extension, rotation, and lateral bending. Testing the strength of the cervical muscles is best performed with the patient in the seated position. Testing the cervical muscles with gravity eliminated is performed with the patient lying supine. Significant weakness of cervical muscles may be found in neuromuscular diseases such as myasthenia gravis and polymyositis.
Cervical Flexion
The sternocleidomastoid muscle is the primary cervical flexor. The scaleni anterior, medius, and posterior, as well as the intrinsic neck muscles (see Figure 4.4) assist it.
Position of the patient: Seated.
Resisted test (Figure 4.52): Place one of your hands on the patient’s sternum to prevent substitution of neck flexion by flexion of the thorax. Place the palm of your other hand on the patient’s forehead and ask the patient to bring the head downward so as to look
65

The Cervical Spine and Thoracic Spine Chapter 4
Figure 4.50 Mobility testing of transverse pressure on the spinous process.
Movement
First rib
 Resistance
Resistance
Figure 4.51 Mobility testing of first rib ventral-caudal glide. |
Figure 4.52 Testing cervical flexion. |
66
|
Chapter 4 The Cervical Spine and Thoracic Spine |
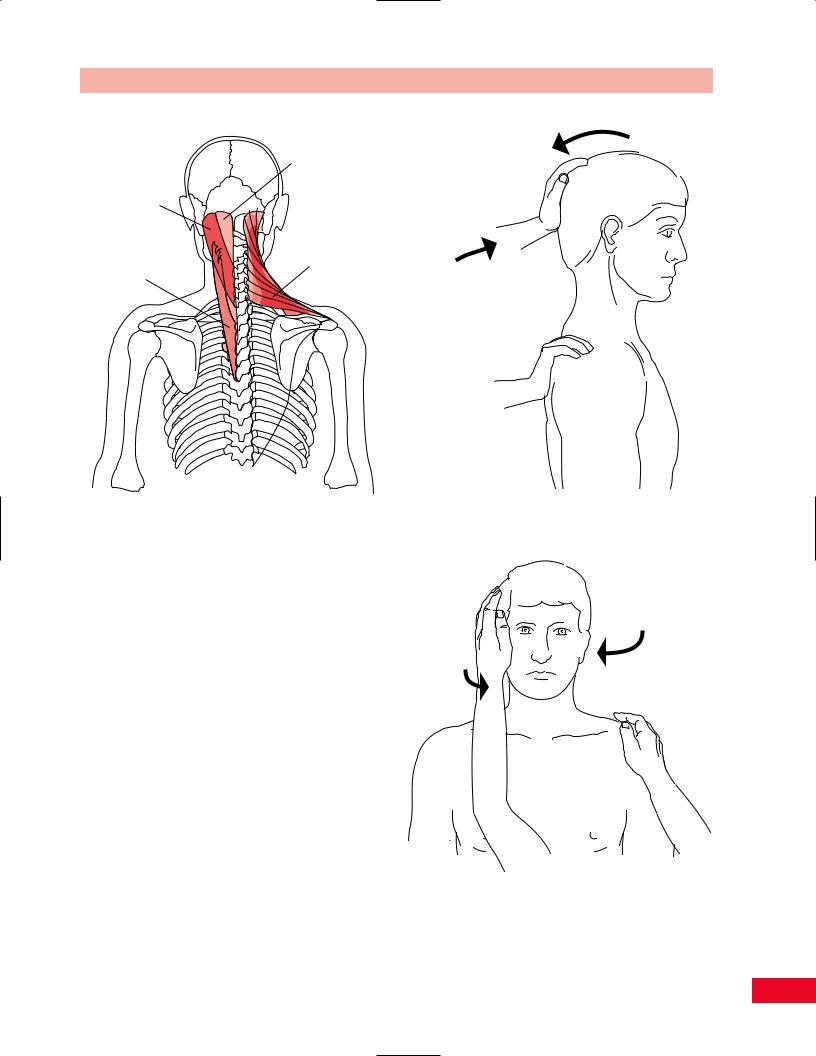
Semispinalis |
Movement |
capitis |
|
muscle |
|
Splenius capitis muscle
Trapezius muscle (superior fibers)
Splenius cervicis |
Resistance |
muscle |
|
Figure 4.53 The cervical extensors. |
Figure 4.54 Testing cervical extension. |
|
at the floor. Resist this movement with your hand as he or she pushes against you.
Cervical Extension
The primary extensors of the cervical spine are the trapezius (superior fibers), the semispinalis capitis, splenius capitis, and splenius cervicis (Figure 4.53). These muscles are assisted by the levator scapulae and the intrinsic neck muscles.
•Position of patient: Seated. Stand behind the patient.
•Resisted test (Figure 4.54): Place one hand on the patient’s shoulder over the scapula for stabilization.
Place your other hand over the occiput and vertex of the patient’s skull and ask the patient to bring the head backward as he or she tries to look to the ceiling, against your resistance. The patient may attempt to lean backward and you should resist this movement with your stabilizing hand.
Movement
Resistance
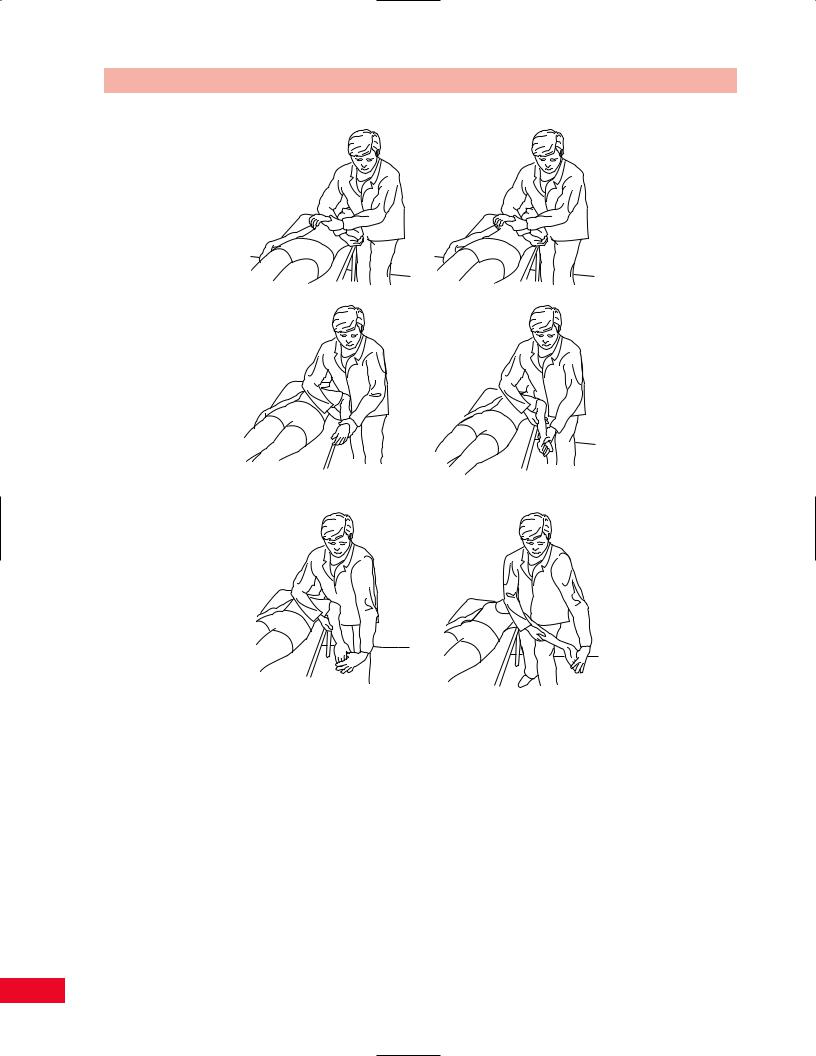
Rotation (see Figure 4.55)
The sternocleidomastoid muscle is the prime rotator of the cervical spine. The right sternocleidomastoid rotates the head to the left (Figure 4.4).
Figure 4.55 Testing lateral rotation. Resisting rotation of the head to the left tests the right sternocleidomastoid muscle.
67

The Cervical Spine and Thoracic Spine Chapter 4
•Position of patient: Seated, with you in front of the patient.
•Resisted test (Figure 4.55): To test the left sternocleidomastoid muscle, you should resist right rotation of the head as follows. Place your right hand on the patient’s left shoulder to stabilize the torso. Cup your left hand and place it so that the patient’s chin is in the palm
of your hand and your fingers cover the patient’s cheek. Ask the patient to rotate the head in
a horizontal plane against the resistance of your left hand.
Weakness of the sternocleidomastoid muscle may
be due to damage to the spinal accessory nerve. Compare left and right rotation.
Lateral Bending
The primary muscles of lateral bending are the scaleni muscles, and the intrinsic muscles of the neck assist them. Lateral bending is not a pure motion and occurs in conjunction with rotation of the cervical spine (see Figure 4.4).
•Position of patient: Seated, with you at the side.
•Resisted test (Figure 4.56): Test right lateral bending by placing your right hand on the patient’s right shoulder to stabilize the torso. Place your left hand over the temporal aspect
Movement |
Resistance |
|
Figure 4.56 Testing lateral bending.
of the skull above the ear and ask the patient to tilt the ear toward the shoulder as you resist this motion. Compare your findings with those of the opposite side.
Neurological Examination of the
Cervical Spine and Upper Extremity
The Brachial Plexus
The brachial plexus (Figure 4.57) is composed of the C5, C6, C7, C8, and T1 nerve roots. In some individuals, C4 is included, and this is referred to as a prefixed brachial plexus. In others, T2 is included, and this is called a postfixed brachial plexus.
During embryogenesis, the upper limb bud rotates so that the upper nerve roots, C5 and C6, become lateral in the arm, and the lower nerve roots, C8 and T1, become medial in the arm.
The five nerve roots that form the plexus join to form three trunks. C5 and C6 form the upper trunk, C7 forms the middle trunk, and C8 and T1 join to form the lower trunk. The trunks are located at the level of the clavicle.
Each trunk splits into an anterior and posterior division. The posterior divisions of the three trunks join to form the posterior cord. The anterior divisions of the upper and middle trunks form the lateral cord, and the anterior division of the lower trunk continues on as the medial cord. The names posterior, lateral, and medial cords are based on their relationship to the second part of the axillary artery and the axilla.
Portions of the lateral and medial cords join to form the median nerve. The lateral cord continues on as the musculocutaneous nerve, and the medial cord continues on as the ulnar nerve. The posterior cord branches into the axillary and radial nerves.
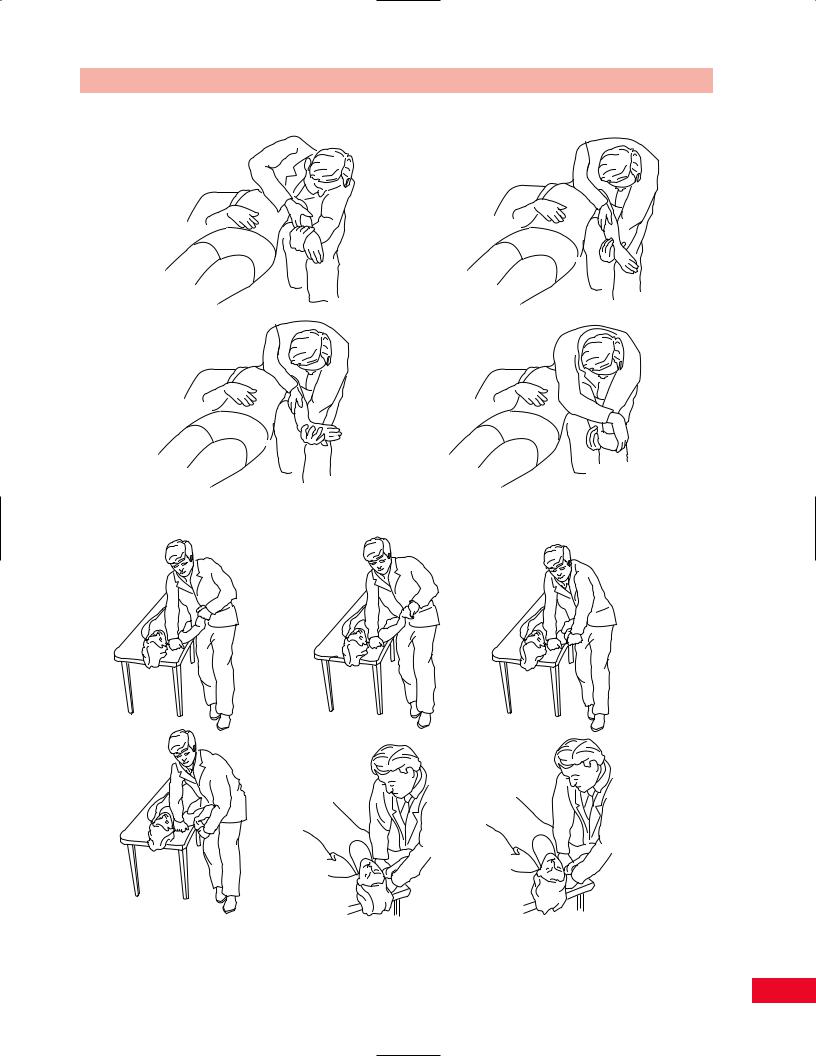
Upper Limb Tension Test (Brachial
Plexus Tension Test, Elvey’s Test)
Performing a stretch test can test the component nerves of the brachial plexus.
Median Nerve
The patient is supine with the scapula unobstructed. Depress the shoulder and maintain the position. Extend the elbow and externally rotate the upper extremity.
68

Chapter 4 The Cervical Spine and Thoracic Spine
C5
Roots |
|
Trunks |
Divisions |
|
|
Scapular |
|
|
Dorsal |
Suprascapular |
|
|
|
|
|
|
|
Upper |
|
Lateral
Cords
pectoral
Lateral
Branches
Musculocutaneous
C6 |
Second part of |
|
the axillary artery |
||
|
||
Clavicle |
|
|
Middle |
Posterior |
|
C7 |
|
|
Lower |
|
Upper |
|
Thoracodorsal |
C8 |
subscapular |
subscapular |
Lower |
Medial |
|
Axillary
Radial
Median
Ulnar
Medial |
MedialMedial |
T1 |
|
pectoral |
brachial |
|
antebrachial |
Posterior divisions Anterior divisions
cutaneous
Long thoracic nerve
cutaneous
Roots |
Trunks |
Divisions |
Cords |
Branches |
Figure 4.57 The brachial plexus. The anterior divisions of the upper and middle trunks form the lateral cord and the anterior division of the lower trunk forms the medial cord. The three posterior divisions of the trunk form the posterior cord.
Then extend the wrist, fingers, and thumb. If nerve root irritation is present, local palpation of the nerve will increase the symptoms (Butler, 1991) (Figure 4.58).
Radial Nerve
The patient is supine with the scapula unobstructed. Depress the shoulder and maintain the position. Extend the elbow and internally rotate the upper extremity. Then flex the wrist. Adding ulnar deviation and flexion of the thumb can enhance the position. If nerve root irritation is present, local palpation of the nerve will increase the symptoms (Butler, 1991) (Figure 4.59).
Adding cervical lateral bending away from the side being tested and some adduction or extension of the shoulder can enhance both tests.
Ulnar Nerve
The starting position is the same as for the median nerve. Extend the patient’s wrist and supinate the
forearm. Then fully flex the elbow and depress the shoulder. Add external rotation and abduct the shoulder. The neck can be placed in lateral bending (Figure 4.60).
The patient will likely complain of numbness or pain in the thumb, index, and middle fingers. This is a normal response. In 70% of normal patients, lateral bending away from the test side will exacerbate the symptoms (Kenneally et al., 1988). The test is abnormal if the patient notes symptoms in the ring and little finger while the head is in neutral. To confirm that the findings are secondary to root irritation, slacken the position of one of the peripheral joints and then side bend the neck. If the symptoms return, the nerve root is probably the source (Kaltenborn, 1993).
Note that these maneuvers will be painful if there is concomitant disease of the joints, ligaments or tendons being mobilized. Refer to other chapters for specific tests of these important structures.
69
The Cervical Spine and Thoracic Spine Chapter 4
depression
elbow |
whole arm |
extension |
lateral rotation |
wrist and finger |
shoulder |
extension |
abduction |
Figure 4.58 The median nerve stretch test. Adapted from Butler DS. Mobilisation of the Nervous System. Melbourne: Churchill Livingstone, 1991.
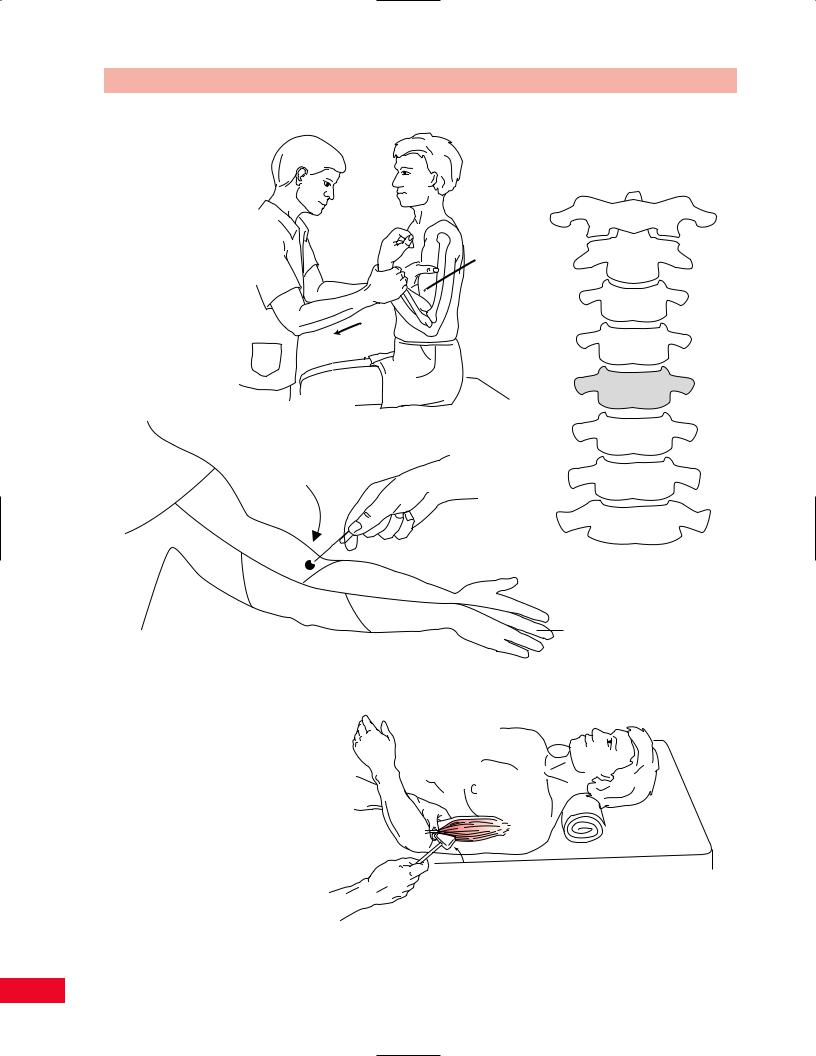
Neurological Testing by Root Level
Neurological examination of the upper extremity is required to determine the location of nerve root impingement or damage in the cervical spine, as may be caused by spondylosis or a herniated disc. By examining the motor strength, sensation, and reflexes in the upper extremities, you can determine the root level that is functioning abnormally. Recall that in the cervical spine, the C1 through C7 nerves exit above the vertebrae of the same number. The C8 nerve root exits between the C7 and T1 vertebral bodies, and the T1 nerve root exits below the T1 vertebral body.
Key muscles, key sensory areas, and reflexes are tested for each root level.
The C5 Root Level
Motor
The biceps muscle, which flexes the elbow, is innervated by the musculocutaneous nerve and represents the C5 root level (Figure 4.61). Many authors also consider the deltoid muscle, innervated by the axillary nerve, to be a key C5 muscle. The patient flexes the elbow with the forearm fully supinated. Resist this movement with your hand placed on the anterior
70
Chapter 4 The Cervical Spine and Thoracic Spine
starting position, shoulder depression, elbow extension
as for median nerve
wrist flexion (gently)
Figure 4.59
wrist and finger extension, then pronation or supination (pronation more sensitive)
shoulder lateral rotation
whole arm internal rotation
wrist flexion (alternate position)
The radial nerve stretch test.
elbow flexion
shoulder |
cervical lateral |
abduction |
flexion |
Figure 4.60 The ulnar nerve stretch test. Adapted from Butler DS. Mobilisation of the Nervous System. Melbourne: Churchill Livingstone, 1991.
71
The Cervical Spine and Thoracic Spine Chapter 4
Motor |
C5 |
|
 Movement
Movement
Resistance
C5
Sensation
Key C5 sensory area
C5
T2
T1 |
C6 |
C8 |
C7 |
Anterior view
Reflex
Figure 4.61 The C5 root level.
72

Chapter 4 The Cervical Spine and Thoracic Spine
aspect of the midforearm (see pp. 217–218 for further information).
Sensation
The key sensory area for C5 is the lateral antecubital fossa.
Reflex
The biceps reflex is tested by placing your thumb on the biceps tendon as the patient rests his or her forearm on yours. Take the reflex hammer and tap your thumb briskly and observe for contraction of the biceps and flexion of the elbow (see pp. 221–222 for further information).
The C6 Root Level
Motor
The wrist extensors (extensor carpi radialis longus and brevis) are innervated by the radial nerve and represent the C6 root level (Figure 4.62). Test wrist extension by having the patient pronate the forearm and raise his or her hand, as if to say “Stop.” Resist this motion with your hand against the posterior aspect of the metacarpals (see pp. 263–265 for further information).
Sensation
The key sensory area for C6 is the anterior distal aspect of the thumb.
Reflex
The brachioradialis reflex is used to test the C6 nerve root level. To test this reflex, have the patient rest the forearm over yours, with the elbow in slight flexion. Use the flat end of the reflex hammer to tap the distal part of the radius. The test result is positive when the brachioradialis muscle contracts and the forearm jumps up slightly (see pp. 221–222 for further information). The biceps reflex can also be tested to evaluate the C6 root level because both the C5 and C6 roots innervate the biceps nerve roots.
The C7 Root Level
Motor
Elbow extension (triceps brachii) is examined to test the C7 root level (Figure 4.63). The triceps is innervated by the radial nerve. Testing elbow extension is performed by having the patient lie supine with the shoulder flexed to 90 degrees and the elbow flexed. Stabilize the arm with one hand placed just proximal to the elbow and apply a downward flexing resistive
force with your other hand placed on the forearm just proximal to the wrist. Ask the patient to extend the hand upward against your resistance (see pp. 217–218 for further information).
Sensation
The key sensory area for C7 is located on the anterior distal aspect of the long finger.
Reflex
The triceps reflex tests the C7 nerve root level. This test is performed by having the patient’s forearm resting over yours. Hold the patient’s arm proximal to the elbow joint with your hand, to stabilize the upper arm. Ask the patient to relax. Tap the triceps tendon with the reflex hammer just proximal to the olecranon process. The test result is positive when a contraction of the triceps muscle is visualized (see pp. 222–223 for further information).
The C8 Root Level
Motor
The long flexors of the fingers (flexor digitorum profundus), which are innervated by the median and ulnar nerves, are tested to evaluate the C8 root level (Figure 4.64). Finger flexion is tested by asking the patient to curl the second through fifth fingers toward the palm as you place your fingers against the patient’s palmar finger pads to prevent him or her from forming a fist (see p. 266 for further information).
Sensation
The key sensory area for C8 is located over the anterior distal aspect of the fifth finger.
Reflex
The finger flexor jerk is not often tested. The reader is referred to neurological textbooks for further information regarding this reflex.
The T1 Root Level
Motor
The small and index finger abductors (abductor digiti quinti, first dorsal interosseous) are tested to evaluate the T1 root level (Figure 4.65). These muscles are innervated by the ulnar nerve. The patient is examined with the forearm pronated. Ask the patient to spread the fingers apart as you apply resistance to this movement against the outer aspects of the proximal phalanges of the index and little fingers (see pp. 269–271 for further information).
73
The Cervical Spine and Thoracic Spine Chapter 4
C6
Motor
Wrist extension (extensor carpi |
Resistance |
radialis longus and brevis) |
Movement |
C6
Sensation
C5 |
|
|
T2 |
|
Key C6 |
|
|
sensory area |
T1 |
C6 |
|
Anterior view |
C8 |
C7 |
|
|
Reflex |
Brachioradialis reflex |
|
Figure 4.62 The C6 root level.
74
