
MusculoSkeletal Exam
.pdf
Chapter 6 The Lumbosacral Spine
Figure 6.33 Mobility testing of the sacroiliac joint: standing forward-bending test.
Press on the process in an anterior direction until all the slack has been taken up. This will cause a rotation of the vertebral body away from the side that you are contacting (Figure 6.31).
Transverse Pressure on the Spinous Process
Place the patient in the prone position with the neck in neutral rotation. Stand on the side of the patient that is on the side of your dominant eye, with your body turned so that you are facing the side of the patient. Place your thumbs on the lateral aspect of the spinous process. Push the process away from you until you have taken up all the slack. This will cause rotation of the vertebral body towards you (Figure 6.32).
Sacroiliac Joint Examination
After concluding the examination of the lumbar intervertebral mobility tests and accessory movements, proceed with the examination of the sacroiliac joint.
Standing Flexion Test
This is a mobility test for the ilium moving on the sacrum. Instruct the patient to stand with the feet approximately 6 in. apart. Stand behind the patient to observe the movement. Remember to use your dominant eye. Locate the posterior superior iliac spines and place your thumbs under them. Maintain contact with the posterior superior iliac spines throughout the movement. Ask the patient to bend as far forward as he or she can. Observe the movement of the posterior superior iliac spines in relation to each other. They should move equally. If there is a restriction, then the side that moves first and furthest is considered to be hypomobile (Figure 6.33). If the patient presents with tight hamstrings, a false-positive finding can occur (Greenman, 1996; Bourdillon et al., 1992).
Stork (Gillet, Marching) Test
This is a mobility test for the ilium moving on the sacrum. Instruct the patient to stand with the feet
115

The Lumbosacral Spine Chapter 6
approximately 6 in. apart. Stand behind the patient to observe the movement. Remember to use your dominant eye. Locate the posterior superior iliac spine on the side that you are testing and place one thumb under it. Place your other thumb just medial to the posterior superior iliac spine, on the sacral base. Ask the patient to raise the lower extremity on the side being tested so that the hip and knee are flexed to 90 degrees. Note the movement of the posterior superior iliac spine in relation to the sacrum. This test should be repeated on the contralateral side. Compare the amount of movement from one side to the other. If the posterior superior iliac spine does not drop down into your thumb on one side, the ilium is considered to be hypomobile (Greenman, 1996; Bourdillon et al., 1992) (Figure 6.34).
Backward-Bending Test
Instruct the patient to stand with the feet approximately 6 in. apart. Stand behind the patient to observe the movement. Remember to use your dominant eye. Place your thumbs medial to the posterior superior iliac spines bilaterally on the sacral base. Instruct the patient to bend backward. Observe as your thumbs move in an anterior direction. An inability to move anteriorly demonstrates hypomobility of the sacrum moving on the ilium (Greenman, 1996; Bourdillon et al., 1992) (Figure 6.35).
Seated Flexion Test
This is a mobility test for the sacrum moving on the ilium. This test eliminates the influence of the lower extremities. Instruct the patient to sit on a stool with the feet firmly on the ground for support. Stand behind the patient to observe the movement. Remember to use your dominant eye. Locate the posterior superior iliac spines and place your thumbs under them. Maintain contact with the posterior superior iliac spines throughout the movement. Ask the patient to bend as far forward as he or she can with their arms between their knees. Observe the movement of the posterior
|
Figure 6.35 Mobility testing of the sacroiliac joint: backward- |
Figure 6.34 Mobility testing of the sacroiliac joint: stork test. |
bending test. |
116
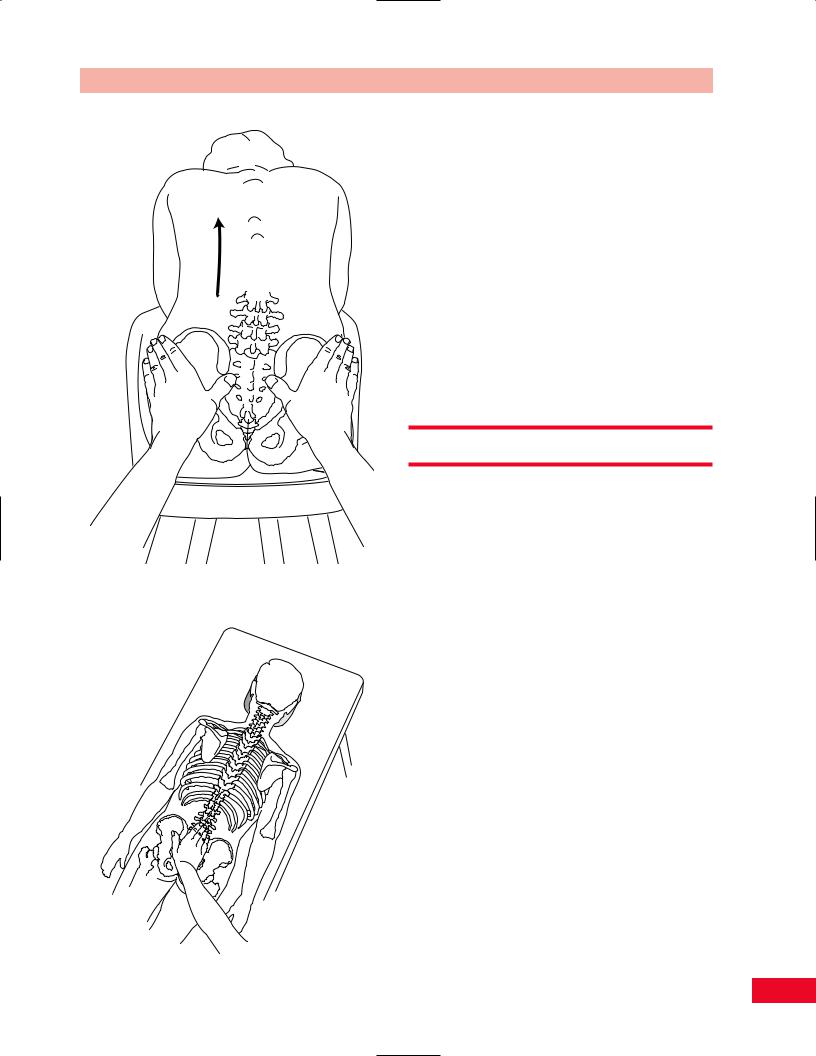
Figure 6.36 Mobility testing of the sacroiliac joint: sitting forward-bending test.
Chapter 6 The Lumbosacral Spine
superior iliac spines in relation to each other. The side that moves first and furthest is considered to be hypomobile (Greenman, 1996; Bourdillon et al., 1992) (Figure 6.36).
Posteroanterior Spring of the Sacrum
This a test for posterior to anterior mobility of the sacrum. Place the patient in the prone position with the neck in neutral rotation. Stand on the side of the patient that is on the side of your dominant eye, with your body turned so that you are facing the patient’s head. Place your hands over the central aspect of the posterior sacrum using the palm as the contact point. Press directly over the sacrum in an anterior direction until all the slack has been taken up (Paris, 1991) (Figure 6.37).
Resistive Testing
Trunk Flexion
The rectus abdominis is the primary trunk flexor. It is assisted by the obliquus internus and externus muscles (Figure 6.38).
•Position of patient (Figure 6.39): Supine with hands clasped behind the head.
•Resisted test: Stabilize the patient’s lower extremities by pressing down on the anterior aspect of the thighs and ask the patient to perform a curl-up, lifting the scapulae off the table. Observe the umbilicus for movement cranially or caudally. Movement toward the head indicates stronger contraction of the upper aspect of the muscle, and movement toward the feet indicates stronger contraction of the lower segments of
the rectus abdominis. Observe the umbilical region for a bulging of the abdominal contents through the linea alba. This represents an umbilical hernia. Trunk flexion is made easier if the patient attempts the test with the arms relaxed at the side.
Weakness of trunk flexion results in increased risk
of lower back pain and may cause difficulty in getting up from a seated position.
Figure 6.37 (left) Mobility testing of the sacroiliac joint: posteroanterior spring of the sacrum.
117

The Lumbosacral Spine Chapter 6
Rectus abdominus |
Internal |
External |
muscle |
oblique |
|
|
|
oblique |
Figure 6.38 The trunk flexors. |
Figure 6.40 The trunk rotators. |
Trunk Rotation
The rotators of the trunk are the obliquus internus and externus muscles (Figure 6.40). Accessory muscles include the multifidi, rotatores, rectus abdominis, latissimus dorsi, and semispinalis muscles.
•Position of patient (Figure 6.41): Supine with the hands behind the neck.
•Resisted test: Stabilize the patient’s lower extremities by pressing down on the anterior aspect of the thighs and ask the patient to raise the left shoulder blade up and twist the body so as to
Figure 6.39 Testing trunk flexion.
118
Chapter 6 The Lumbosacral Spine
Figure 6.41 Testing trunk rotation.
bring the left elbow toward the right hip. This tests for the left obliquus externus and the right obliquus internus muscles. Now ask the patient to repeat the procedure, bringing the right shoulder and scapula off the table and twisting toward the left to test the right obliquus externus and left obliquus internus muscles.
Spinalis
Weakness of the trunk rotators causes reduced expiratory effort and may result in a functional scoliosis. The risk of lower back pain is also increased.
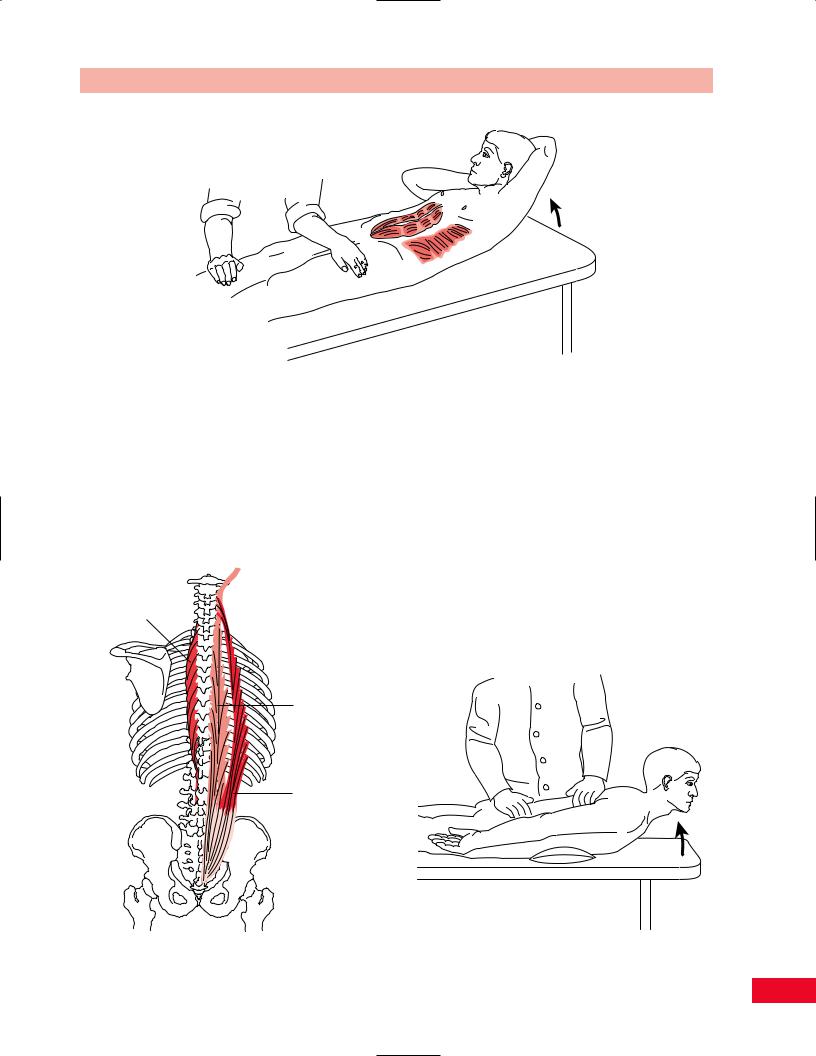
Trunk Extension
The extensors of the trunk are the erector spinae, which include the iliocostalis thoracis, longissimus thoracis, spinalis thoracis, and iliocostalis lumborum (Figure 6.42).
•Position of patient (Figure 6.43): Prone with arms at the side. Place a pillow beneath the abdomen for patient comfort and to reverse the lumbar lordosis.
Longissimus
Iliocostalis
Figure 6.42 The trunk extensors. |
Figure 6.43 Testing trunk extension. |
119
The Lumbosacral Spine Chapter 6
•Resisted test: Stabilize the patient’s pelvis with one of your forearms and ask the patient to raise the neck and sternum upward as the patient attempts to raise the trunk against your resistance applied to the middle of the back.
Weakness of the back extensor muscles results in a
loss of the lumbar lordosis and an increase in the thoracic kyphosis. Weakness on one side results in lateral curvature with concavity toward the strong side.
Neurological Testing
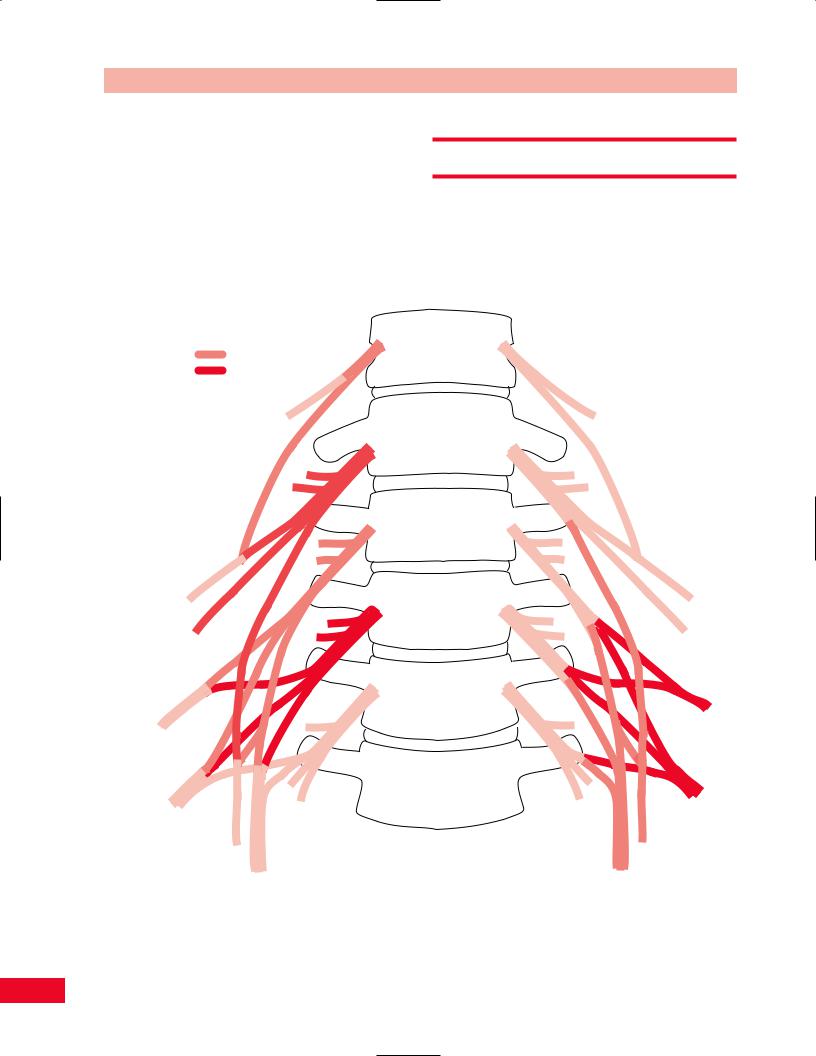
The Lumbar Plexus
The lumbar plexus is composed of the L1 through L4 nerve roots, with some contribution from T12 (Figure 6.44). The nerve roots branch into anterior
Divisions
Anterior
Posterior
Iliohypogastric
T12
L1
Ilioinguinal
L1
Lateral femoral cutaneous L2, 3
Femoral
L2, 3, 4
Genitofemoral
L1, 2
Obturator
L2, 3, 4
T12
T12
L1
L1
L2
L2
L3
L3
L4
L4
L5
Figure 6.44 The lumbar plexus. The lumbar plexus is formed by the ventral primary rami of L1, L2, L3, and L4 and possibly T12. Note that the peripheral nerves from the anterior divisions innervate the adductor muscles of the hip, and the peripheral nerves from the posterior divisions innervate the hip flexors and knee extensors.
120
Chapter 6 The Lumbosacral Spine
and posterior divisions near to the spine. The peripheral nerves that are formed from the anterior divisions innervate the adductor muscles of the hip. The nerves that form from the posterior divisions innervate the hip flexors and knee extensors.
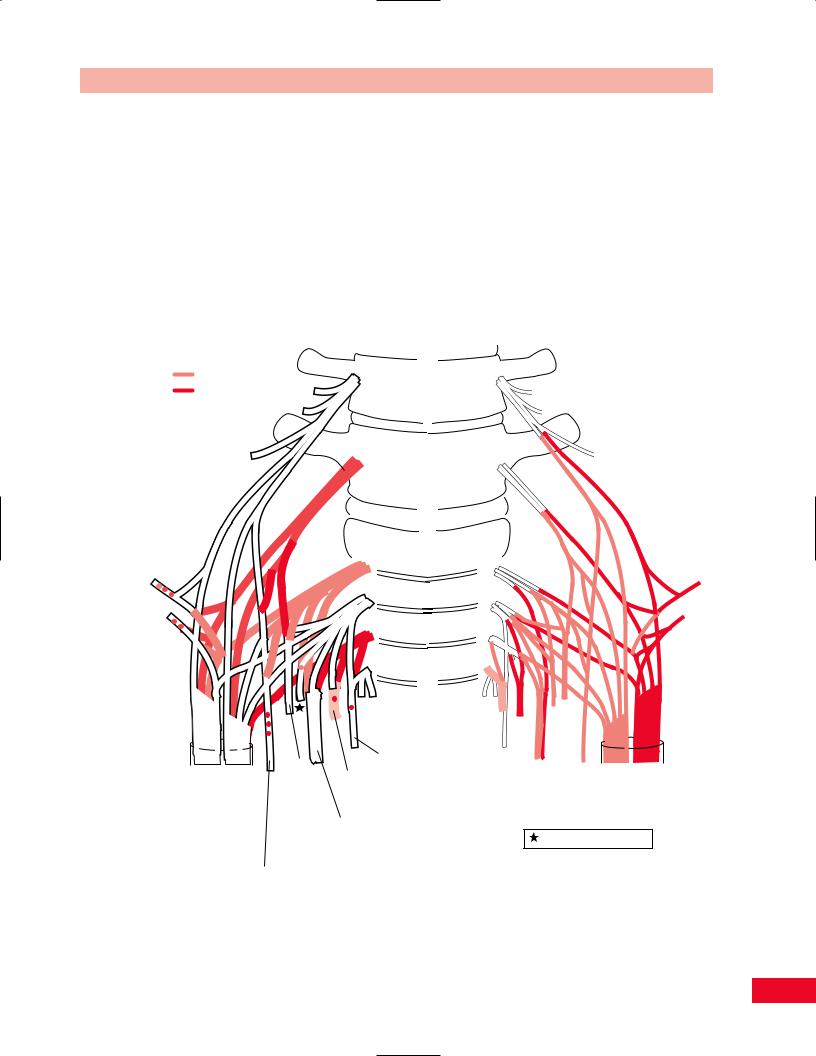
The Lumbosacral Plexus
The lumbosacral plexus is composed of the nerve roots from L4 through S3 (Figure 6.45).
Due to the rotation of the lower limb that occurs during embryogenesis, the anterior divisions and the
peripheral nerves that emanate from them innervate the posterior aspect of the lower extremity and the plantar surface of the foot. The posterior divisions of the lumbosacral nerve roots and the peripheral nerves derived from them innervate the lateral abductors and an extensor of the hip, the dorsiflexor muscles of the ankle, and the extensor muscles of the toes.
Testing by Neurological Level
Pathology of the lumbosacral spine is common and neurological testing is necessary to determine where in
Divisions
Anterior
Posterior
Superior gluteal L4, 5
S1
Inferior gluteal L5
S1, 2
L4
L5
S1
S2
S3
S4
L4
L5
S1
S2
S3
S4
|
|
|
|
|
to |
Pudendal |
|
Common |
Tibial |
|
S2, 3, 4 |
|
|||
|
Gemellus |
Perforating |
|
||||
peroneal |
L4, 5 |
|
|
||||
|
superior |
cutaneous |
|
||||
L4,5 |
S1, 2, 3 |
|
|||||
and |
S2, 3 |
|
|||||
S1, 2 |
|
|
|
|
|
||
|
|
|
|
Obturator |
|
|
|
Sciatic |
|
|
|
Posterior |
|
||
|
|
|
internus |
|
|||
L4, 5 |
|
|
|
Nerve to Piriformis S1, 2 |
|||
|
|
|
L5 |
femoral |
|||
S1, 2, 3 |
|
|
S1, 2 |
cutaneous |
|
||
|
|
|
to Gemellus |
S1, 2, 3 |
|
||
|
|
|
|
|
|||
|
|
|
inferior and |
|
|
||
|
|
|
Quadratus |
|
|
||
|
|
femoris L4, 5 |
|
|
|||
|
|
|
|
S1, (2) |
|
|
|
Figure 6.45 The lumbosacral plexus. This plexus is formed by the ventral primary rami of L4, L5, S1, S2, and S3.
121

The Lumbosacral Spine Chapter 6
Table 6.1 The lumbosacral plexus: muscle organization.
Root level |
Muscle test |
Muscles innervated at this level |
L1–L2 |
Hip flexion (adduction) |
Psoas, iliacus, sartorius, adductor longus pectineus gracilis, adductor brevis |
L3 |
Knee extension (hip adduction) |
Quadriceps, adductor magnus, and longus, brevis |
L4 |
Ankle dorsiflexion (knee extension) |
Tibialis anterior, quadriceps adductor magnus, obturator externus, tibialis |
|
|
posterior, tensor fascia lata |
L5 |
Toe extension (hip abduction) |
Extensor hallucis longus, extensor digitorum longus, gluteus medius and |
|
|
minimus, obturator internus, peroneus tertius, semimembranosus |
|
|
semitendinosus, popliteus |
S1 |
Ankle plantar flexion |
Gastrocnemius, soleus, gluteus maximus, biceps femoris, semitendinosus, |
|
Hip extension |
obturator internus, piriformis, peroneus longus and brevis, extensor |
|
Knee flexion |
digitorum brevis |
|
Ankle eversion |
|
S2 |
Knee flexion |
Biceps femoris, piriformis, flexor digitorum longus, flexor hallicus longus, |
|
|
gastrocnemius, soleus, intrinsic foot muscles |
|
|
|
the lumbosacral spine the pathology exists. The muscles of the lower extremity are usually innervated by specific nerve roots. Muscles that share a common nerve root innervation are in the same myotome (Table 6.1).
The skin of the lower extremity is innervated by peripheral nerves that emanate from specific nerve roots.
L1 |
L1 |
|
S 3 |
|
|
S 4 |
|||
S |
|
|
||
|
|
S 5 |
||
3 |
|
|
||
L2 |
L2 |
|
|
|
|
|
|
L2 |
L2 |
|
|
|
S2 |
S2 |
L3 |
L3 |
Key |
L |
L |
3 |
3 |
|||
|
|
Sensory |
|
|
|
|
Areas |
|
|
L4 |
L4 |
|
|
|
L5 |
L5 |
|
L |
L |
|
|
|
||
|
|
|
4 |
4 |
|
L5 |
L5 |
|
S1 |
S1 |
S1 |
S1 |
|
|
S1 |
|
Figure 6.46 The dermatomes and key sensory areas of the lower extremity.
Skin that shares innervation from a particular nerve root shares a common dermatome (Figure 6.46).
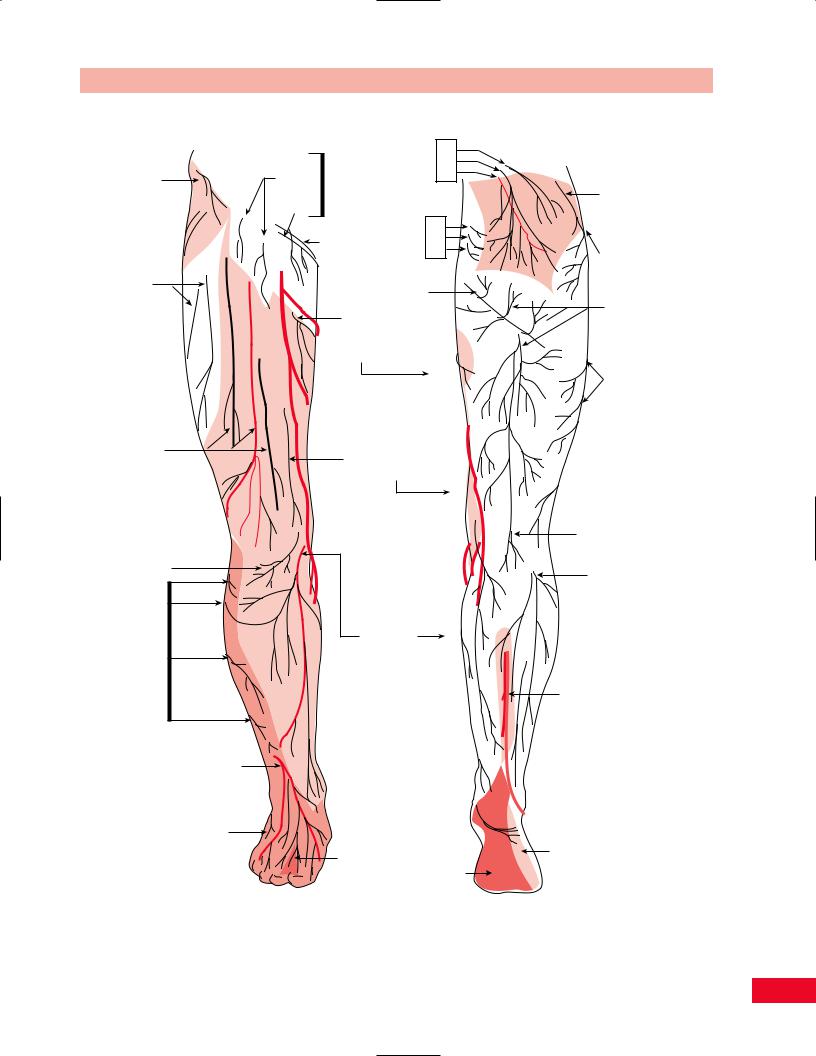
Knowledge of the myotomes, dermatomes, and peripheral nerve innervations (Figure 6.47) of the skin and muscles will assist you in the diagnosis of neurological pathology. Remember that there is significant variability from patient to patient with respect to patterns of innervation. With this in mind, the neurological examination is organized by root levels.
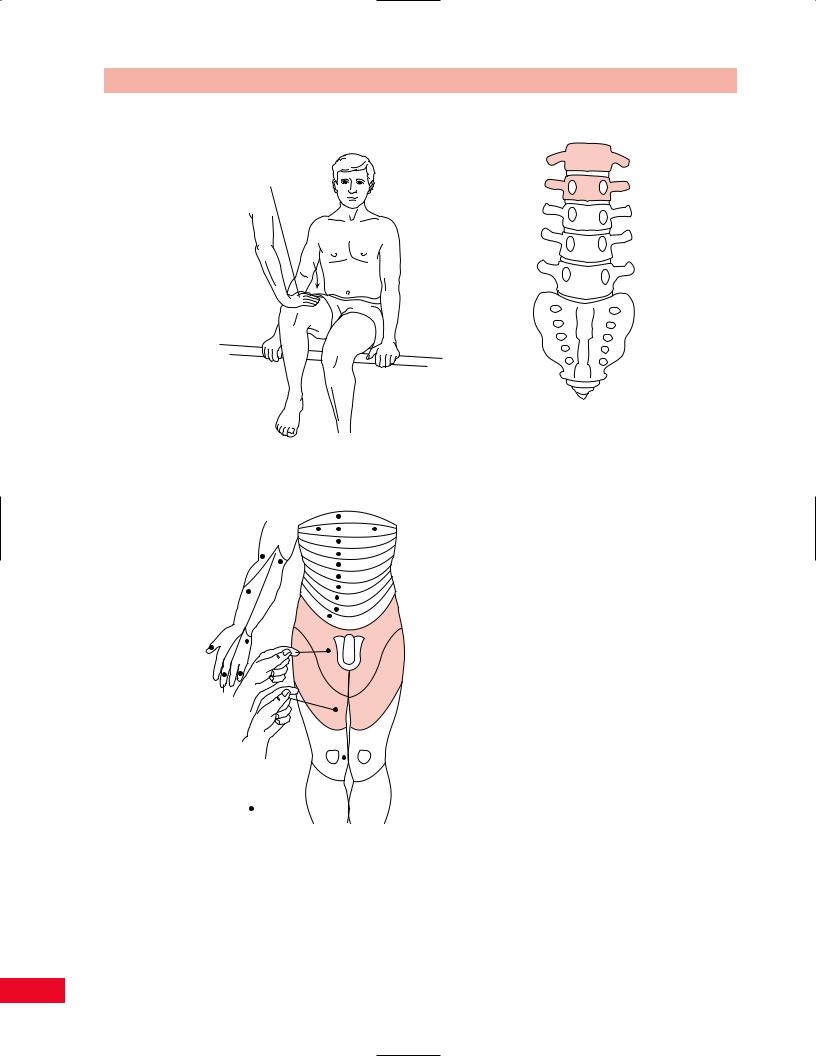
The L1 and L2 Levels
Muscle Testing
The L1 and L2 nerve roots (Figure 6.48) innervate the iliopsoas muscle, which is a hip flexor. Test hip flexion by having the patient sit at the edge of the table with the knees bent to 90 degrees. Ask the patient to raise the knee upward as you apply resistance to the anterior mid-aspect of the thigh (see pp. 313–315 for more information).
Sensation Testing
The L1 dermatome is located over the inguinal ligament. The key sensory area is located over the medial third of the ligament. The L2 dermatome is located over the proximal anteromedial aspect of the thigh. The key sensory area is located approximately midway from the groin to the knee in the medial aspect of the thigh.
Reflex Testing
There is no specific reflex for the L1 and L2 levels.
122
Chapter 6 The Lumbosacral Spine
Lateral cutaneous branch of subcostal nerve T12
Lateral femoral cutaneous nerve, anterior branches
Intermediate femoral cutaneous nerves
Infrapatellar branch of saphenous nerve
Cutaneous branches of common fibular or peroneal nerve
Superficial fibular or peroneal nerve becoming dorsal digital nerves
Dorsal lateral cutaneous nerve of foot
Cutaneous branches:
|
|
Dorsal |
L1 |
|
Femoral |
|
L2 |
||
|
rami |
L3 |
||
branch |
|
|||
Genitofemoral |
|
|
||
|
|
|
||
Genital nerve |
|
|
|
|
branch |
|
|
|
|
|
Ilioinguinal |
Dorsal |
S1 |
|
|
nerve |
S2 |
||
|
|
rami |
S3 |
|
Performing cutaneous nerve
Cutaneous branch of obturator nerve
Medial femoral cutaneous nerve
Saphenous nerve
Calcaneal nerve 
Lateral cutaneous branch of iliohypogastric nerve
Lateral femoral cutaneous nerve,  posterior branches
posterior branches
Branches of posterior femoral cutaneous nerve
Lateral femoral cutaneous nerve
Posterior femoral cutaneous nerve, end branch
Lateral sural cutaneous nerve
Medial sural cutaneous nerve
Dorsal lateral
 cutaneous nerve of foot (sural)
cutaneous nerve of foot (sural)
Deep fibular |
Lateral plantar nerve |
Medial |
|
or peroneal |
plantar |
nerve |
nerve |
A. Anterior view |
B. Posterior view |
Figure 6.47 The cutaneous innervation of a lower limb.
123
The Lumbosacral Spine Chapter 6
Motor
 L1
L1 
Hip flexion (iliopsoas)
L2
L3
L4
L5
Sensation
|
|
T3 |
|
|
|
T4 |
|
|
|
T5 |
|
|
|
T6 |
|
|
|
T7 |
|
T1 |
|
T8 |
|
|
T9 |
||
C6 |
|
T10 |
|
|
T11 |
||
|
|
||
|
L1 |
T12 |
|
|
|
L1 |
|
C8 |
|
S |
|
|
3 |
||
C7 |
L2 |
L2 |
|
|
|||
|
L3 |
L3 |
|
L1, L2 |
|
|
|
dermatomes |
|
|
|
Key ( ) |
L4 |
L4 |
|
L5 |
L5 |
||
sensory areas |
|||
|
|
Figure 6.48 The L1 and L2 root levels.
Reflex
"No Reflex"
124
