
- •Contents
- •Acknowledgments
- •Preface to the Third Edition
- •1 Introduction to Anatomic Systems and Terminology
- •2 Clinical Imaging Basics Introduction
- •3 Back
- •4 Clinical Imaging Basics of the Spine
- •5 Overview of the Thorax
- •6 Thoracic Wall
- •7 Mediastinum
- •8 Pulmonary Cavities
- •9 Clinical Imaging Basics of the Thorax
- •10 The Abdominal Wall and Inguinal Region
- •12 Abdominal Viscera
- •13 Clinical Imaging Basics of the Abdomen
- •14 Overview of the Pelvis and Perineum
- •15 Pelvic Viscera
- •16 The Perineum
- •18 Overview of the Upper Limb
- •19 Functional Anatomy of the Upper Limb
- •20 Clinical Imaging Basics of the Upper Limb
- •21 Overview of the Lower Limb
- •22 Functional Anatomy of the Lower Limb
- •23 Clinical Imaging Basics of the Lower Limb
- •24 Overview of the Head and Neck
- •25 The Neck
- •26 Meninges, Brain, and Cranial Nerves
- •29 Clinical Imaging Basics of the Head and Neck
- •Index

6 Thoracic Wall
A bony and muscular cage, which communicates superiorly with the neck and inferiorly with the abdomen, encloses and protects the thoracic contents. A superficial layer of extrinsic muscles overlies the thoracic cage, although these muscles act primarily on the upper limb. The breast, a derivative of the epidermis (outermost layer of skin), is a prominent superficial structure of the thoracic wall.
6.1 The Breast
General Features
The breast is made up of the mammary gland, a modified sweat gland, and its supporting fat and fibrous tissue (Figs. 6.1 and 6.2). Breasts remain rudimentary in males but are prominent struc-tures of the female pectoral region.
—Female breasts extend from the lateral border of the sternum to the midaxillary line and overlie the 2nd through 6th ribs.
—The breast is embedded in the subcutaneous layer of the skin overlying the deep fascia of the pectoralis major and serratus anterior muscles.
—The retromammary space is a plane of loose connective tissue that separates the breast from underlying fascia of the pectoralis major muscle and allows movement of the breasts on the thoracic wall.
—The highest prominence of the breast, the nipple, is located at the center of the areola. Circularly arranged smooth muscle fibers cause erection of the nipple in response to cold or tactile stimulation. In men and young women, the nipple is at the T4 vertebral level, but in older women this location varies considerably.
—The areola, the pigmented skin surrounding the nipple, contains sebaceous glands whose oily secretions lubricate the area during nursing.
—An axillary tail, or small finger of glandular tissue, may extend into the axilla (armpit) along the lower edge of the pectoralis muscle.
—The volume of fat, not the volume of glandular tissue, largely determines the differences in breast size among women.

Fig. 6.1 Surface anatomy of the breast
Right breast, anterior view. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
Mammary Gland
The mammary gland has two components:
—The parenchyma, or milk-producing part of the gland (see Fig. 6.2)
•The parenchyma consists of lobes divided into 15 to 20 lobules, which contain grapelike clusters of alveoli, hollow balls lined by secretory cells.
•Lactiferous ducts in the parenchyma drain each lobule and open at the nipple. Deep to the areola, each duct has a small, dilated portion called the lactiferous sinus where, in lactating females, a small amount of milk is stored.
—The stroma, or fibrous framework, of the gland that separates the lobules and supports the lobes
•Stroma is attached to the overlying dermis of the skin by suspensory (Cooper) ligaments, which are particularly strong on the superior surface of the breast.
Neurovasculature of the Breast
—Anterior intercostal branches and medial mammary branches (from perforating branches) of the internal thoracic artery, lateral thoracic and thoracoacromial branches of the axillary artery, and the 2nd, 3rd, and 4th posterior intercostal arteries supply the breast (see Sections 5.2 and 6.4).
—Venous blood drains primarily to the axillary vein but also to the internal thoracic vein.
—Most lymph (> 75%) from the breast drains (particularly from the lateral

quadrant) to axillary lymph nodes (Fig. 6.3); from there it travels to nodes around the clavicle and the ipsilateral lymphatic duct.
•Some lymph may drain to deep pectoral nodes, where it joins the bronchomediastinal drainage in the mediastinum.
•Medial portions of the breast may drain to parasternal nodes and to the contralateral breast; inferior segments may drain to abdominal nodes.
—The anterior and lateral cutaneous branches of the 4th, 5th, and 6th intercostal nerves innervate the breast.
Fig. 6.2 Structure of the breast
(From Gilroy AM, MacPherson BR, Wikenheiser JC. Atlas of Anatomy. Illustrations by Voll M and Wesker K. 4th ed. New York: Thieme Publishers; 2020.)

Fig. 6.3 Lymphatic drainage of the female breast
Anterior view. Axillary, parasternal, and cervical lymph nodes. Right thoracic and axillary region with the arm abducted. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 1st ed. New York: Thieme Publishers; 2007.)
BOX 6.1: CLINICAL CORRELATION
CARCINOMA OF THE BREAST
The most common type of breast cancer, invasive ductal carci-noma, arises from the lining of the lactiferous ducts. Typically, it metastasizes through lymphatic channels, most abundantly to axillary nodes from the supralateral quadrant but it may also travel to supraclavicular nodes, the contralateral breast, and the abdo-men. Obstruction of the lymphatic drainage causes edema, and fibrosis (shortening) of the suspensory ligaments can cause a pitted appearance of the skin. Through venous communication with the azygos system and vertebral venous plexus, breast cancer can metastasize to the vertebrae, cranium, and brain. Elevation of the breast with contraction of the pectoralis major muscle sug-gests invasion of the pectoralis fascia and retromammary space.
Origin of malignant breast tumors by quadrant

Right breast. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
Normal mammogram (From Gunderman R. Essential Radiology, 3rd ed. New York: Thieme; 2014.)
This mediolateral-oblique mammogram demonstrates a spiculated mass in the upper outer quadrant, an infiltrating ductal carcinoma, in this 63-year-old woman. (From Gunderman R. Essential Radiology, 3rd ed. New York: Thieme Publishers; 2014.)
6.2 The Thoracic Skeleton
The thoracic skeleton protects the thoracic viscera and provides attachment for
the upper limb. The thoracic cage includes the sternum, 12 pairs of ribs, and the 12 thoracic vertebrae (Fig. 6.4).
The Sternum
The sternum is a flat, elongated bone that has three parts:
1.The manubrium, which articulates laterally with the costal cartilages (cartilage that attaches the ribs to the sternum) of the 1st and 2nd ribs. A deep jugular notch separates the right and left sternoclavicular joints, where the manubrium articulates with the clavicles.
2.The body, which is fused superiorly with the manubrium at the manubriosternal joint. Laterally, the body articulates with costal cartilages of the 2nd to 7th ribs.
3.The xiphoid process, the lowest part of the sternum, which joins superiorly
with the body of the sternum at the xiphis-ternal joint.
•The sternal angle is an important surface landmark on the anterior thoracic wall that provides orientation to the internal anatomy of the thorax. It is a palpable ridge that marks the fusion of the manubrium and body of the sternum. A horizontal plane through the sternal angle intersects
◦the articulation between the sternum and the costal cartilages of the 2nd ribs,
◦the division of the mediastinum into superior and inferior regions,
◦the origin and termination of the aortic arch,
◦the bifurcation of the trachea, and
◦the T4–T5 intervertebral disk.

Fig. 6.4 Thoracic skeleton
Anterior view. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
The Ribs
—The ribs are numbered 1 to 12 from superior to inferior, and each rib articulates with a thoracic vertebra of the same number.
—The ribs hang obliquely downward from their articulation with the vertebral column. Their anterior ends may be two to five vertebral levels lower than their posterior attachment.
—Ribs 1 to 10 articulate anteriorly with a cartilaginous segment called the costal cartilage.
—The ribs are classified according to the articulation of their costal cartilage with the sternum (Fig. 6.5):
•True ribs (1 to 7) articulate directly with the sternum via individual costal cartilages.
•False ribs (8 to 10) articulate indirectly with the sternum through costal cartilages that are connected to the cartilage superior to it.
•Floating ribs (11 and 12) have no connection to the sternum.
—Most ribs articulate at three joints (Fig. 6.6):
1. Costochondral joints between the bony segments of ribs 1 to 10 and their respective costal cartilages

2.Sternocostal joints between the sternum and costal cartilages of ribs 1 to 7 on each side
3.Costovertebral joints between the ribs and vertebrae. These joints may contain multiple articulations.
◦The costal tubercle of each rib articulates with the costal facet on its accompanying thoracic vertebra (see Fig. 3.6).
◦The heads of ribs 2 to 10 articulate with the vertebra of the same number and with the vertebra superior to them. Ribs 1, 11, and 12 articulate only with their own vertebra.
Thoracic Apertures
—The thoracic cage has superior and inferior openings (see Fig. 6.4):
•The superior thoracic aperture (thoracic inlet), which is bounded by the T1 vertebra, the 1st ribs, and the manubrium of the sternum. The thorax communicates with the neck through this opening.
•The inferior thoracic aperture (thoracic outlet), which is bounded by the T12 vertebra, the 11th and 12th ribs, the costal margin (lower border of the thoracic cage), and the xiphoid process. A muscular diaphragm closes this aperture, separating the thoracic cavity from the abdomi-nal cavity.
Fig. 6.5 Types of ribs
Left lateral view. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)

Fig. 6.6 Structure of a thoracic segment
Superior view of 6th rib pair. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
6.3 Muscles of the Thorax
Muscles of the Thoracic Wall (Fig. 6.7; Table 6.1)
—Extrinsic muscles of the upper limb, including the pectoralis major, pectoralis minor, and serratus anterior, cover the thorax. Although they mainly move or stabilize the upper limb, these muscles also assist in movements of the ribs during deep inspiration. (See Chapter 18, Overview of the Upper Limb.)
—The anterior scalene, middle scalene, and posterior scalene muscles originate on the transverse processes of the cervical vertebrae and insert onto the 1st and 2nd ribs. They assist the intrinsic thoracic muscles during inspiration and are consid-ered extrinsic muscles of respiration.
—Intrinsic muscles of the thoracic wall are the chief muscles that move the ribs during respiration.
•The intercostal muscles occupy the intercostal spaces between the ribs. They extend from the inferior border of one rib to the superior border of
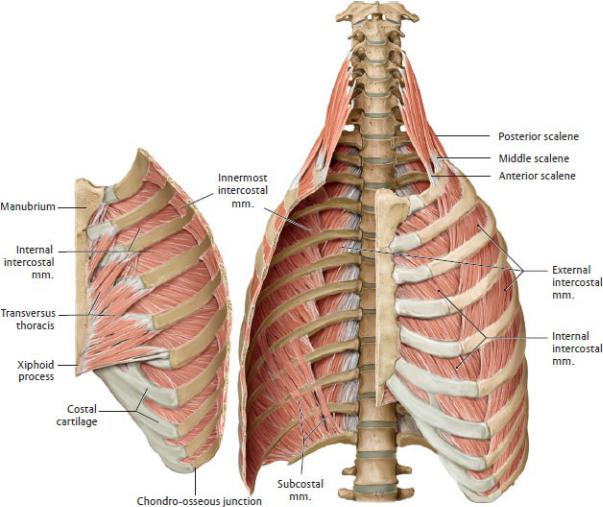
the next inferior rib. The intercostal muscles move the ribs primarily during forced respiration. During quiet respiration, they stabilize the thoracic wall. They include
Fig. 6.7 Transversus thoracis
Anterior view with thoracic cage opened to expose posterior surface of anterior wall. The external and internal intercostal membranes have been removed. (From Gilroy AM, MacPherson BR, Wikenheiser JC. Atlas of Anatomy. Illustrations by Voll M and Wesker K. 4th ed. New York: Thieme Publishers; 2020.)

◦the external intercostal muscles, with fibers directed inferoanteriorly, which make up the most superficial layer
◦the internal intercostal and innermost intercostal muscles, which occupy the middle and deepest layers of the thoracic wall, respectively, with their fibers directed inferoposteriorly
•The subcostal muscles are most prominent along the lower thoracic wall, where they cross the inner surface of one or two intercostal spaces.
•The transversus thoracic muscles consist of four of five thin slips that extend superiorly and laterally from the posterior surface of the sternum to the ribs.
The Thoracic Diaphragm
The thoracic diaphragm (or simply, the diaphragm), a musculotendinous sheet that separates the thorax from the abdomen, is the principal muscle of respiration. The diaphragm forms the floor of the thorax, the roof of the abdomen, and a portion of the posterior abdominal wall (Fig. 6.8).
—The skeletal muscle fibers of the diaphragm originate along the costal margin, the vertebral bodies of L1–L3, the medial and lateral arcuate ligaments, and the xiphoid process. They insert on the diaphragm’s central tendon.
—Right and left crura, extensions of the posterior diaphragm, attach to

the bodies of the lumbar vertebrae, with the right crus extending slightly lower than the left crus.
Fig. 6.8 Diaphragm
The diaphragm, which separates the thorax from the abdomen, has two asymmetric domes and three apertures (for the aorta, vena cava, and esophagus). (From Gilroy AM, MacPherson BR, Wikenheiser JC. Atlas of Anatomy.

Illustrations by Voll M and Wesker K. 4th ed. New York: Thieme Publishers; 2020.)
Fig. 6.9 Projection of the diaphragm onto the trunk
Anterior view. Position of the diaphragm in inspiration and expiration. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 2. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
—The domes on the right and left sides of the diaphragm are asymmetric; the right hemidiaphragm is generally higher than the left.
—During full expiration the diaphragm is 4 to 6 cm higher than during full inspiration. During expiration it ascends to the level of the 4th or 5th rib on the right and slightly lower on the left, although this varies with respiration, posture, and body type (Fig. 6.9).
—The diaphragm has three openings to allow the passage of structures between the thorax and abdomen (Fig. 6.10):
1.The caval opening, which is a passage for the inferior vena cava through the central tendon at the T8 vertebral level.
2.The esophageal hiatus, which is an opening at the T10 vertebral level for the esophagus, the anterior and poste-rior vagal trunks, and left gastric artery and vein.It is usually formed by the right crus of the diaphragm (occasionally by the right and left crura) that, when contracted, forms a sphincter around the esophagus.
3.The aortic hiatus, which is a passageway for the aorta between the right

and left crura as it passes behind the diaphragm at T12. The thoracic duct, and often the azygos and hemiazygos veins, also passes through this aperture.
—The inferior phrenic arteries, branches of the abdominal aorta (or celiac trunk), are the primary blood supply to the diaphragm. The superior phrenic, pericardiacophrenic, and musculophrenic arteries make additional contributions (Fig. 6.11).
—Venous blood drains to the azygos system through posterior intercostal and superior phrenic veins.
—The phrenic nerve (C3–C5) provides all of the motor and most of the sensory innervation to the diaphragm. The subcostal and lower intercostal nerves transmit sensory information from the periphery of the diaphragm
(Fig. 6.12).
Fig. 6.10 Diaphragmatic apertures


Fig. 6.11 Neurovasculature of the diaphragm
Fig. 6.12 Innervation of the diaphragm
Anterior view. The phrenic nerve lies on the lateral surface of the fibrous pericardium together with the pericardiacophrenic arteries and veins. Note: The phrenic nerve also innervates the pericardium. (From Gilroy AM, MacPherson BR, Wikenheiser JC. Atlas of Anatomy. Illustrations by Voll M and Wesker K. 4th ed. New York: Thieme Publishers; 2020.)
6.4 Neurovasculature of the Thoracic Wall
—Intercostal neurovascular bundles course along the inferior surface of the ribs within the costal groove (Figs. 6.13, 6.14, 6.15, 6.16).
•Anterior intercostal arteries (branches of the internal thoracic arteries) and posterior intercostal arteries (branches of the thoracic aorta and subclavian arteries) supply the muscles and skin of the thoracic wall
(Fig. 6.14).
•Intercostal veins drain primarily to the azygos system but also into the brachiocephalic and internal thoracic veins, which join the superior vena

cava (Fig. 6.15).
—The thoracoepigastric vein is a superficial vein that drains the subcutaneous tissue of the anterolateral thoracic and abdominal walls. It drains superiorly to the axillary vein of the upper limb and inferiorly to the superficial epigastric vein (Fig. 6.16).
—The thoracic wall is drained by three major groups of lymph nodes:
•The parasternal nodes, which are scattered along the internal thoracic artery. They receive lymph from the breast, anterior thoracic wall, liver, and upper deep surface of the anterior abdominal wall.
•The intercostal nodes, which are located in the inter-costal spaces near the heads and necks of the ribs. They drain the posterolateral part of the chest and mammary glands.
•The diaphragmatic nodes, which are located on the superior surface of the diaphragm. They drain the central tendon of the diaphragm, the fibrous pericardium, and the superior surface of the liver.
—Intercostal nerves T1–T11 innervate the muscles of the thoracic wall. In the midaxillary line these nerves give off a lateral cutaneous branch that supplies the superficial muscles and skin of the thorax (Figs. 6.17 and 6.18).
Fig. 6.13 Neurovascular topography of the thoracic wall

(From Gilroy AM, MacPherson BR, Wikenheiser JC. Atlas of Anatomy. Illustrations by Voll M and Wesker K. 4th ed. New York: Thieme Publishers; 2020.)
Fig. 6.14 Course and branches of the intercostal arteries
(From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
Fig. 6.15 Intercostal veins
Anteriosuperior view. Vertebral column and rib segment. (From Schuenke M,

Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
Fig. 6.16 Superficial veins
Anterior view. The thoracoepigastric veins are a potential superficial collateral venous drainage route in the event of superior or inferior vena cava obstruction. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
—The 7th through 11th intercostal nerves continue anteriorly from the intercostal space to innervate the anterior abdomi-nal wall.
—Landmark dermatomes on the thoracic wall include T4 at the nipple and T6 over the xiphoid process.
—Intercostal nerves and vessels are protected within the costal groove on the deep inferior edge of the ribs (see Box 6.2). Within this bundle of neurovascular structures, the nerve runs inferior to its accompanying vessels.

Fig. 6.17 Branches of an intercostal nerve
(From Gilroy AM, MacPherson BR, Wikenheiser JC. Atlas of Anatomy. Illustrations by Voll M and Wesker K. 4th ed. New York: Thieme Publishers; 2020.)
Fig. 6.18 Cutaneous innervation of the thoracic wall
Anterior view. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of

Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
BOX 6.2: CLINICAL CORRELATION
INSERTION OF A CHEST TUBE
Abnormal fluid collection in the pleural space (e.g., pleural effu-sion due to bronchial carcinoma) may necessitate the insertion of a chest tube. Generally, the optimal puncture site in a sitting patient is at the level of the fourth and fifth intercostal space in the mid to anterior axillary line, immediately behind the lateral edge of the pectoralis major. The drain should always be intro-duced at the upper margin of a rib to avoid injuring the intercostal vein, artery, and nerve.
Coronal section, anterior view
(From Gilroy AM, MacPherson BR, Wikenheiser JC. Atlas of Anatomy. Illustrations by Voll M and Wesker K. 4th Edition. New York: Thieme Publishers;
