
- •Contents
- •Acknowledgments
- •Preface to the Third Edition
- •1 Introduction to Anatomic Systems and Terminology
- •2 Clinical Imaging Basics Introduction
- •3 Back
- •4 Clinical Imaging Basics of the Spine
- •5 Overview of the Thorax
- •6 Thoracic Wall
- •7 Mediastinum
- •8 Pulmonary Cavities
- •9 Clinical Imaging Basics of the Thorax
- •10 The Abdominal Wall and Inguinal Region
- •12 Abdominal Viscera
- •13 Clinical Imaging Basics of the Abdomen
- •14 Overview of the Pelvis and Perineum
- •15 Pelvic Viscera
- •16 The Perineum
- •18 Overview of the Upper Limb
- •19 Functional Anatomy of the Upper Limb
- •20 Clinical Imaging Basics of the Upper Limb
- •21 Overview of the Lower Limb
- •22 Functional Anatomy of the Lower Limb
- •23 Clinical Imaging Basics of the Lower Limb
- •24 Overview of the Head and Neck
- •25 The Neck
- •26 Meninges, Brain, and Cranial Nerves
- •29 Clinical Imaging Basics of the Head and Neck
- •Index
1 Introduction to Anatomic Systems and Terminology
Anatomy of the human body can be studied by inspection of all the systems that occupy a specific region or by considering the global aspects of a particular system throughout the entire body. The first approach tends to focus on anatomic relationships while the second is better suited to studying physiologic influences. Most systems, however, are conveniently confined to one or two regions, and in this text are discussed in the units devoted to those regions. Some systems, however, (those included in this chapter) are more pervasive throughout the body, and a fundamental under-standing of their basic organization is important before undertak-ing the study of the systems they support.
1.1 Structural Design of the Human Body
The most preliminary inspection of the human body reveals that it is structurally divided into a head and neck region, a trunk, and paired upper and lower extremities (limbs). Each is further divided into smaller regions (Fig. 1.1; Table 1.1). These house the structures that make up the functional organ systems that perform the basic bodily functions (Table 1.2). Although the pri-mary organ of a system is often confined to a single anatomic region (e.g., the brains resides in the head), systems extend beyond regional borders, both anatomically and physiologically, to inte-grate their influences on normal function and growth.
Table 1.1 Regional Subdivisions of the Body
Head
Neck
Trunk
•Thorax (chest)
•Abdomen
•Pelvis
Upper limb
•Shoulder girdle
•Free upper limb
Lower limb
•Pelvic girdle
•Free lower limb
Table 1.2 Functional Subdivisions by Organ Systems
Locomotor system (musculoskeletal system)
•Skeleton and skeletal connections (passive part)
•Striated skeletal musculature (active part)
Viscera
•Cardiovascular system
•Hemolymphatic system
•Endocrine system
•Respiratory system
•Digestive system
•Urinary system
•Male and female reproductive system
Nervous system
•Central and peripheral nervous system
•Sensory organs
The skin and its appendages
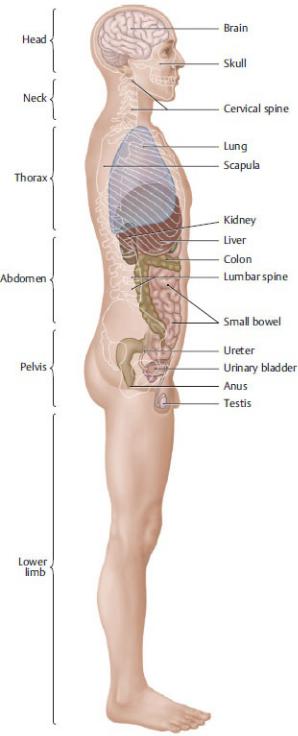
Fig. 1.1 Structural design of the human body: location of the internal organs.
(From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
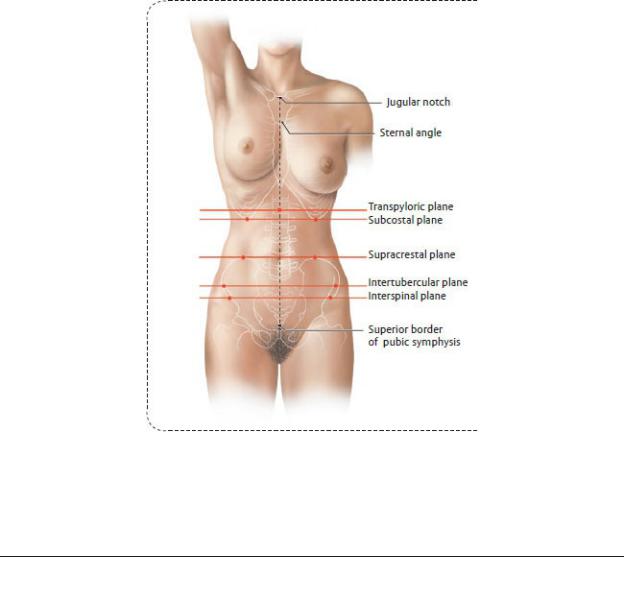
1.2 Terms of Location and Direction, Cardinal
Planes, and Axes
—All locational and directional terms used in anatomy, and in medical practice, refer to the human body in the anatomic position, in which the body is upright, arms at the side, with the eyes, palms of the hands, and feet directed forward (Fig. 1.2, Table 1.3).
—Three perpendicular cardinal planes and three axes based on the three spatial coordinates can be drawn through the body (Fig. 1.3).
•The sagittal plane passes through the body from front to back, dividing it into right and left sides.
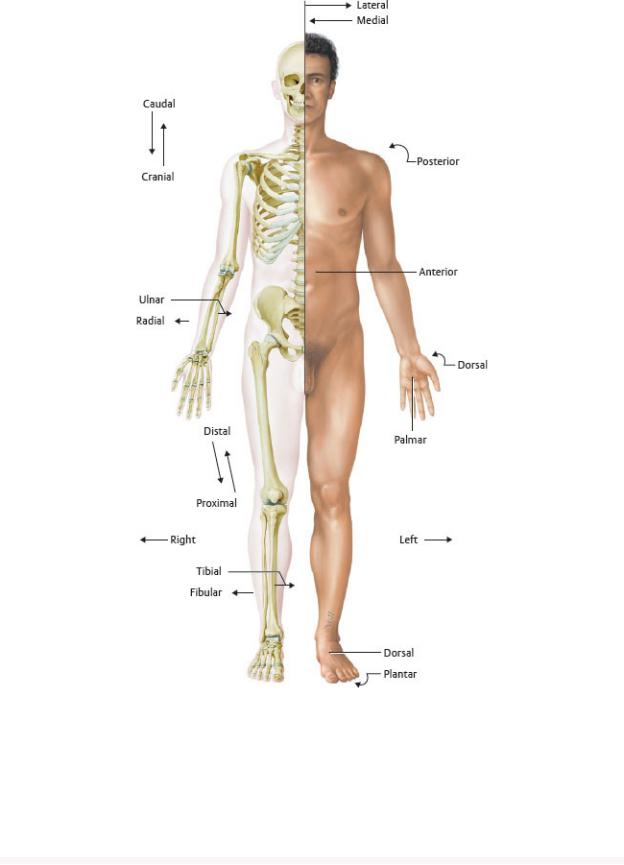
Fig. 1.2 Anatomic position.
Anterior view. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
Table 1.3 General Terms of Location and Direction
Term Explanation
Upper Body (Head, Neck, and Trunk)
Cranial |
Pertaining to, or located toward, the head |
Caudal |
Pertaining to, or located toward, the tail |
|
|
Anterior |
Pertaining to, or located toward, the front; synonym: |
|
ventral (used for all animals) |
|
|
Posterior |
Pertaining to, or located toward, the back; synonym: |
|
dorsal (used for all animals) |
|
|
Superior |
Upper or above |
|
|
Inferior |
Lower or below |
|
|
Axial |
Pertaining to the axis of a structure |
|
|
Transverse |
Situated at right angles to the long axis of a structure |
|
|
Longitudinal |
Parallel to the long axis of a structure |
|
|
Horizontal |
Parallel to the plane of the horizon |
|
|
Vertical |
Perpendicular to the plane of the horizon |
|
|
Medial |
Toward the median plane |
|
|
Lateral |
Away from the median plane (toward the side) |
|
|
Median |
Situated in the median plane or midline |
|
|
Peripheral |
Situated away from the center |
|
|
Superficial |
Situated near the surface |
|
|
Deep |
Situated deep beneath the surface |
|
|
External |
Outer or lateral |
|
|
Internal |
Inner or medial |
|
|
Apical |
Pertaining to the top or apex |
|
|
Basal |
Pertaining to the bottom or base |
|
|
Sagittal |
Situated parallel to the sagittal suture |

Coronal |
Situated parallel to the coronal suture (pertaining to |
|
the crown of the head) |
|
|
Limbs |
|
|
|
Proximal |
Close to, or toward, the trunk, or toward the point of |
|
origin |
|
|
Distal |
Away from the trunk (toward the end of the limb), or |
|
away from the point of origin |
|
|
Radial |
Pertaining to the radius or the lateral side of the |
|
forearm |
|
|
Ulnar |
Pertaining to the ulna or the medial side of the |
|
forearm |
|
|
Tibial |
Pertaining to the tibia or the medial side of the leg |
|
|
Fibular |
Pertaining to the fibula or the lateral side of the leg |
|
|
Palmar (volar) |
Pertaining to the palm of the hand |
|
|
Plantar |
Pertaining to the sole of the foot |
|
|
Dorsal |
Pertaining to the back of the hand or top of the foot |
|
|
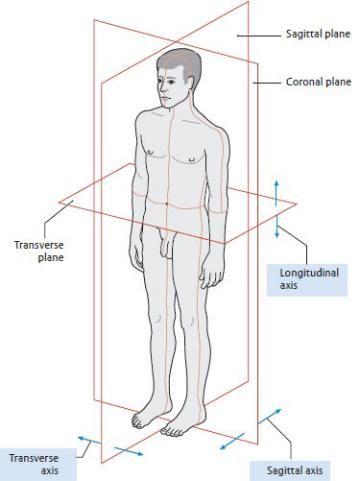
Fig. 1.3 Cardinal planes and axes.
Neutral position, left anterolateral view. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
•The coronal plane passes through the body from side to side, dividing it into front (anterior) and back (posterior) parts.
•The transverse (axial, horizontal, cross-sectional) plane divides the body into upper and lower parts. A particular transverse section is often given the designation of the corresponding vertebral level, such as T4, which passes through the fourth thoracic vertebra.
•The longitudinal axis passes along the height of the body in a craniocaudal direction.
•The sagittal axis passes from the front to the back (or the back to the front) of the body in an anteroposterior direction.
•The transverse (horizontal) axis passes through the body from side to
side.
1.3 Landmarks and Reference Lines
—In surface anatomy, palpable structures or visible markings on the surface of the body are used to identify the location of underlying structures. Reference lines are vertical or transverse planes that connect palpable structures or markings (Tables 1.4, 1.5, and 1.6; see also Fig. 1.5).
Table 1.4 Anterior and Lateral Reference Lines on the Trunk
(From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
Anterior midline |
Passes through the center of the sternum |
Sternal line |
Passes along the lateral border of the sternum |
|
|
Midclavicular line |
Passes through the midpoint of the clavicle |
Parasternal line |
Passes through a point midway between the |
|
sternal and midclavicular lines |
|
|
Anterior axillary line |
Marks the anterior axillary fold formed by the |
|
pectoralis major muscle |
|
|
Posterior axillary |
Marks the posterior axillary fold formed by the |
line |
teres major muscle |
|
|
Midaxillary line |
Marks the midpoint between the anterior and |
|
posterior axillary lines |
|
|
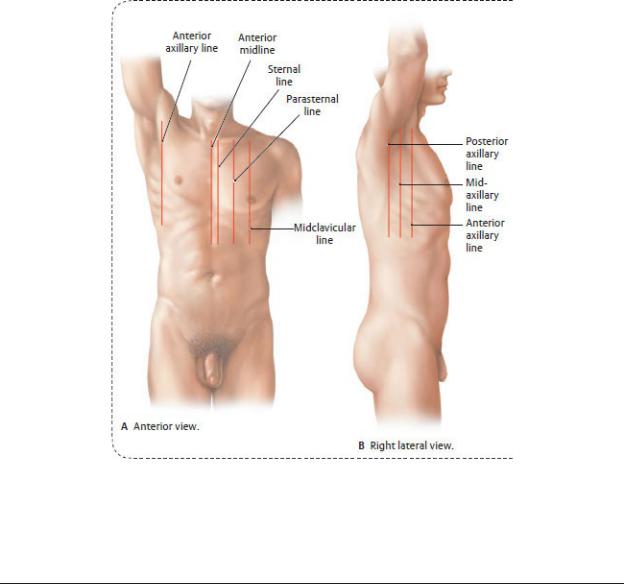
Table 1.5 Landmarks and Transverse Planes on the Anterior Trunk
(From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
Jugular notch Marks the superior border of the manubrium
Sternal angle |
Marks the junction of manubrium and body of the |
|
sternum |
|
|
Transpyloric |
Passes through the midpoint between the jugular notch |
plane |
and pubic symphysis |
|
|
Subcostal |
Marks the lowest level of the thoracic cage, the tenth |
plane |
costal cartilage |
|
|
Supracrestal |
Connects the top of the iliac crests |
plane |
|
|
|
Intertubercular |
Passes through the iliac tubercles |
plane |
|
|
|
Interspinal |
Connects the anterior superior iliac spines |
plane |
|
|
|
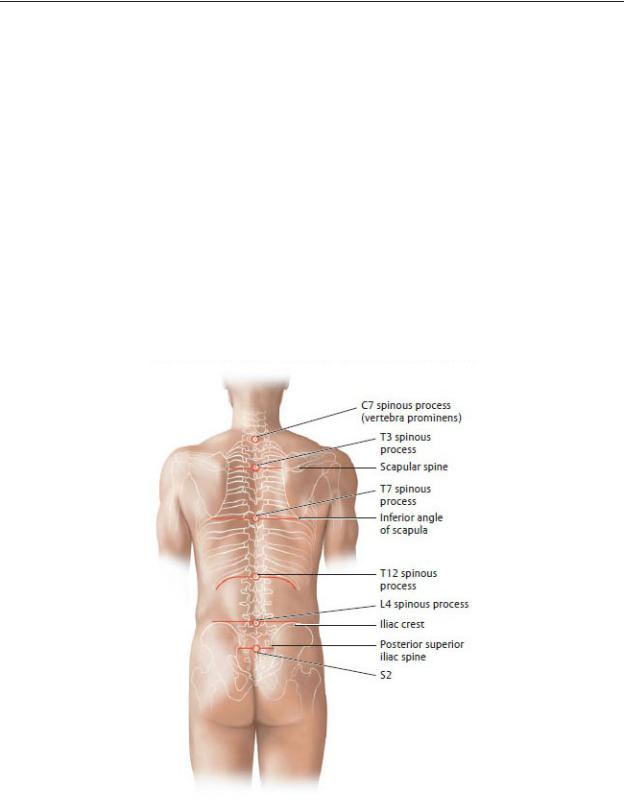
Table 1.6 Vertebral Spinous Processes and Posterior Landmarks
(From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
C7 The vertebra prominens
T3 Level of the medial edge of spines of the scapulae
T7 Level of the inferior angles of the scapulae
T12 Level of the lower limit of the thoracic cavity
L4 Level of the iliac crests
S2 Level of the posterior superior iliac spine
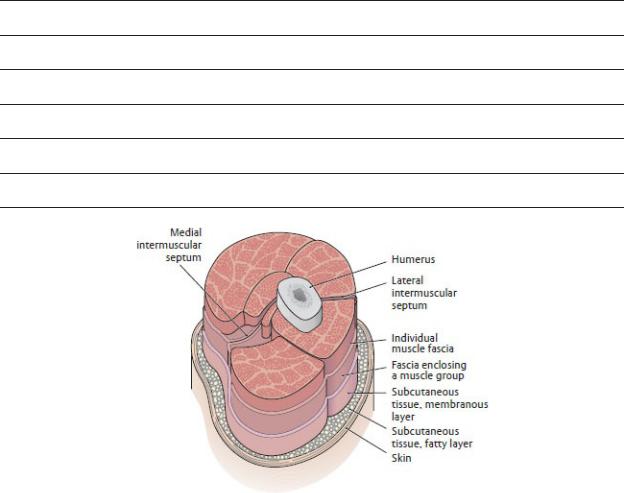
Fig. 1.4 Fascia.
Cross section through the right arm, proximal view. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
1.4 Connective and Supporting Tissues
—Connective tissue comprises a variety of forms that are found throughout the body. Its common characteristic is a predomi-nance of extracellular material made up largely of fibrous proteins and an amorphous ground substance and widely spaced cells that may include adipocytes, fibroblasts, and
mesenchymal stem cells as well as macrophages and lymphocytes. Bone and cartilage are specialized types of connective tissue.
—The classification of connective tissue types is based on the degree to which the fibrous components are organized.
•Irregular types include
◦Loose, or areolar, connective tissue, which is widely distributed around vessels and nerves and within organs, where it binds lobes and groups of muscle fascicles. It provides support while allowing movement of structures.
◦Dense connective tissue, which supports structures under mechanical stress. It ensheathes muscles and nerves and forms the capsules of organs such as the testis.
◦Adipose tissue, or fat, which is found in specialized areas such as the subcutaneous tissue of the skin, the female breast, and padding on the soles of the feet and in the renal bed surrounding the kidneys.
•Regular connective tissue, which is largely fibrous but may also contain elastin fibers, makes up the tendons, liga-ments, and aponeuroses as well as fascial layers that enclose muscles and underlie the skin.
—Fascia is a general term that has been redefined in recent years to describe any easily discernable connective tissue sheet or sheath. The most common usages pertain to the connective tissue layers between the skin and muscle, formerly known as the superficial and deep fasciae. New terminology refers to these layers as the subcutaneous connective tissue with two layers (Fig. 1.4):
•A fatty layer of varying thickness that lies deep to the skin, composed of loose connective tissue and fat, traversed by superficial nerves and vessels.
•A membranous layer of dense connective tissue layer that lies under (deep to) the fatty layer and is devoid of fat. It forms an investing layer, which envelops neurovascular structures and muscles of the limbs, trunk wall, head, and neck. Invaginations of this layer form intermuscular septa that compartmentalize limb musculature into functional groups.
1.5 The Integumentary System
The skin (integument), the largest organ of the body, protects underlying tissue from biologic, mechanical, and chemical injury; regulates body temperature; and participates in metabolic pro-cesses, such as the synthesis of vitamin D.
—The skin is composed of
•an outer waterproof avascular layer, the epidermis, which has a superficial layer of keratinized cells that shed continuously and a deep basal layer of regenerating cells, and
•an inner richly vascularized and innervated layer, the dermis, which supports the epidermis and contains hair follicles.
1.6 The Skeletal System
The bones and cartilages of the body, which make up the skeletal system, provide leverage for muscles and protect the internal organs. Bone is also the site for calcium storage and blood cell production.
—There are two anatomic divisions of the skeleton (Fig. 1.5):
•The axial skeleton, which consists of the skull, vertebrae, sacrum, coccyx, ribs, and sternum
•The appendicular skeleton, which includes the clavicle and scapula of the pectoral girdle, the coxal bones of the pelvic girdle, and the bones of the upper and lower limbs
—Periosteum is a thin layer of fibrous connective tissue that coats the outer surface of each bone (Fig. 1.6). Perichon-drium forms a similar layer around cartilaginous structures. These tissues nourish and assist in the healing of the underlying bone.
—All bones have a superficial layer of dense compact (cortical) bone that surrounds a less dense cancellous (spongy) bone. In some areas of the bone, a medullary cavity contains yellow (fatty) or red (blood cell or plateletforming) bone marrow.
—Bones develop from mesenchyme (embryonic connective tissue) through two processes of ossification (bone formation).
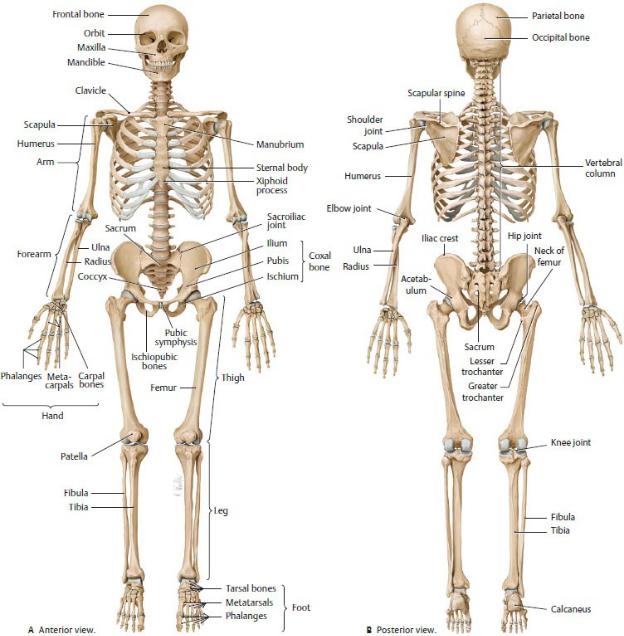
Fig. 1.5 Human skeleton.
Left forearm is pronated, and both feet are in plantarflexion. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)

Fig. 1.6 Structure of a typical long bone.
Illustrated for the femur. Coronal cuts through the proximal and distal parts of an adult femur. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York:
Thieme Publishers; 2020.)
•The clavicle and some bones of the skull develop by membranous ossification, in which the bones form through direct ossification of mesenchymal templates that are set down during the embryonic period.
•Most bones, including the long bones of the limbs, develop by endochondral ossification, in which a cartilaginous template, formed from mesenchyme, is laid down during the fetal period. Over the first and second decades of life, bone replaces most of the cartilage.
◦Within each bone undergoing endochondral ossification, bone formation occurs first at a primary ossifi cation center, which is in the diaphysis (shaft) of the long bones. Secondary ossification centers appear later at the epiphyses (growing ends) of the bones.
—Long bones of the skeleton increase in length through growth of the epiphyses and diaphysis on either side of the epiphy-seal plate, an intervening cartilaginous area. During child-hood and adolescence the epiphyseal plates gradually shorten as they are replaced by bone. In the adult these areas are completely ossified, and only thin epiphyseal lines remain.
—Apophyses, bony outgrowths that lack their own growth center, serve as attachment sites for ligaments or tendons. Specific apophyses are referred to as condyles, tubercles, spines, crests, trochanters, or processes.
—Ligaments are connective tissue bands that connect bones to each other or to cartilage. (Within the body cavities, the term ligament refers to folds or condensations of a serous or fibrous membrane that support visceral structures.)
—Joints are classified according to the type of tissue that connects the bones.
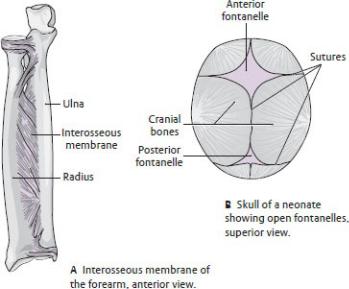
•Syndesmoses (fibrous joints), such as those found in the sutures of the skull and interosseous membrane of the forearm, are united by fibrous tissue and allow minimal movement (Fig. 1.7).
•Synchondroses (cartilaginous joints) are united either by fibrocartilaginous segments, such as the costal cartilages of the ribs, intervertebral disks, and pubic symphysis (Fig. 1.8A,B), or by articular cartilage, often found in temporary joints, such as those that join the ilium, ischium, and pubis of the hip bone (Fig. 1.8C). Subsequent fusion of these temporary joints creates synostoses (sites of bony fusion) (Fig. 1.9).
•Synovial joints, the most common type of joint, allow free movement (Fig. 1.10) and typically have
◦a joint cavity that is enclosed by a fibrous joint capsule and lined by a synovial membrane, which secretes a thin film of lubricating synovial fluid;
◦articulating ends of the bones that are covered by articular (hyaline) cartilage; and
◦extrinsic ligaments on the outer surface, which reinforce the joints.
◦Some synovial joints also contain intrinsic ligaments and intraarticular fibrocartilaginous structures.
—Bursae are closed sacs that contain a thin film of fluid and are lined with a synovial membrane. Commonly found around joints of the limbs, bursae cushion prominent bony processes from external pressure and prevent friction where tendons cross bony surfaces.
Fig. 1.7 Syndesmoses
(From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
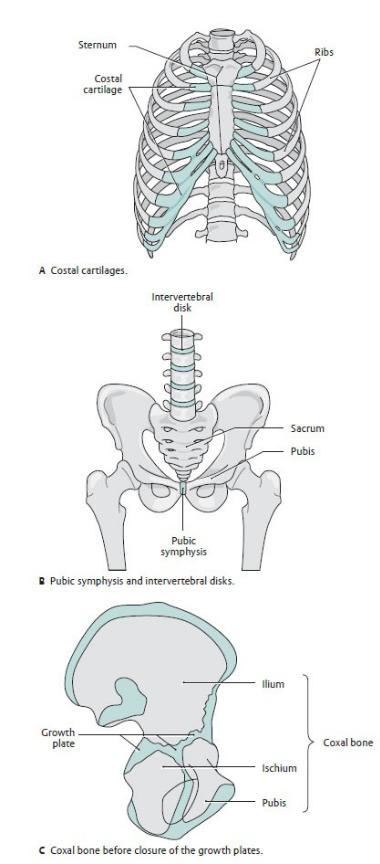
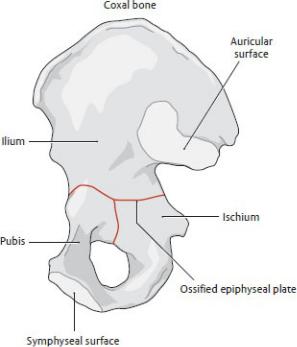
Fig. 1.8 Synchondroses
(From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
Fig. 1.9 Synostoses.
Coxal bone (fusion of the ischium, ilium, and pubis). (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
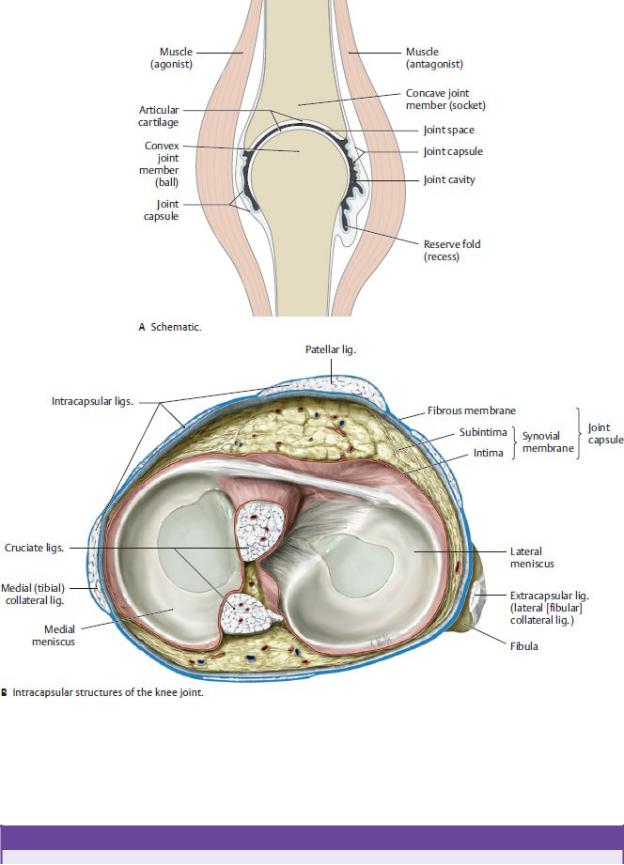
Fig. 1.10 Structure of a synovial joint
(From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
BOX 1.1: ANATOMIC NOTES
EXTRA-ARTICULAR AND INTRA-ARTICULAR STRUCTURES OF SYNOVIAL JOINTS (SEE FIG. 1.10)
The joint capsule of a synovial joint is composed of an outer fibrous membrane and an inner synovial membrane. The intima (innermost lining) of the synovial membrane produces the synovial fluid, which lubricates and nourishes intra-articular structures.
—Ligaments of synovial joints act as primary joint stabilizers. They may be:
•Extra-capsular (e.g., lateral (fibular) collateral ligament of the knee), which lie outside the fibrous capsule.
•Intra-capsular, which run either within the fibrous membrane (e.g., medial (tibial) collateral ligament of the knee) or between the fibrous and synovial membranes (e.g., cruciate ligaments).
—Menisci, articular disks, and articular labra are intra-articular structures composed of connective tissue and fibrocartilage:
•Menisci are crescent-shaped structures found in the knee joint. They act as shock absorbers and modify the incongruity of the articulating surfaces.
•Articular disks divide joints into separate chambers and are found in the sternoclavicular and proximal wrist joints.
•Articular labra are wedge-shaped structures that line the glenoid of the scapula and acetabulum of the coxal (hip) bone, thus enlarging the articular surfaces of the shoulder and hip joints.
1.7 The Muscular System
The muscular system is composed of muscles and their ten dons, which produce movement through contraction of muscle cells.
—Muscle cells are the structural units of the muscular system. Connective tissue binds muscle cells (fibers) together to form bundles, which in turn are bound together to form muscles (Fig. 1.11).
—A motor unit is the functional unit of muscles and describes the group of muscle fibers innervated by a single motor neuron. Motor units are relatively small in muscles that perform fine movements but larger in muscles that are responsible for maintaining posture or performing gross movements.
—Muscles function through tensing and contraction of the muscle fibers, which provide movement and stability
•Phasic contractions can change the length of the muscle through shortening (concentric contractions), or lengthening (eccentric
contractions), or simply increas ing the muscle tension (isometric contractions).
•Tonic contractions contribute to stability of joints and position but do not provide any movements.
•Reftexive contractions are involuntary and are responsive to muscle stretch.
—Muscle tissue is classified by location (somatic or visceral), appearance (striated or nonstriated), and innervation (voluntary or involuntary).
—Somatic, or skeletal muscles, the most prevalent type, are found in the neck, trunk wall, and limbs, where they move and support the skeleton (Fig. 1.12). They are multinucleated, striated, and voluntary.
•Somatic muscle fibers are interwoven with three sheaths of connective tissue including the endomysium, the innermost sheath, which surrounds and condenses muscle fibers into primary bundles; the perimysium, which surrounds and condenses prima ry bundles into secondary bundles; and the epimysium, a loose connective tissue layer that surrounds the muscle and lies deep to the muscle fascia.
•Muscle fascia is the tough connective tissue sheath that encloses the muscle, maintains its shape, and allows frictionless movement between muscles and muscle groups.
•Tendons, dense fibrous bands, connect muscles to their bony attachments. Aponeuroses are tendons that form flat sheets, which attach the muscle to the skeleton, other muscles, or organs.
•Muscles shapes are described according to the arrange ment of the muscle fibers as pennate (uni-, bi-, multi-), fusiform, circular, convergent, or parallel.
•Tendon (synovial) sheaths, such as those found in the wrist and ankle, facilitate the movement of tendons over bone.Similar to a synovial joint capsule, they are com posed of an outer fibrous membrane lined with a two layered synovial membrane. The space between the synovial layers is filled with synovial fluid.
—Visceral muscles, considered involuntary, alter the shape of internal structures, such as the heart and gastrointestinal tract. There are two types:
•Cardiac muscle, which makes up the thick muscular layer (myocardium) of the heart, is striated.
•Smooth muscle, which found in the walls of blood vessels and hollow internal organs, is nonstriated.
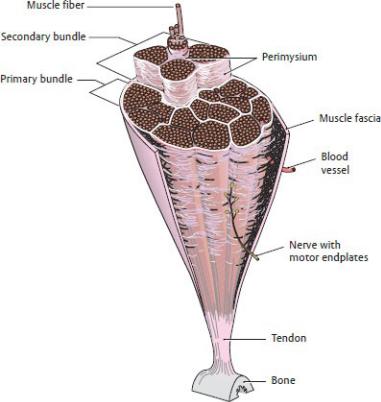
Fig. 1.11 Structure of a skeletal muscle.
Cross section through a skeletal muscle.(From Schuenke M. Schulte E. Schumacher U. THIEME Atlas of Anatomy.Vol 1. Illustrations by Vall M and Wesker K.3rd ed.New York:Thieme Publishers: 2020.)

Fig. 1.12 Overview of skeletal muscles
Some superficia I muscles have been removed or windowed on both the left (A) and right (B) side of the body.Skeletal muscles (approximately 220 individual muscles) make up the active musculo skeletaI system. Two thirds of these muscles are found in the lower limb where they support the upright sta nee ofthe body against the force of gravity.They make up an average of 40% ofthe tota I body weight (varying with gender.age.and physical condition) but decrease in mass with age. (From Schuenke M. Schulte E. Schumacher U.THIEME Atlas of Anatomy. Voll.Illustrations by Vol! M and Wesker K.3rd ed. New York:Thieme Publishers: 2020.)
1.8 The Circulatory System
The heart and blood vessels, which make up the circulatory sys-tem (Figs. 1.13 and 1.14), transport blood to tissues of the body for the exchange of gases, waste products, and nutrients.
—The muscular heart provides the pumping action that maintains the flow of blood through the vessels.
—The blood vessels of the circulatory system (Fig. 1.15) are classified as follows:
•Arteries, which transport blood away from the heart and branch into many smaller arterioles
•Veins, which carry blood toward the heart and are formed by the convergence of many small venules
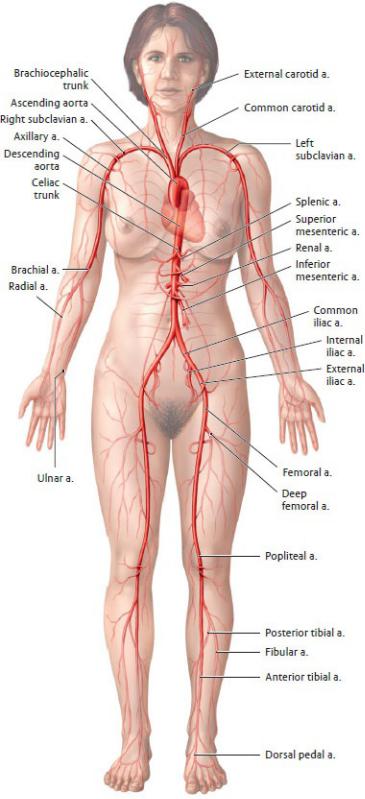
Fig. 1.13 Overview of the principal arteries in the systemic circulation.
Anterior view. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of

Anatomy, Vol 2. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)

Fig. 1.14 Overview of the principal veins in the systemic circulation.
Anterior view. The portal circulation of the liver is shown in purple. Deep veins shown on the left limb, superficial veins shown on the right limb. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 2. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
Fig. 1.15 Structure of blood vessels.
Blood vessels in different regions of the systemic circulation, shown in cross section. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
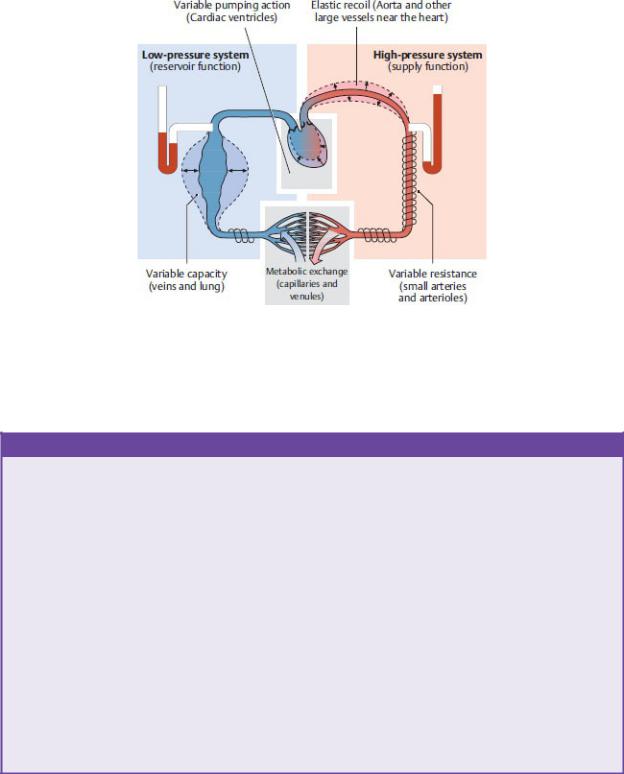
Fig. 1.16 Pressure gradients in the circulatory system.
(Note: No distinction is made between the systemic and pulmonary systems in the diagram; Klinke R, Sibernagel S. Lehbuch der Phyiologic. 3rd ed. Stuttgart: Thieme; 2001.)
BOX 1.2: ANATOMIC NOTES
FUNCTIONAL ASPECTS OF THE CIRCULATORY SYSTEM
Blood is transported through the circulatory system along a pres-sure gradient that is influenced by the size, number, and structure of the vessels through which it flows (Fig. 1.16). Relatively high pressure is maintained in the arterial system. Large elastic type arteries can accommodate the intermittent volume ejected from the heart while more distal muscular arteries, through vasodila-tion (expansion) and vasoconstriction (contraction), can control vascular resistance and regulate local blood flow.
The venous system maintains a much lower pressure, and veins have comparatively thinner walls and larger diameters. They can accommodate up to 80% of the total blood volume and there-fore serve an important reservoir function. Return of venous blood to the heart is aided by factors such as (a) venous valves that prevent backflow, (b) arteriovenous coupling that transmits the arterial pulse to accompanying veins, and (c) the pumping action of surrounding muscles
(Fig. 1.17).
Terminal vascular beds, formed by the extensive branching of capillaries, connect the arterial and venous circulations. These vascular networks are characterized by a large increase in crosssectional area and a corresponding decrease in the flow velocity, which is necessary for the exchange process between the blood and interstitial fluid. Flow through these vascular beds can be reg-ulated locally by contraction and relaxation of precapillary sphincters. Only one fourth to one third of capillary networks are perfused under normal resting conditions.
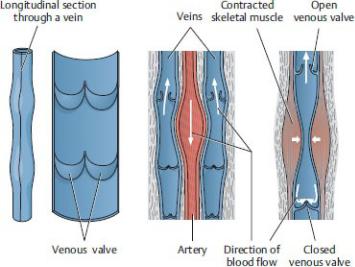
Fig. 1.17 Venous return to the heart
(From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
◦Many veins, particularly in the limbs, have multiple valves along their length to prevent backward flow due to gravity.
◦The veins are divided into superficial veins, which travel in the subcutaneous tissue and deep veins, which accompany the arteries. Perforator veins connect the superficial and deep venous circulations.
◦Veins are more numerous and more variable than arteries and often form venous plexuses (networks), which are named for the structure they surround (e.g., uterine venous plexus).
•Capillaries, which form networks that intervene between the arteries and veins at the terminal vascular beds, where gas, nutrient, and waste exchange occurs
•Sinusoids, which are wide, thin-walled vessels that replace capillaries in some organs, such as the liver
—The circulatory system has two circuits (Fig. 1.18):
1. The pulmonary circulation transports oxygen-poor blood from the right side of the heart to the lungs through pulmonary arteries. Oxygen-rich blood from the lungs flows back to the left side of the heart through pulmonary veins.
2. The systemic circulation distributes oxygen-rich blood from the left side of the heart to body tissues through the systemic arteries (the aorta
and its branches). Oxygen-poor blood returns to the heart through the systemic veins (the superior and inferior venae cavae and their tributaries—sometimes referred to as the caval system— and the coronary sinus).
—A portal circulation is a route within the systemic circulation that diverts blood to a second capillary network before returning it to the systemic veins. The largest of these, the portal system in the liver, diverts blood from the gastrointestinal tract to the capillaries (sinusoids) in the liver before returning it to the systemic veins. A similar portal system is found in the pituitary gland.
—An anastomosis, a communication between blood vessels, allows blood to bypass its normal route and flow through an alternate, or collateral, route. Although blood volume through the anastomosis is usually minimal, it increases when the lumen of vessels along the normal route is obstructed.
—End arteries are vessels that lack anastomoses, such as the central retinal artery and renal arteries. Gradual narrowing of end arteries stimulates the formation of new vessels, but an abrupt obstruction of an end artery can cause necrosis (death) of the target tissue.
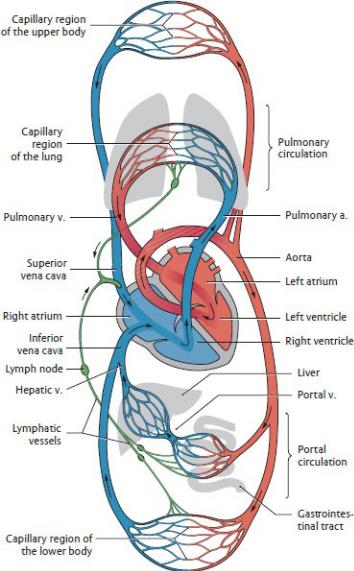
Fig. 1.18 Circulation.
Schematic showing the pulmonary and systemic circulations. The portal circulation through the liver is part of the systemic circulation. Arteries are shown in red, veins in blue, and lymphatic vessels in green. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
1.9 The Lymphatic System
The lymphatic system, which runs parallel to the circulatory sys-tem, consists of lymph, lymphatic vessels, and lymphoid organs.
— The lymphatic system performs the following functions:
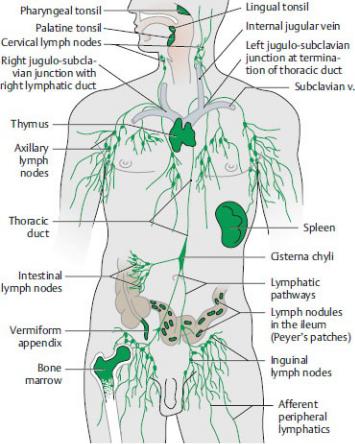
•Drains excess extracellular fluid from body tissues and returns it to veins of the systemic circulation
•Mounts an immune response in the body
•Transports fat and large protein molecules that cannot be taken up by venous capillaries
—Lymphoid organs and tissues that are part of the body’s immune system include
•primary lymphatic organs: the thymus and bone marrow
•secondary lymphatic organs: the spleen, lymph nodes, mucosaassociated lymphatic tissue (MALT), pharyngeal lymphatic (Waldeyer’s) ring, bronchus-associated lymphatic tissue (BALT) in the airway, and gut-associated lymphatic tissue (GALT)—such as Peyer’s patches and the vermiform appendix—in the gastrointestinal tract (Fig. 1.19).
Fig. 1.19 Lymphatic system.
The lymphatic system parallels the veins of the circulatory system and includes lymph nodes, lymphatic vessels, and lymphatic organs. (From Schuenke M,
Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
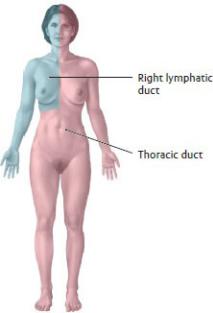
Fig. 1.20 Lymphatic drainage by body quadrants
(From Gilroy AM, MacPherson BR, Wikenheiser JC. Atlas of Anatomy. Illustrations by Voll M and Wesker K. 4th Edition. New York: Thieme Publishers; 2020.)
—Lymph, extracellular fluid that is extracted by lymph capillaries and transported by lymphatic vessels, is a clear, watery substance similar to blood plasma.
—The conducting vessels of the lymphatic system include
•blind-ended lymphatic capillaries that begin in the tissues and drain to lymphatic vessels;
•lymphatic vessels, which are interposed with lymph nodes along their length and drain to lymphatic trunks; and
•two major lymphatic trunks, the thoracic duct (left lymphatic trunk) and right lymphatic trunk, which drain into large veins of the neck.
—The left lymphatic trunk, or thoracic duct, (~ 40 cm long), is the larger of the two major lymphatic trunks. It originates from the cisterna chyli, a dilated lymphatic vessel in the abdomen, and drains lymph from the right and left lower quadrants and left upper quadrant of the body. The smaller right lymphatic duct (~ 1 cm long) drains only the right upper quadrant of the body (Fig. 1.20).
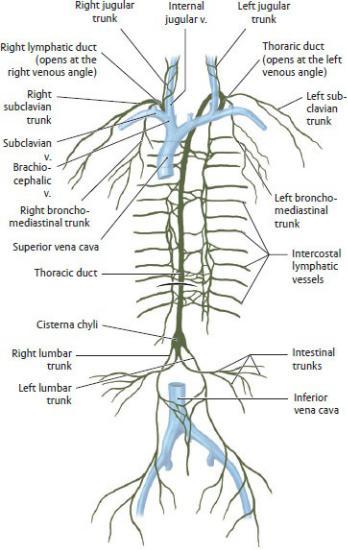
—Lymph carried by the thoracic duct and right lymphatic duct returns to the systemic venous circulation at the left and right venous angles (junction of the internal jugular and subclavian veins), also known as the jugulosubclavian junction, in the neck (Fig. 1.21).
—Tributaries of the thoracic duct (left lymphatic trunk) include the:
• left jugular trunk, which drains the left half of the head and neck
Fig. 1.21 Lymphatic pathways.
Anterior view. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
•left subclavian trunk, which drains the left upper limb, left sides of the
chest, and back wall
•left bronchomediastinal trunk, which drains viscera of the left thoracic cavity (except from the lower lobe of the left lung, which can drain to the right lymphatic trunk). This trunk commonly empties directly into the left subclavian vein.
•intestinal trunks from the abdominal organs
•right and left lumbar trunks , which drain both lower limbs, all of the pelvic viscera, and walls of the pelvis and abdomen
—Tributaries of the right lymphatic duct include the:
•right jugular trunk, which drains the right half of the head and neck
•right subclavian trunk, which drains the right upper limb and right sides of the chest and back walls
•right bronchomediastinal trunk, which drains the viscera of the right thoracic cavity. This trunk commonly empties directly into the right subclavian vein.
1.10 The Nervous System
The nervous system receives, transmits, and integrates informa-tion throughout the body through the conduction of nerve impulses. This complex system can be classified according to many different criteria. Although these classifications are somewhat artificial, they are useful for understanding the numerous interconnections within the nervous systems (Fig. 1.22).
—The nervous system has two major structural, or anatomic, divisions (Fig. 1.23):
•A central nervous system (CNS), which consists of the brain and spinal cord, where information about the body’s internal and external environment is processed
•A peripheral nervous system (PNS), which consists of 12 pairs of cranial nerves, 31 pairs of spinal nerves, and autonomic (visceral) nerves; peripheral nerves transmit information between the CNS and target organs and tissues in the rest of the body.
—The nervous system can also be divided into functional divisions (Fig. 1.24). Both the CNS and PNS contain compo-nents of each functional division.
•The somatic nervous system controls voluntary functions such as contraction of skeletal muscles.
•The autonomic (visceral) nervous system controls involuntary
functions such as gland secretion.
—Nerve cells or neurons, the functional unit of the nervous system found in the CNS and PNS, are specialized for conducting nerve impulses. They generate electrical signals, the action potential, and pass them on to other nerve or muscle cells. A variety of neurons can be described based on their appearance but the basic structure remains similar. The typical neuron (Fig. 1.25A) has
•a cell body (soma). An aggregate of cell bodies in the CNS is called a nucleus; an aggregate of cell bodies in the PNS is called a ganglion.
•multiple short branching dendrites, which receive information from other neurons and transmit impulses toward the cell body.
•a single long axon or nerve fiber, which transmits impulses away from the cell body. Bundles of axons in the CNS form tracts; bundles of axons in the PNS form nerves.
—Neurons transmit electrical signals from cell to cell across junctions called synapses. At the synapse the electrical impulse of the presynaptic nerve fiber initiates the release of a chemical signal, or transmitter, which generates an electrical impulse in the receptor, or postsynaptic nerve cell
(Fig 1.25B).
—Neurons are classified by function as
•sensory (afferent) nerves, which carry information regarding pain, temperature, and pressure to the CNS from peripheral structures.
•motor (efferent) nerves, which transmit impulses from the CNS that elicit responses from peripheral target organs.
—Neuroglia, or glial cells, the non -neuronal cellular compo-nents of the nervous system, act as supporting cells and perform a variety of metabolic functions. Glial cells are responsible for producing the myelin sheath, a lipid-rich layer that surrounds axons and increases the speed of impulse conduction (Fig. 1.26). The myelin-producing cells in the PNS are called
Schwann cells and in the CNS are called oligodendrocytes.
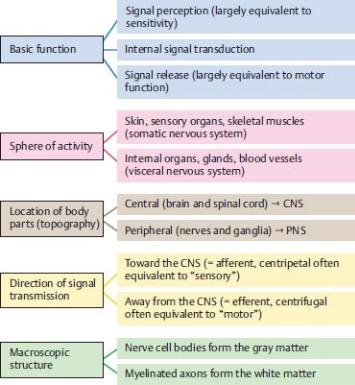
Fig. 1.22 Classification of the nervous system—overview
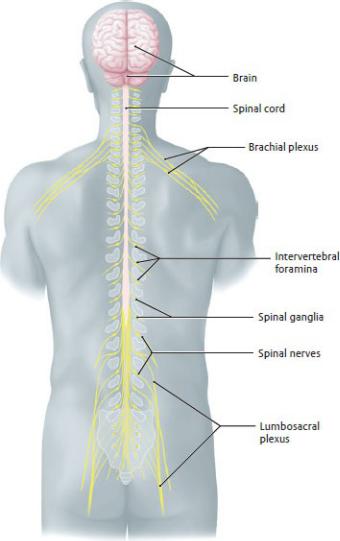
Fig. 1.23 Topography of the nervous system.
Posterior view. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
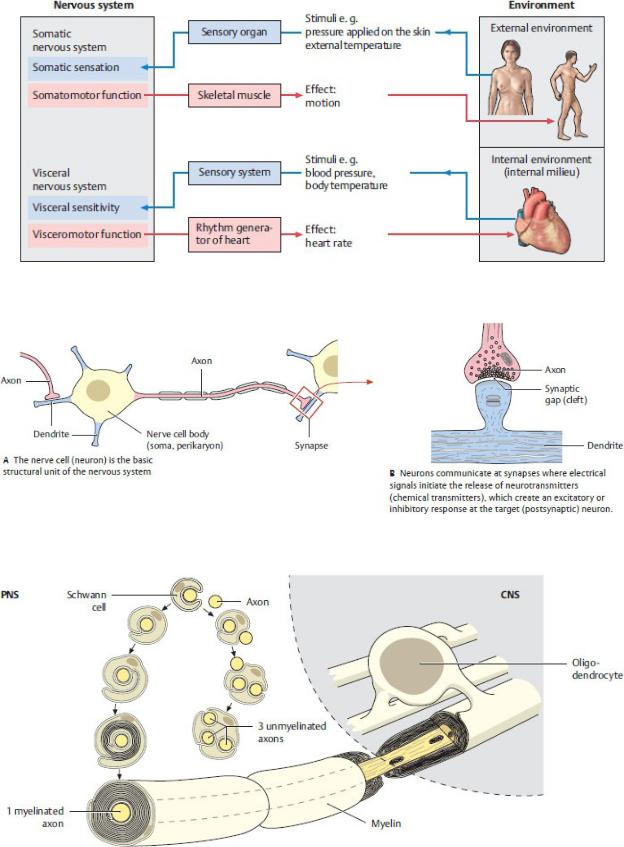
Fig. 1.24 Functional classification of the nervous system
Fig. 1.25 Nerve cell and synapse
Fig. 1.26 Glial cells in the CNS and PNS.
Glial cells form myelin sheaths around axons. This increases the speed with which impulses travel in the nervous system. In myelinated axons, multiple layers of glial membrane surround a single axon forming a distinct myelin sheath. In unmyelinated axons, a glial cell surrounds and supports multiple axons without forming a myelin sheath. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
The Central Nervous System
The detailed anatomy of the central nervous system is most appro-priately described in texts on neuroanatomy, and therefore is not included in this text. However, because an appreciation of its struc-ture is essential to understanding the functioning of peripheral structures, a brief overview is included here, with further discus-sions to follow in Section 2.2 (spinal cord) and Section 18.2 (brain).
—The brain and spinal cord of the central nervous system (Fig. 1.27) consist of
•gray matter, which contains the cell bodies, dendrites, and unmyelinated axons of neurons;
•white matter, which contains the myelinated axons of neurons; and
•neuroglial cells, which are abundant in both white and gray matter.
—The brain resides in the cranial cavity of the skull. The tissue of the brain consists of an outer cerebral cortex of gray matter, an inner core of white matter, and islands of gray matter deep within the brain known as basal ganglia. Axonal tracts of the white matter link regions of the brain with each other and with the spinal cord.
—The brain (Fig. 1.28) is subdivided into
•cerebral hemispheres
•diencephalon
•cerebellum
•brainstem
—The bony vertebral column encloses the spinal cord. Gray matter in the spinal cord is located centrally and is sur-rounded by white matter tracts. The gray matter forms an H-shaped area that consists of bilateral
•anterior horns, which contain motor neurons;
•posterior horns, which contain sensory neurons;
•lateral horns in the thoracic and upper lumbar region, which contain visceromotor neurons.
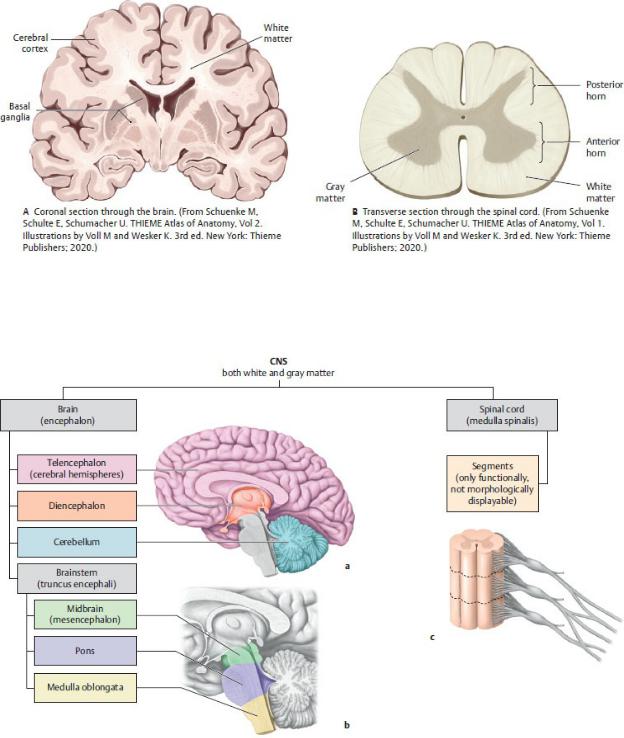
Fig. 1.27 Gray and white matter in the central nervous system.
Nerve cell bodies appear gray in gross inspection, whereas nerve cell processes (axons) and their insulating myelin sheaths appear white.
Fig. 1.28 Structure of the central nervous system.
A,B-Right side of brain, medial view. C-Anterior view of a section of the spinal cord. (From Gilroy AM, MacPherson BR, Wikenheiser JC. Atlas of Anatomy. Illustrations by Voll M and Wesker K. 4th Edition. New York: Thieme
Publishers; 2020.)
The Peripheral Nervous System
—The peripheral nervous system includes the peripheral parts of the autonomic and somatic divisions. Components of each system (Fig. 1.29) are found in
•12 pairs of cranial nerves (traditionally designated, in order from cranial to caudal, by Roman numeral) that arise from the brain and primarily innervate structures of the head and neck. The vagus nerve (cranial nerve X) also innervates viscera of the thorax and abdomen.
•31 pairs of spinal nerves that arise from the spinal cord and exit the vertebral column through intervertebral foramina (openings between vertebrae). Spinal nerves are named for the section of the spinal cord from which they arise (e.g., T4 is the fourth segment of the thoracic part of the spinal cord).
—Most nerves of the peripheral nervous system are mixed nerves that contain both motor and sensory fibers (Fig. 1.30).
•The somatic nervous system contains a combination of fiber types:
◦somatic sensory (somatosensory) fibers, which transmit the information from skin and skeletal muscles
◦somatic motor (somatomotor) fibers, which innervate skeletal muscles
•The autonomic nervous system contains only visceral motor (visceromotor) fibers, which innervate smooth muscle, cardiac muscle, and glands.
•Visceral sensory (viscerosensory) fibers transmit information from smooth muscle, cardiac muscle, and internal organs. Although these often accompany the visceral motor fibers, they are generally not considered part of the autonomic system.
•In addition to those named above, cranial nerves may also contain special fiber types that are associated with structures in the head:
◦Special somatic sensory (somatomotor) fibers, which conduct information from the retina of the eye, and auditory and vestibular apparatus of the ear
◦Special visceral sensory (viscerosensory) fibers, which transmit information from the taste buds of the tongue and olfactory mucosa
◦Special visceral motor fibers (visceromotor, branchio-motor), which innervate skeletal muscles that originate from the branchial arches
—The somatic component of the nervous system transmits the motor output to, and sensory input from, structures over which we have voluntary and conscious control. (Consider a simple activity like walking, in which we have control over the movement of our legs and are aware of the pain elicited by an arthritic knee joint or a splinter in the sole of the foot.)
—The autonomic component transmits the motor output to structures that function without conscious control. Its two divisions work to excite
(sympathetic) or relax (parasympa-thetic) visceral responses based on internal and external stimuli. Together they work to maintain a stable (homeo-static) internal environment. (Consider the increase in heart rate when you have won the lottery and the crucial corre-sponding slowing of the heart rate when you need to sleep.)
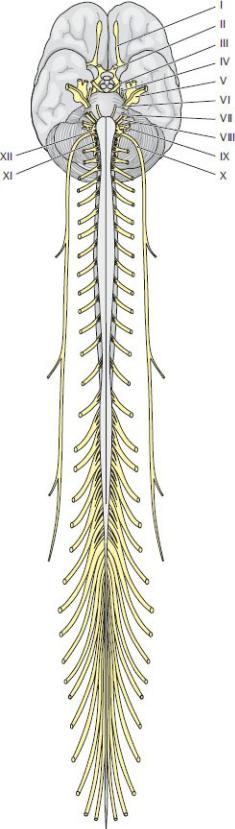
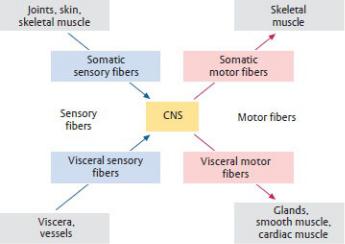
Fig. 1.29 Spinal nerves and cranial nerves.
Anterior view. Thirty-one pairs of spinal nerves arise from the spinal cord in the peripheral nervous system, compared with 12 pairs of cranial nerves that arise from the brain. The cranial nerve pairs are traditionally designated by Roman numerals. (From Gilroy AM, MacPherson BR, Wikenheiser JC. Atlas of Anatomy. Illustrations by Voll M and Wesker K. 4th Edition. New York: Thieme Publishers; 2020.)
Fig. 1.30 Information flow in the nervous system.
Fibers that carry information to the central nervous system (CNS) are called sensory or afferent fibers; fibers that carry signals away from the CNS are called motor or efferent fibers.
—The somatic and autonomic nervous systems each have their own network of nerves that transmit information between the CNS and PNS. Although somatic and autonomic nerves may travel together, the nerve fibers remain anatomically and functionally distinct.
—Most cranial nerves and all spinal nerves carry somatic nerve fibers; some also carry autonomic fibers:
•parasympathetic fibers are carried by cranial nerves III, VII, IX, and X and spinal nerves S2–S4
•sympathetic fibers originate at spinal cord levels T1–L2 but, via the sympathetic trunk, are distributed to, and travel with, spinal nerves at all levels.
—Nerves from each system typically form nerve plexuses (i.e., somatic nerve plexus, autonomic nerve plexus). Each contains nerves arising from multiple levels of the spinal cord.
•Somatic plexuses are made up of large, distinct, easily identifiable nerve roots and give rise to nerves that are given descriptive names (median n., femoral n.).
•Autonomic plexuses appear as dense mats of thin hair-like nerves that frequently extend peripherally along major arteries.
—Both somatic and autonomic nerves carry motor information from the CNS to a peripheral structure, but the type of target organ they innervate and the response they elicit is very different.
•Somatic nerves initiate voluntary responses (such as contraction of the biceps).
•Autonomic nerves initiate visceral responses (such as secretion of pancreatic juices).
—Somatic sensory and visceral sensory nerves carry sensory information from target organs to the CNS.
•Sensations carried by visceral sensory fibers are vague and poorly localized (such as nausea).
•Sensations carried by somatic sensory fibers are sharp and localized (such as a paper cut).
•In all cases, the cell bodies of peripheral sensory neurons lie in sensory (spinal/dorsal root) ganglia that lie outside the CNS.
—Splanchnic nerves are nerves of the autonomic nervous system that innervate visceral structures (splanchnic refers to internal organs or viscera). They may carry either sympathetic or parasympathetic fibers (never both) and contain no somatic fibers. All splanchnic nerves contain visceral sensory and visceral motor fibers.
1.11 Body Cavities and Internal Organ Systems
The large organs of the endocrine, respiratory, digestive, urinary, and reproductive systems are housed in the thoracic, abdominal, and pelvic cavities. These large spaces are divided into serous cav-ities and connective tissue spaces.
—A serous cavity is a fully enclosed potential space that is lined by a serous (fluid secreting) membrane. The outer, or parietal, layer of this membrane lines the inner wall of the cavity. It is continuous with the inner, or visceral, layer that reflects from the wall to cover or enclose the viscera within the cavity. The large serous cavities include:
• In the thorax
◦ paired pleural cavities, which contain the lungs
◦a pericardial cavity, which contains the heart
•In the abdomen and pelvis
◦a peritoneal cavity, which contains the gastrointestinal tract and its accessory structures
—Connective tissue spaces are potential spaces that lie outside the serous cavities. They are often defined by adjacent layers of fascia or may lie between opposing serous cavities. Major examples include:
•The deep cervical space between fascial layers of the neck
•The mediastinum, which lies between the pleural cavities in the thorax
•The retroperitoneal space, which lies posterior to the peritoneal cavity in the abdomen, and its continuation into the pelvis below the peritoneum, where it is known as the subperitoneal space. Urinary and reproductive organs, as well as the major vascular structures, reside within these extraperitoneal spaces.
