
- •Contents
- •Acknowledgments
- •Preface to the Third Edition
- •1 Introduction to Anatomic Systems and Terminology
- •2 Clinical Imaging Basics Introduction
- •3 Back
- •4 Clinical Imaging Basics of the Spine
- •5 Overview of the Thorax
- •6 Thoracic Wall
- •7 Mediastinum
- •8 Pulmonary Cavities
- •9 Clinical Imaging Basics of the Thorax
- •10 The Abdominal Wall and Inguinal Region
- •12 Abdominal Viscera
- •13 Clinical Imaging Basics of the Abdomen
- •14 Overview of the Pelvis and Perineum
- •15 Pelvic Viscera
- •16 The Perineum
- •18 Overview of the Upper Limb
- •19 Functional Anatomy of the Upper Limb
- •20 Clinical Imaging Basics of the Upper Limb
- •21 Overview of the Lower Limb
- •22 Functional Anatomy of the Lower Limb
- •23 Clinical Imaging Basics of the Lower Limb
- •24 Overview of the Head and Neck
- •25 The Neck
- •26 Meninges, Brain, and Cranial Nerves
- •29 Clinical Imaging Basics of the Head and Neck
- •Index

5 Overview of the Thorax
The thorax is the region of the trunk between the neck and abdo-men. The thoracic cavity, surrounded by a bony cage that protects the thoracic contents, is open to the neck through the superior thoracic aperture but separated from the abdomen at the inferior thoracic aperture by a muscular diaphragm. The viscera of the thorax include the primary organs of the respiratory and cardio-vascular systems, as well as components of the gastrointestinal, endocrine, and lymphatic systems.
5.1 General Features
—The thorax is divided into two lateral compartments, the pulmonary cavities, which contain the lungs and pleural sacs, and a central compartment, the mediastinum, which contains the heart, pericardial sac, trachea and bronchi, esophagus, thymus, and neurovasculature (Fig. 5.1; Table 5.1).
—A pericardial sac surrounds the heart, and a pleural sac surrounds each lung. These closed membranous sacs contain a thin layer of serous fluid that ensures frictionless move-ment, which is crucial to the function of these organs.
—The lungs are the organs of respiration. They communicate with the tracheobronchial tree (the passages for air between the lungs and outside environment) and the heart through the hilum, an indentation on the medial surface of each lung.
—The heart is a four-chambered muscular organ that functions as a dual pump that propels blood through the body. Each pump is made up of two chambers: a thin-walled atrium and a thick-walled ventricle.
—During a cardiac cycle, the right pump receives deoxygenated blood from the systemic circulation (circulation of blood through all regions of the body except the lungs) and directs it to the pulmonary circulation in the lungs. The left pump receives oxygenated blood from the pulmonary circulation and returns it to the systemic circulation for the distribution of

oxygen and nutrients (Fig. 5.2).
—Coordinated contraction of atria and ventricles, known as the cardiac cycle, is self-moderated by specialized tissue within the cardiac muscle that makes up the heart’s conduction system.
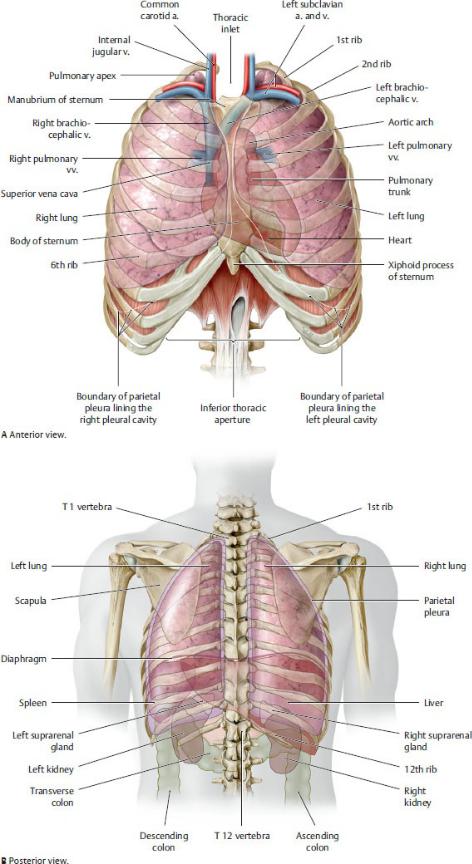
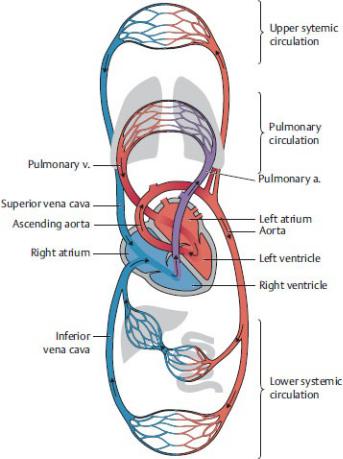
Fig. 5.1 Overview of the thorax
(From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 2. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers;
Fig. 5.2 Systemic and pulmonary circulation
Red, oxygenated blood; blue, deoxygenated blood. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 1. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
5.2 Neurovasculature of the Thorax
The “great vessels,” which include the pulmonary arteries and veins, the aorta, the superior vena cava, and the inferior vena cava, direct blood into and out of the heart and lungs. Their branches and further details of their anatomy, along with more detailed descriptions of lymphatic drainage and nerves of the thorax, are discussed in Chapters 7 and 8 on the mediastinum and pulmonary cavities.
Arteries of the Thorax
—The pulmonary trunk directs deoxygenated blood from the right side of the heart into the pulmonary circulation. It arises from the right ventricle on the anterior surface of the heart, passes superiorly and posteriorly, and, under the arch of the aorta, divides into right and left pulmonary arteries (Fig. 5.3).
—One pulmonary artery enters each lung, where it branches into generations of smaller vessels that accompany the respi-ratory passages. The pulmonary arteries transport deoxygen-ated blood to the small respiratory units in the lungs.
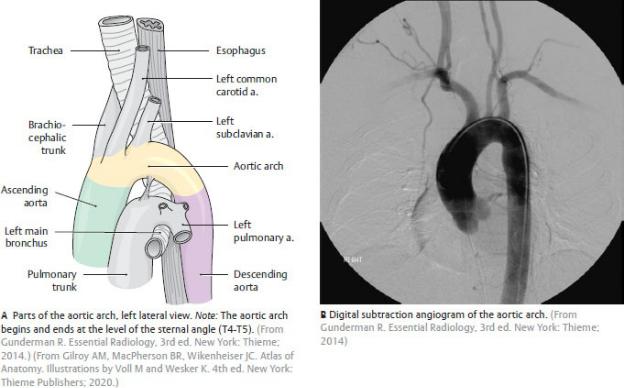
—The thoracic aorta arises from the left side of the heart and carries oxygenated blood that is distributed to the systemic circulation. It is divided into three sections (Fig. 5.4):
•The ascending aorta arises from the left ventricle of the heart and ascends to the level of the fourth thoracic vertebra. The right and left coronary arteries are its only branches.
•The aortic arch (radiographically, the “aortic knob”) ascends anterior to the right pulmonary artery and the bifurcation of the trachea (where the trachea splits into right and left bronchi). It courses posteriorly and to the left, arching over the structures entering the left lung, and then turns inferiorly to descend to the left of the trachea and esophagus. It terminates on the left side of the T4 vertebral body. Three large branches arise from the arch:
◦The brachiocephalic trunk, which ascends posterior to the right sternoclavicular joint, where it bifurcates into the right common carotid and right subclavian arteries.
◦The left common carotid artery, which enters the neck posterior to the left sternoclavicular joint.
◦The left subclavian artery, which arises from the distal segment of the arch and enters the neck posterior to the left sternoclavicular joint.
•The descending aorta, a continuation of the aortic arch, descends within the posterior mediastinum, where it passes posterior to the root of the left lung and anterior and to the left of the thoracic vertebral bodies. It passes into the abdomen through the diaphragm at T12. Its thoracic branches (Fig. 5.5; Table 5.2) are
◦the 3rd through 11th posterior intercostal arteries (the 1st and 2nd arise from the subclavian artery), which run anteriorly within the corresponding intercostal spaces (between the ribs), where they

anastomose with the anterior intercostal arteries; and
◦the visceral branches to the esophagus, trachea, bronchi, and pericardium.
—The internal thoracic arteries arise from the subclavian arteries in the neck and descend deep to the ribs on either side of the sternum. Their branches, which supply the thoracic and abdominal walls include (Fig. 5.6):
•the anterior intercostal arteries, which run within the intercostal spaces;
•the musculophrenic arteries, terminal branches of the internal thoracic arteries, which arise at the level of the sixth costal cartilage and follow the lower margin of the rib cage laterally; and
•the superior epigastric arteries, terminal branches of the internal thoracic arteries, which run inferiorly to supply muscles of the anterior abdominal wall.
Fig. 5.3 Pulmonary arteries and veins
Distribution of the pulmonary arteries and veins, anterior view. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 2. Illustra-tions
by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
Fig. 5.4 Thoracic aorta
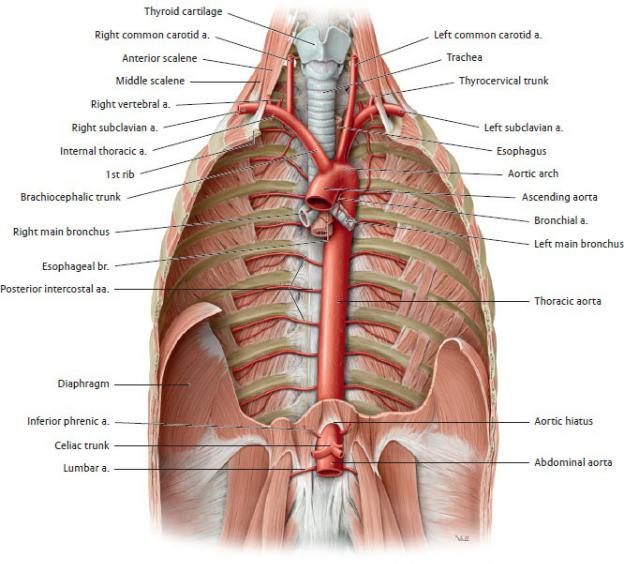
Fig. 5.5 Thoracic aorta in situ, anterior view
Removed: Heart, lungs, and portions of the diaphragm. (From Gilroy AM, MacPherson BR, Wikenheiser JC. Atlas of Anatomy. Illustrations by Voll M and Wesker K. 4th ed. New York: Thieme Publishers; 2020.)

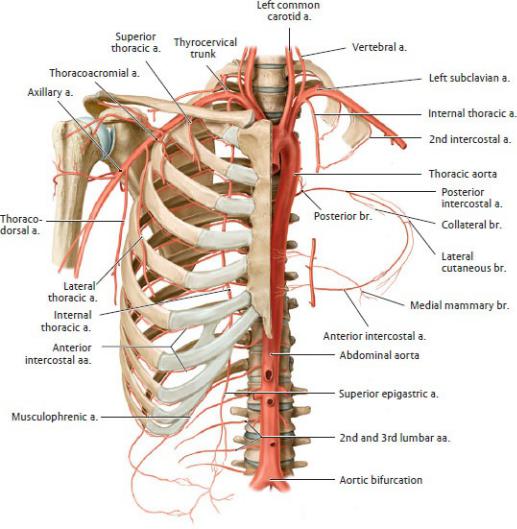
Fig. 5.6 Arteries of the thoracic wall
Anterior view. (From Gilroy AM, MacPherson BR, Wikenheiser JC. Atlas of Anatomy. Illustrations by Voll M and Wesker K. 4th ed. New York: Thieme Publishers; 2020.)
Veins of the Thorax (Fig. 5.7)
—Internal thoracic veins, which receive the anterior intercos-tal veins, accompany the internal thoracic arteries and drain into the brachiocephalic veins of the superior mediastinum.
—The right and left brachiocephalic veins, which drain the head, neck, and upper limb, form behind the clavicle by the convergence of the internal jugular and subclavian veins. The left brachiocephalic vein, which is longer than the right, crosses the midline just anterior to the branches of the aortic arch and converges with the right brachiocephalic vein to form the superior
vena cava.
—The superior vena cava, which returns deoxygenated blood from the upper body to the heart, forms on the right side, posterior to the costal cartilage of the first rib by the junction of the brachiocephalic veins. It descends behind and to the right side of the aorta and drains into the superior pole of the right atrium.
—The inferior vena cava, which returns deoxygenated blood to the heart from the abdomen, pelvis, and lower limbs, enters the right atrium after passing through the diaphragm from the abdomen. Only a small portion, therefore, is located within the thorax.
—The pulmonary veins, two on each side (often three on the left side), carry oxygenated blood from the lungs to the left side of the heart (see Fig. 5.3).
—The azygos system drains veins of the thoracic and antero lateral abdominal walls (Figs. 5.7 and 5.8).
•The azygos vein ascends along the right side of the thoracic vertebral bodies as it drains the posterior intercostal veins of the thoracic wall on that side. It arches over the root of the right lung to empty into the superior vena cava.
•The accessory hemiazygos and hemiazygos veins run along the left side of the thoracic vertebrae and drain the thoracic wall on the left side. They cross the midline inde-pendently (or they may join to form a single vessel) to drain into the azygos vein on the right side.
•The azygos and hemiazygos veins are the continuations of the ascending lumbar veins in the abdomen, which communicate with the inferior vena cava. Thus the azygos system links the drainages of the superior and inferior vena cavae and provides a collateral (alternate) pathway for blood back to the heart.
•Mediastinal, esophageal, and bronchial veins in the thorax, and the vertebral venous plexus (see Section 3.2) are also tributaries of the azygos system.
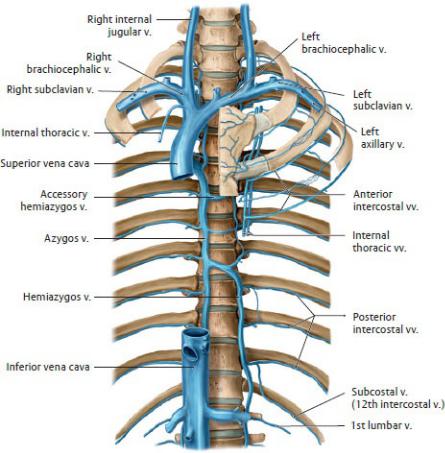
Fig. 5.7 Veins of the thoracic wall
Anterior view with rib cage opened. Removed: Clavicle. (From Gilroy AM, MacPherson BR, Wikenheiser JC. Atlas of Anatomy. Illustrations by Voll M and Wesker K. 4th ed. New York: Thieme Publishers; 2020.)
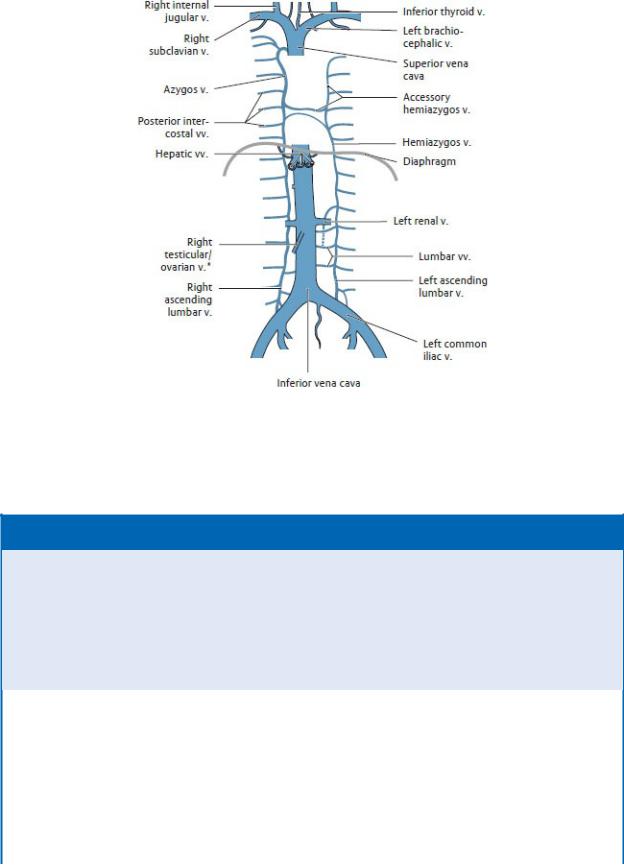
Fig. 5.8 Azygos system
Anterior view. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 2. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
BOX 5.1: CLINICAL CORRELATION
SUPERIOR VENA CAVA SYNDROME
The superior vena cava syndrome is an obstruction of the superior vena cava (SVC), which in the majority of cases is caused by mediastinal tumors such as metastatic lung carcinoma (the upper lobe of the right lung lies next to the SVC), lymphoma, breast cancer, or thyroid cancer. Noncancerous causes include thromboses (blood clots) that obstruct the lumen and infections that produce scarring. The onset of symptoms is usually gradual and includes dyspnea (shortness of breath) and swelling of the face, neck, and arms.
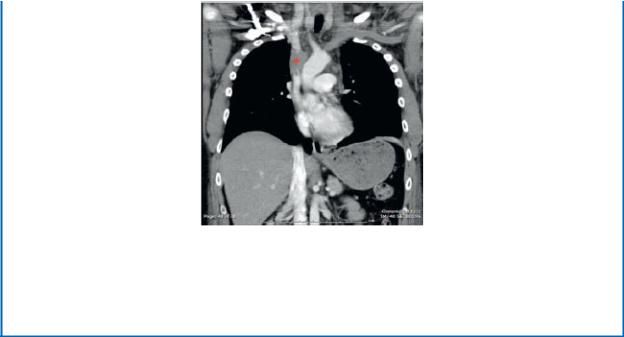
A coronal computed tomography (CT) scan image with intravenous (IV) contrast demonstrates a hypodense mass (*) occluding the superior vena cava (SVC), causing a swelling of the face and upper limbs. (From Gunderman R. Essential Radiology, 3rd ed. New York: Thieme Publishers; 2014)
Lymphatics of the Thorax (see Section 1.9)
—The thoracic duct, the main lymphatic vessel of the body,
•drains the abdomen, pelvis, and lower limbs, and the left side of the thorax, head, neck, and left upper limb (except the lower lobe of the left lung; see Section 8.5);
•enters the thorax from its origin in the abdomen and passes superiorly in the midline of the posterior mediastinum; and
•terminates at the junction of the left subclavian and left internal jugular veins (jugulosubclavian junction or “venous angle”) in the neck.
—The right lymphatic duct, which has a variable form,
•drains lymph from the right side of the thorax, the lower lobe of the left lung, the head, and neck, and the right upper limb; and
•usually terminates at the junction of the right subclavian and right internal jugular veins (the jugulosubclavian junction).
—Lymph from most thoracic structures drains through chains of lymph nodes that empty into bronchomediastinal trunks in the mediastinum (Figs. 5.9 and 5.10). This includes
•parasternal and intercostal lymph nodes of the thoracic wall and superior surface of the diaphragm;
•bronchopulmonary and intrapulmonary lymph nodes of the lungs and bronchi; and
•tracheobronchial, paratracheal, and paraesophageal lymph nodes of the
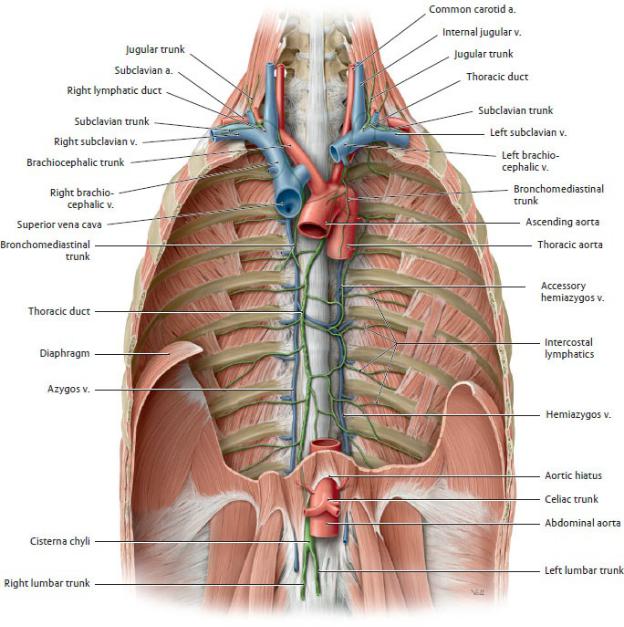
heart, pericardium, trachea, and esophagus.
—The bronchomediastinal trunks may empty into the thoracic and right lymphatic ducts, but, more commonly, they empty directly into the subclavian veins in the neck.
Fig. 5.9 Lymphatic trunks in the thorax
Anterior view of opened thorax. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 2. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
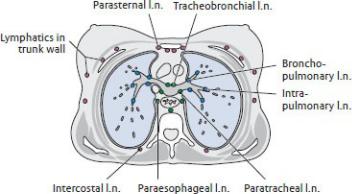
Fig. 5.10 Thoracic lymph nodes
Transverse section at the level of the tracheal bifurcation (at approxi-mately T4), viewed from below. Topographically, the thoracic lymph nodes can be divided into three broad groups:
—Lymph nodes in the thoracic wall (pink)
—Lymph nodes in the lung and at the divisions of the bronchial tree (blue)
—Lymph nodes associated with the trachea, esophagus, and pericardium
(green)
(From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 2. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
Nerves of the Thorax (Figs. 5.11, 5.12, 5.13, 5.14)
—Pairs of posterior intercostal nerves arise from the anterior rami of T1– T11 and pass along the inferior edge of the ribs on their deep surface.
•The nerves innervate the muscles between the ribs, over-lying muscles and skin of the thoracic wall and the breast.
—Phrenic nerves arise in the neck from anterior rami of C3, C4, and C5 (“to keep the diaphragm alive”) and descend into the thorax.
•On the right, the nerve runs along the superior vena cava; on the left, it descends along the lateral side of the aortic arch.
•Both nerves pass anterior to the hila of the lungs as they descend to the diaphragm between the pericardial and pleural sacs.
•The phrenic nerves provide motor innervation to the diaphragm and transmit sensory input from the mediasti-num, mediastinal and diaphragmatic pleura, and perito-neum on the inferior diaphragmatic surface.
—The thoracic sympathetic trunks run along either side of the thoracic vertebral column.

Fig. 5.11 Nerves of the thorax
Anterior view of opened thorax. (From Schuenke M, Schulte E, Schumacher U. THIEME Atlas of Anatomy, Vol 2. Illustrations by Voll M and Wesker K. 3rd ed. New York: Thieme Publishers; 2020.)
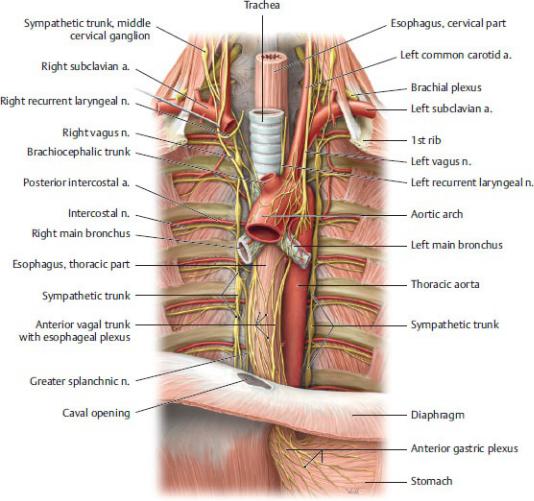
Fig. 5.12 Nerves of the posterior mediastinum
Anterior view. (From Gilroy AM, MacPherson BR, Wikenheiser JC. Atlas of Anatomy. Illustrations by Voll M and Wesker K. 4th ed. New York: Thieme Publishers; 2020.)

Fig. 5.13 Esophageal plexus
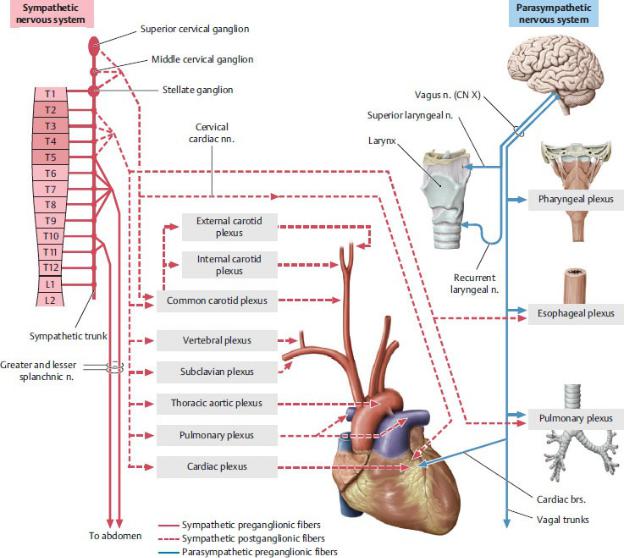
Fig. 5.14 Sympathetic and parasympathetic nervous systems in the thorax
Schematic. (From Gilroy AM, MacPherson BR, Wikenheiser JC. Atlas of Anatomy. Illustrations by Voll M and Wesker K. 4th ed. New York: Thieme Publishers; 2020.)
•Sympathetic (paravertebral) ganglia at each spinal level communicate with spinal nerves through white and gray rami communicans.
•The T1 ganglion may combine with the ganglion at C8 to form a large stellate (star-shaped) ganglion.
•Small splanchnic nerves, course medially from the sympathetic trunk, to contribute to the autonomic plexuses of the thorax, which innervate thoracic viscera.
—Three large additional splanchnic nerves arise from the thoracic sympathetic
trunk on each side, the greater (T5–T9 or T10), lesser (T10–T11), and least (T12) splanchnic nerves, and course inferomedially along the thoracic vertebral bodies into the abdomen. They contain preganglionic fibers that synapse in prevertebral ganglia of abdominal autonomic nerve plexuses
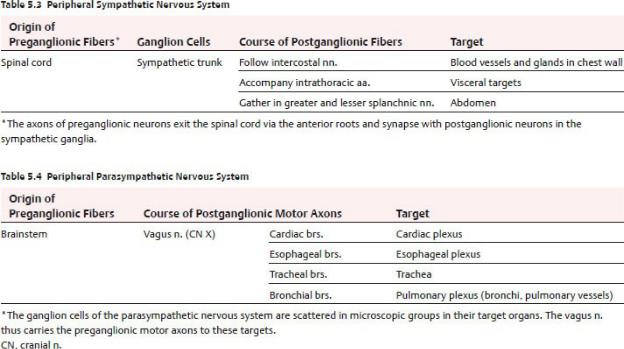
(Table 5.3).
—The vagus nerves (cranial nerve X) descend from the neck into the thorax.
•The right vagus courses behind the superior vena cava, medial to the arch of the azygos vein; the left vagus runs lateral to the aortic arch.
•Both vagus nerves pass posterior to the hilum of the lung before merging on the wall of the esophagus.
•The vagus nerves contribute parasympathetic fibers to the cardiac, pulmonary, and esophageal plexuses (Table 5.4).
—The left recurrent laryngeal nerve, a branch of the left vagus nerve, passes under the aortic arch, posterior to the ligamen-tum arteriosum (see Section 5.6), and turns superiorly to ascend in the neck in the groove between the trachea and esophagus.
•The right recurrent laryngeal nerve, a branch of the right vagus, recurs around the subclavian artery in the neck and is not a thoracic structure.
—The esophageal plexus surrounds the lower esophagus.
•It is composed of preganglionic parasympathetic fibers from the right and left vagus nerves and postganglionic fibers from the thoracic
sympathetic trunk.
•Anterior and posterior vagal trunks arise from the plexus and pass into the abdomen, anterior and posterior to the esophagus.
—The cardiac plexus (Fig. 5.13), which is located above the heart in the concavity of the arch of the aorta, continues along the coronary arteries. It innervates the conducting system of the heart and contains
•preganglionic sympathetic fibers from T1 to T5 and postganglionic sympathetic fibers from cardiopulmonary branches of the cervical and thoracic sympathetic trunk;
•preganglionic parasympathetic fibers from cardiac branches of the vagus nerve that arise in the cervical region and contributions from the recurrent laryngeal nerves; and
•visceral sensory fibers that travel with sympathetic and parasympathetic nerves.
—The pulmonary plexus is a continuation of the cardiac plexus onto the bifurcation of the trachea and the bronchi that pene-trate the hilum of each lung.
•It regulates the constriction and dilation of the pulmonary vessels and respiratory passages.
•It transmits sensation from the lung and visceral, or inner, layer of the pleural sac that is adherent to the surface of the lung.
