
- •Table of Contents
- •Front matter
- •Copyright
- •Preface to the twelfth edition
- •Preface to the eleventh edition
- •Preface to the tenth edition
- •Acknowledgements
- •Chapter 1. Introduction to regional anatomy
- •2. Upper limb
- •Part two. Shoulder
- •Part three. Axilla
- •Part four. Breast
- •Part five. Anterior compartment of the arm
- •Part six. Posterior compartment of the arm
- •Part eight. Posterior compartment of the forearm
- •Part nine. Wrist and hand
- •Part ten. Summary of upper limb innervation
- •Part eleven. Summary of upper limb nerve injuries
- •Part twelve. Osteology of the upper limb
- •Chapter 3. Lower limb
- •Part two. Medial compartment of the thigh
- •Part three. Gluteal region and hip joint
- •Part four. Posterior compartment of the thigh
- •Part five. Popliteal fossa and knee joint
- •Part six. Anterior compartment of the leg
- •Part seven. Dorsum of the foot
- •Part eight. Lateral compartment of the leg
- •Part nine. Posterior compartment of the leg
- •Part ten. Sole of the foot
- •Part eleven. Ankle and foot joints
- •Part twelve. Summary of lower limb innervation
- •Part thirteen. Summary of lower limb nerve injuries
- •Part fourteen. Osteology of the lower limb
- •Chapter 4. Thorax
- •Part one. Body wall
- •Part three. Thoracic cavity
- •Part five. Anterior mediastinum
- •Part eight. Pleura
- •Chapter 5. Abdomen
- •Part two. Abdominal cavity
- •Part nine. Spleen
- •Part eleven. Kidneys, ureters and suprarenal glands
- •Part twenty. Female urogenital region
- •Chapter 6. Head and neck and spine
- •Part three. Prevertebral region
- •Part eleven. Mouth and hard palate
- •Part fifteen. Lymph drainage of head and neck
- •Part twenty-two. Vertebral canal
- •Chapter 7. Central nervous system
- •Part two. Brainstem
- •Part three. Cerebellum
- •Part four. Spinal cord
- •Part five. Development of the spinal cord and brainstem nuclei
- •Chapter 8. Osteology of the skull and hyoid bone
- •Part two. Hyoid bone
- •Biographical notes
- •Index
Part twenty. Female urogenital region
The female external genitalia include the mons pubis, labia majora, labia minora, clitoris, vestibule, bulbs of the vestibule and the greater vestibular glands. Collectively they form the vulva. All the formations and structures seen in the male are present in the female, but greatly modified for functional reasons. The essential difference is the failure in the female of the midline fusion of the genital folds. The scrotum is represented by the labia majora and the corpus spongiosum by the labia minora and the bulb of the vestibule, with corresponding vessels and nerves.
The mons pubis is the mound of hairy skin and subcutaneous fat in front of the pubic symphysis and pubic bones. It extends backwards on either side as the labia majora which are fatty cutaneous folds forming the boundary of the pudendal cleft. The round ligaments of the uterus end in the anterior part of each labium. A persistent processus vaginalis, and consequently an inguinal hernia, may reach a labium. The labia are joined in front as the anterior commissure; at the back they fade away behind the vagina, the connecting skin between them forming a low ridge, the posterior commissure, which overlies the perineal body.
The labia minora are cutaneous folds without fat lying internal to the labia majora and forming the boundaries of the vestibule. Their front ends split and unite to form the (dorsal) prepuce and (ventral) frenulum of the clitoris, while at the back they unite by a small skin fold, the frenulum of the labia.
T he clitoris lies at the front ends of the labia minora. It is formed by two miniature corpora cavernosa and the anterior ends of the bulbs of the vestibule. Its free extremity, the glans, is highly sensitive to sexual stimulation and is usually overlapped by the prepuce.
The vestibule is bounded by the labia minora and contains the external urethral meatus, the vaginal orifice and the ducts of the greater vestibular glands.
The perineal membrane is wider but weaker than in the male, being pierced by the vagina. It gives attachment to the crura of the clitoris, each of which is covered by an ischiocavernosus muscle. Medial to each crus, attached to the perineal membrane at the side of the vagina, is a mass of erectile tissue, the bulb of the vestibule, one on each side of the orifices of the vagina and urethra. They join in front of the urethral orifice and pass forwards to the glans of the clitoris. Each bulb is covered by a bulbospongiosus muscle, whose fibres extend from the perineal body round the vagina and urethra to the clitoris. They form a perineal sphincter for the vagina in addition to its pelvic sphincter (the pubovaginalis parts of levator ani).
The greater vestibular glands (of Bartholin) form pea-shaped masses less than 1 cm in diameter lying at the side of the vaginal opening, one behind the posterior end of each bulb and deep to bulbospongiosus. Each opens by a single duct 2 cm long into the posterolateral part of the vaginal orifice, in the groove between the labium minus and the hymen or its remains. The duct may be subject to cyst formation, and the gland to infection (bartholinitis). The glands may play a minor role in lubricating the lower vagina. They are homologous with the bulbourethral (Cowper's) glands of the male, but unlike in the male they are superficial to the membrane.
The lesser vestibular glands are very small mucous glands with minute openings between the urethral and vaginal openings.
The hymen is a mucosal fold of variable extent and thickness at the margins of the vaginal opening. It may be absent or may even completely close the opening, in which case it must be incised at the age when menstruation begins. Its remains after rupture by the first sexual intercourse may form small tags (hymenal carunculae).
The deep perineal space is traversed by both the urethra and vagina. As in the male it contains the sphincter urethrae, deep transverse perineal muscles, nerves and vessels. The pudendal nerve and internal pudendal vessels have a corresponding course and distribution in the female deep perineal space and vulval region to that in the male deep and superficial perineal spaces, but the neurovascular branches are generally smaller. The pudendal nerve can be infiltrated with a local anaesthetic (pudendal nerve block) via a needle passed through the vaginal wall, directed towards the ischial spine and sacrospinous ligament which are palpable per vaginam.
Female orgasm
Sexual excitement induces vascular dilatation and engorgement in the vulva, especially the bulbs of the vestibule and glans clitoris, and is due, as in the male, to parasympathetic activity. There is dilatation of the thin-walled submucous veins of the vagina, which becomes moistened by a transudation of fluid through the mucous membrane. The vestibular glands probably make a negligible contribution. At the climax there is some vaginal smooth muscle and perineal skeletal muscle contraction, mediated by their sympathetic and somatic nerve supply respectively.
Part twenty-one. Pelvic joints and ligaments
The joints of the pelvis are the sacroiliac and sacrococcygeal joints and the pubic symphysis, while the chief ligaments of the pelvis (vertebropelvic ligaments) are the sacrotuberous, sacrospinous and iliolumbar.
Sacroiliac joint
The sacroiliac joint is a synovial joint between the auricular surfaces of the ilium (see Fig. 3.49, p. 167) and sacrum (see Fig. 6.98, p. 437). The articulating surfaces are jagged and there is very little movement. With increasing age fibrous adhesions and gradual obliteration of the joint cavity occur; earlier in males, after the menopause in females.
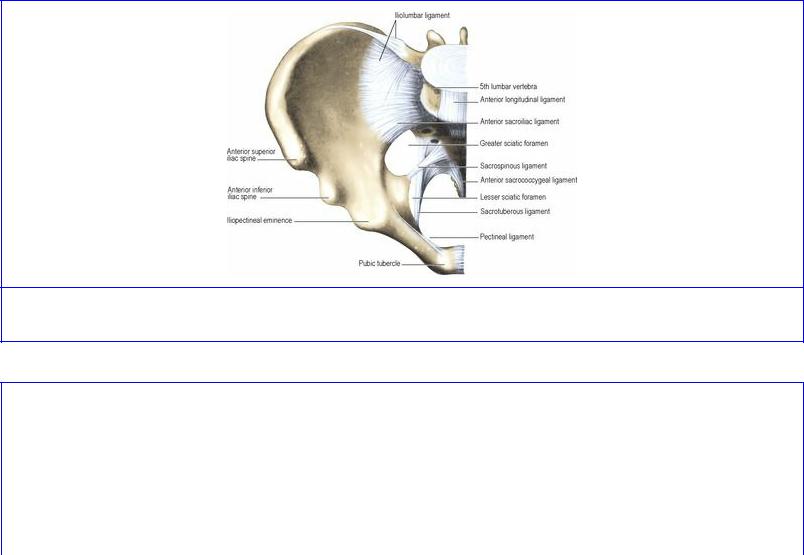
The capsule is attached to the articular margins. Ligamentous bands surround the capsule. The anterior sacroiliac ligament is a flat band which joins the bones above and below the pelvic brim (Fig. 5.73); stronger in the female, it indents a preauricular groove on the female ilium just below the pelvic brim. A mass of ligaments attaches the sacrum to the ilium behind the joint. Most of them constitute the very strong interosseous sacroiliac ligament, whose fibres are attached to deep pits on the posterior surface of the lateral mass of the sacrum. The most superficial fibres form the posterior sacroiliac ligament (Fig. 5.74). The posterior rami of the spinal nerves and vessels pass between the interosseous and posterior ligaments.
Figure 5.73 Ligaments of the right half of the pelvis: anterior aspect.
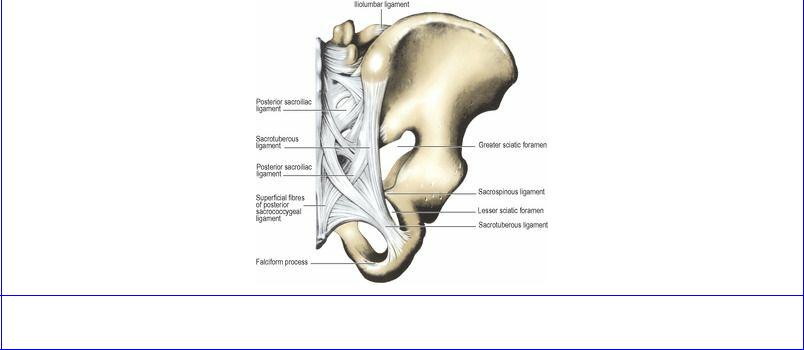
Figure 5.74 Ligaments of the right half of the pelvis: posterior aspect.
The stability of the sacroiliac articulation depends entirely upon ligaments. Body weight transmitted through L5 vertebra tends to push the sacrum downwards and forwards towards the symphysis. Opposing any gliding movement of the joint surfaces are the interosseous sacroiliac ligament and the iliolumbar ligament, while opposing forward rotation of the sacral promontory are the sacrotuberous and sacrospinous ligaments (see below). The sacroiliac ligaments soften towards the later months of pregnancy and permit some slight rotation of the sacrum during parturition.
Sacrotuberous ligament
The sacrotuberous ligament is a flat band of great strength. It is blended with the posterior sacroiliac ligament and is attached to the posterior border of the ilium and the posterior superior and posterior inferior iliac spines, to the transverse tubercles of the sacrum below the auricular surface, and to the upper part of the coccyx (Fig. 5.74). From this wide area the ligament slopes down to the medial surface of the ischial tuberosity. The lower edge of the ischial attachment is prolonged forwards and attached to a curved ridge of bone. This prolongation is the falciform process; it lies just below the pudendal canal. The sacrotuberous ligament is narrower in the middle than at either end. Its gluteal surface gives origin to gluteus maximus. The ligament is said to be the phylogenetically degenerated tendon of origin of the long head of biceps femoris. It is pierced by the perforating cutaneous nerve and branches of the inferior gluteal vessels and coccygeal nerves.
Sacrospinous ligament
The sacrospinous ligament lies on the pelvic aspect of the sacrotuberous ligament (Fig. 5.73). It has a broad base which is attached to the side of the lower part of the sacrum and the upper part of the coccyx. It narrows as it passes laterally, where its apex is attached to the spine of the ischium. The coccygeus muscle lies on the pelvic surface of the ligament. The ligament is the phylogenetically degenerated posterior surface of the coccygeus muscle.
The sacrotuberous and sacrospinous ligaments, with the lesser sciatic notch of the ischium, enclose the lesser sciatic foramen, whose lateral part is occupied by the emerging obturator internus muscle and whose medial part leads forwards into the pudendal canal above the falciform process of the
sacrotuberous ligament (Fig. 5.70).
Iliolumbar ligament
The iliolumbar ligament is shaped like a V lying sideways, the apex of the V being attached to the transverse process of L5 vertebra, from which upper and lower bands fan outwards. The upper band passes to the iliac crest, giving partial origin to quadratus lumborum and becoming continuous with the anterior layer of the lumbar fascia. The lower band runs laterally and downwards to blend with the front of the anterior sacroiliac ligament.
Sacrococcygeal joint
The sacrococcygeal joint is a symphysis between the apex of the sacrum and the base of the coccyx, with an intervening disc of fibrocartilage. A short anterior sacrococcygeal ligament unites the bones at the front. Behind, there are two posterior sacrococcygeal ligaments: a short deep one uniting the adjacent bones and a superficial which closes over the sacral hiatus at the lower end of the sacral canal. At each side there is a lateral sacrococcygeal ligament running from the transverse process of the coccyx to the inferolateral angle of the sacrum, completing a foramen for the anterior ramus of the fifth sacral nerve. This ligament may become ossified. Slight flexion and extension are possible at this joint.
Pubic symphysis
The pubic symphysis as its name implies, is a secondary cartilaginous joint. The body surfaces of the pubes are each covered with a thin plate of hyaline cartilage and the two sides are connected by fibrocartilage forming an interpubic disc. Centrally a tissue-fluid space may develop, but it is never lined with synovial membrane. Ligamentous fibres forming the superior pubic ligament reinforce the symphysis above, and below it is strengthened by the arcuate pubic ligament. No perceptible movement occurs at the symphysis; some separation of the pubes may occur during parturition.

Part twenty-two. Summary of lumbar and sacral plexuses
The two plexuses have already been described, and accounts of their branches are found in the descriptions of the appropriate regions; the branches are summarized below.
Lumbar plexus
After the anterior rami of the upper four lumbar nerves have supplied psoas and quadratus lumborum segmentally, they form the plexus in the substance of psoas major. The plexus ( Fig. 5.75) innervates part of the lower abdominal wall, but is chiefly concerned in supplying skin and muscle in the lower limb. It reinforces the sacral plexus, which is the true plexus of the lower limb.
Branches of the lumbar plexus
L1 Iliohypogastric and ilioinguinal
L1, 2 Genitofemoral
L2, 3 (posterior divisions) Lateral femoral cutaneous
L2, 3, 4 (posterior divisions) Femoral
L2, 3, 4 (anterior divisions) Obturator.
Iliohypogastric and ilioinguinal nerves (L1)
These are only by convention included in the lumbar plexus. They are really just the first lumbar segmental body–wall nerve and its collateral branch, in series with the thoracic nerves (see p. 12). Apart from supplying skin over the inguinal region and the front of the scrotum, they provide the important motor supply for the fibres of internal oblique and transversus that form the roof of the inguinal canal and reach the conjoint tendon.
Genitofemoral nerve (L1, 2)
The femoral part supplies an area of skin below the middle of the inguinal ligament. The genital part supplies that part of the abdominal wall herniated into the scrotum for the descent of the testis (i.e. the spermatic cord). It is sensory to tunica vaginalis and the spermatic fasciae, and motor to cremaster muscle. It supplies a small area of anterior scrotal and labial skin.
Lateral femoral cutaneous nerve (L2, 3—posterior divisions)
The nerve is wholly sensory, to the iliac fascia and peritoneum of the iliac fossa, and to the lateral side of the thigh down to the knee. It emerges from the lateral border of psoas and enters the thigh by passing through or under the lateral part of the inguinal ligament.
Femoral nerve (L2, 3, 4—posterior divisions)
This nerve issues from the lateral border of psoas and crosses the iliac fossa in the gutter between psoas and iliacus, deep to the iliac fascia. It supplies iliacus in the abdomen and passes beneath the inguinal ligament lateral to the femoral sheath. As it enters the femoral triangle it supplies pectineus and breaks up at once into several branches.
The nerve to pectineus runs behind the femoral sheath to reach the muscle. Of two nerves to sartorius one often pierces the muscle and continues on as an intermediate femoral cutaneous nerve
which supplies skin and fascia lata over the front of the thigh down to the knee. The medial femoral cutaneous nerve supplies the medial side of the thigh, and an anterior branch reaches the front of the knee.
The nerve to rectus femoris is usually double, and the upper branch also supplies the hip joint. The nerve to vastus lateralis runs down with the descending branch of the lateral femoral circumflex artery between rectus femoris and vastus intermedius. The nerve to vastus intermedius sinks into the anterior surface of that muscle. The nerve to vastus medialis enters the upper part of the subsartorial canal and sinks into the muscle. The nerves to all three vasti also supply the knee joint.
The saphenous nerve crosses in front of the femoral artery in the subsartorial canal, and emerges from behind the posterior border of sartorius. Its infrapatellar branch pierces sartorius to run into the patellar plexus. The saphenous nerve pierces the fascia lata between the tendons of sartorius and gracilis and descends to supply skin and periosteum over the subcutaneous surface of the tibia. It runs with the great saphenous vein in front of the medial malleolus and ends on the medial side of the foot just short of the big toe.
Obturator nerve (L2, 3, 4—anterior divisions)
Emerging from the medial side of psoas the nerve lies on the ala of the sacrum lateral to the lumbosacral trunk. It slants down to the side wall of the pelvis between the origin of the internal iliac artery and the ilium. From the angle between external and internal iliac vessels it runs straight to the obturator foramen, supplying the parietal peritoneum of the side wall of the pelvis (in the female the ovary lies here). As it emerges from the obturator foramen it splits into anterior and posterior divisions.
The posterior division supplies obturator externus, then pierces the upper part of that muscle and runs into the thigh deep to adductor brevis. It runs down on adductor magnus, whose pubic part it supplies. A slender branch accompanies the femoral artery into the popliteal fossa to supply the knee joint.
The anterior division passes over obturator externus and, emerging into the thigh, it supplies the hip joint. It runs down over adductor brevis, deep to pectineus and adductor longus. It supplies these two adductors and may supply pectineus. It also supplies gracilis. It supplies the medial side of the thigh by a cutaneous branch which runs through the subsartorial plexus.
The accessory obturator nerve, when occasionally present, passes over the superior pubic ramus to supply pectineus.
Sacral plexus
This is a flat, triangular formation on the front of piriformis muscle. It is formed out of the lumbosacral trunk (L4, 5) and the upper four anterior sacral rami (Fig. 5.76). These rami divide and unite as they converge to the greater sciatic foramen, forming the branches of the sacral plexus.
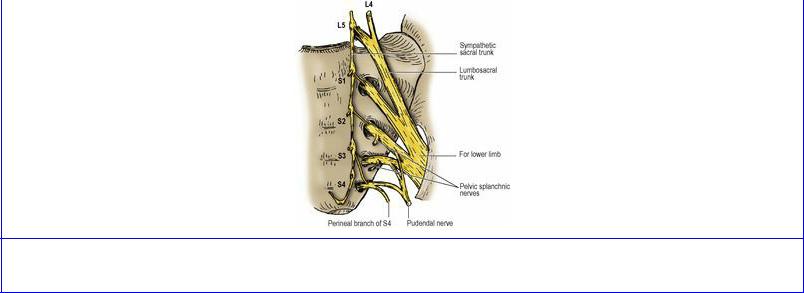
Figure 5.76 Left sacral plexus. The branches from its anterior surface (three Ps) are shown.
The nerves to piriformis (S1, 2) are twigs that pass back from the upper sacral nerves into the muscle.
The perforating cutaneous nerve (S2, 3) pierces the sacrotuberous ligament and the fibres of gluteus maximus that arise there, and supplies a small area of skin on the lower medial side of the buttock.
The posterior femoral cutaneous nerve (S1, 2, 3) has a wide distribution. It runs down below piriformis on the sciatic nerve. From the lower border of gluteus maximus it runs down the posterior midline beneath the fascia as far as the lower ends of the gastrocnemius bellies. It supplies a strip of deep fascia and skin, between anterior and posterior axial lines, from the buttock to the midcalf by a series of branches which pierce the deep fascia.
Gluteal branches wind around gluteus maximus to supply skin over the convexity of the buttock. The long perineal branch winds around the hamstrings and gracilis origins and pierces the fascia lata at the medial convexity of the upper thigh. It supplies the lateral part of the posterior two-thirds of the scrotum (labium majus).
The pelvic splanchnic nerves (S2, 3, 4) constitute the sacral parasympathetic outflow and the fibres join the inferior hypogastric plexus. They are motor to the bladder and to the large intestine from the splenic flexure downwards, and cause penile (clitoral) erection. Their afferent fibres include those for distension and pain from the bladder, lower cervix, lower colon and rectum. Referred pain may be felt in the distribution of the posterior femoral cutaneous nerve.
The pudendal nerve (S2, 3, 4) runs down and curls around the gluteal surface of the sacrospinous ligament to enter the pudendal canal. It is the nerve of the perineum.
At the posterior end of the canal it gives the inferior rectal nerve which arches through the fat of the ischioanal fossa; its branches supply the external anal sphincter, anal canal and perianal skin.
The perineal nerve emerges from the anterior end of the canal as a terminal branch of the pudendal. It runs forward and breaks up to supply skin of the posterior two-thirds of the scrotum and vulva, and the mucous membrane of the urethra and vagina. It is motor to the perineal muscles, namely, ischiocavernosus, bulbospongiosus, superficial and deep transversus perinei and the sphincter urethrae.
The dorsal nerve of the penis (clitoris) is the other terminal branch of the pudendal. It runs forward deep to the perineal membrane, which it pierces just below the symphysis pubis to supply the skin of the penis (clitoris).
Muscular branches of S3 and S4 supply levator ani and coccygeus on their upper (pelvic) surfaces.
The perineal branch of S4 passes between levator ani and coccygeus to supply the puborectalis, pubourethralis and pubovaginalis parts of levator ani from below, and the skin over the ischioanal fossa.
The nerve to quadratus femoris (L4, 5, S1) lies on the ischium deep to the sciatic nerve and runs down deep to obturator internus to sink into the deep surface of quadratus femoris. It also supplies the inferior gemellus and gives a branch to the hip joint.
The nerve to obturator internus (L5, S1, 2) passes below piriformis, curls around the base of the ischial spine and sinks into obturator internus. It also supplies the superior gemellus.
T he superior gluteal nerve (L4, 5, S1) passes back through the greater sciatic notch above piriformis, runs in the plane between glutei medius and minimus, supplies both, and ends in the tensor fasciae latae.
The inferior gluteal nerve (L5, S1, 2) passes back below piriformis and sinks into the deep surface of gluteus maximus.
Sciatic nerve
The sciatic nerve is the largest branch of the sacral plexus from which it is formed at the lower margin of piriformis by union of its tibial and common peroneal parts. It passes into the buttock lying on the posterior surface of the ischium. Here the nerve to quadratus femoris is deep to it and the posterior femoral cutaneous nerve lies superficial. From midway between the greater trochanter and the ischial tuberosity, the sciatic nerve passes vertically downwards into the hamstring compartment. It lies on obturator internus and gemelli, quadratus femoris and then on adductor magnus. It is overlaid by the long head of biceps. The main trunk of the sciatic nerve supplies all the hamstrings and the ischial fibres of adductor magnus and it then divides, usually at the upper angle of the popliteal fossa, into the tibial and common peroneal nerves. The branches for the long head of biceps, the two ‘semi-’ muscles and adductor magnus are from the tibial part, but the branch to the short head of biceps comes from the common peroneal part.
Common peroneal (fibular) nerve (L4, 5, S1, 2)
The common peroneal nerve supplies the extensor and peroneal compartments of the leg and the dorsum of the foot. It enters the apex of the popliteal fossa and runs medial to the biceps tendon just beneath the deep fascia. It crosses plantaris, lateral head of gastrocnemius and curves around the neck of the fibula, through peroneus longus, where it divides into two terminal branches, the deep and superficial peroneal (fibular) nerves. It can be palpated on the neck of the fibula, where it can be rolled on the bone. It is the nerve most commonly injured in the lower limb.
The common peroneal nerve itself supplies no muscles. Three articular branches, the upper and lower lateral and recurrent genicular nerves, supply the knee joint; the lateral genicular nerves accompany
the arteries, the recurrent supplies the superior tibiofibular joint as well.
There are two cutaneous branches. The sural communicating nerve joins the sural nerve below the gastrocnemius heads. The lateral cutaneous nerve of the calf supplies skin and deep fascia over the upper half of the peroneal compartment.
The deep peroneal nerve is formed in the substance of peroneus longus, spirals down over the fibula deep to extensor digitorum longus and reaches the interosseous membrane. It runs down lateral to the vessels, crosses the lower end of the tibia and the dorsum of the foot, and ends by supplying the skin of the first interdigital cleft.
It supplies the muscles of the extensor compartment of the leg: extensor digitorum longus, tibialis anterior, extensor hallucis longus and peroneus tertius. On the dorsum of the foot it gives a lateral branch which supplies extensor digitorum brevis.
The superficial peroneal nerve is formed in the substance of peroneus longus and runs down in the muscle, emerging from its anterior border about a third of the way down the leg. It supplies peroneus longus and brevis, then perforates the fascia to supply the skin over the peronei and extensor muscles in the lower third of the leg. Above the ankle it divides into a medial and a lateral branch which supply skin and deep fascia on the dorsum of the foot. The medial branch breaks up to supply the medial side of the big toe and the second interdigital cleft, while the lateral branch breaks up to supply the third and fourth clefts.
Tibial nerve (L4, 5, S1, 2, 3)
The tibial nerve supplies the calf and the sole of the foot around to the toenails. The nerve enters the apex of the popliteal fossa and, in the midline of the limb, passes vertically down deep to the heads of gastrocnemius behind the knee joint and across the popliteus muscle, to run beneath the fibrous arch in soleus.
Branches in the popliteal fossa. Three genicular nerves, upper and lower medial and a middle, accompany the arteries and supply the knee joint. Five muscular branches supply the muscles of the fossa: plantaris, both heads of gastrocnemius, soleus and popliteus. The last-named branch recurves around the lower border of the muscle to enter its deep (anterior) surface. A single cutaneous branch, the sural nerve, lies in the groove between the two heads of gastrocnemius and pierces the deep fascia halfway down the leg. Here it is joined by the sural communicating nerve. The sural nerve runs down alongside the small saphenous vein behind the lateral malleolus and ends on the lateral side of the little toe.
From the fibrous arch the nerve runs down with the posterior tibial vessels deep to the soleus muscle. The neurovascular bundle lies in the groove between the bellies of flexor hallucis longus and flexor digitorum longus. Behind the medial malleolus, beneath the flexor retinaculum, the nerve divides into its terminal medial and lateral plantar branches.
Branches in the calf. Four muscular branches supply soleus, tibialis posterior and the flexors hallucis and digitorum longus. Medial calcanean branches pierce the flexor retinaculum and supply the weight-bearing skin of the heel.
The medial and lateral plantar nerves correspond approximately to the median and ulnar nerves in the hand as far as skin and muscle supplies are concerned. The medial plantar supplies the medial part of the sole and plantar surface of the medial three and a half digits, and innervates flexor digitorum brevis, abductor hallucis, flexor hallucis brevis and the first lumbrical, with the lateral plantar supplying the rest of the sole and the other small muscles of the foot.
