
Pediatrics(2)
.pdf-- Gallop rhythm
-- Hepatomegaly
-- Crackles/wheezes
-- Weak and fast pulses (or absent)
-- Cold extremities/ palor
-- Capillary refill > 2 seconds
-- Oliguria/anuria
-Management
-Non pharmacological management
-• Avoid excessive IV fluids, the patient is fluid overloaded in this case, give 2/3 of maintenance (aim at urine output of 2ml/kg/h)
-•Oxygen therapy: 10-15l/min with mask and reservoir bag
-• SemiSitting position (cardiac bed)
-• Low sodium diet
-• Strict bed rest
-• Ensure adequate nutrition
-• Correct hypoglycemia with 3-5ml/kg IV of Dextrose 10%
-Pharmaceutical treatment
-• Dopamine IV 5-10 microgram/kg/min, may increase to 20 microgram/kg/min Or
-• Dobutamine IV 2 to 20 microgram/kg/min •Furosemide IV 2mg/kg/dose if adequate
peripheral perfusion. Repeat the dose according to estimated fluid
overload up to 8mg/kg/day

-• Correct arrhythmia if present with Digoxin 0.04mg/kg/day in 3 divided doses ( maintenance0.01mg/kg/day)
-• Monitor: Heart rate, Respiratory rate, BP, Urine output, Pulse Oxymetry for oxygen saturation
-3.3. Pulmonary Oedema
-  - Kerley B lines represent thickened
- Kerley B lines represent thickened
connective tissue planes, for example due to edema of the septal lines of secondary lobules. They are most commonly due to pulmonary edema or lymphangitic carcinomatosis. Kerley B lines are horizontal, < 2 cm long and 1 mm thick, at periphery of lung and reaching the lung edge.
-Definition: Pulmonary oedema is the accumulation of fluid in the
-alveoli due to an increase in pulmonary capillary venous pressure resulting from acute left ventricular failure.
-Causes
-- Heart not removing fluid from lung circulation properly (cardiogenic pulmonary edema)
-- A direct injury to the lung parenchyma
-Signs and Symptoms
-- Breathlessness/ respiratory distress
-- Sweating
-- Cyanosis (decreased oxygen saturation)
-- Frothy blood-tinged sputum
-- Ronchi, and crepitations/wheezers
-Investigations
-- Chest x-ray shows loss of distinct vascular margins, Kerley B lines, diffuse haziness of lung fields, pleural effusion
-- Blood Gas if possible
-- ECG
-- Echocardiography
-Management
-- Maintain patient in a semi sitting position
-- Oxygen by facial mask with reservoir bag if available
-- IV Furosemide 2mg/kg/dose, maximum 8mg/kg/day
-- Inotropic support with Dopamine or Dobutamine if signs of shock
-- Transfer to cardiologist for further management
-3.4. Congenital Heart Diseases
-Definition: Congenital heart disease refers to a problem with the heart’s structure and function due to abnormal heart developmentbefore birth. Often divided into two types, non-cyanotic and cyanotic(blue discoloration caused by a relative lack of oxygen).
General principles of management
•Initial stabilization: secure airway, adequate ventilation, circulatory support
•Correct metabolic acidosis, electrolyte derangements, hypoglycaemia;
prevent hypothermia.
•Empirical treatment with IV antibiotics.
•Early cardiology consultation.
•IV Prostaglandin E infusion if duct-dependent lesions suspected:
•2tar3ng dose: +C – 4C ng/kg/min; maintenance: 2 – +C ng/kg/min.
•Adverse effects: apnoea, fever, hypotension.
•If unresponsive to IV prostaglandin E, consider:
•Transposition of great arteries, obstructed total anomalous pulmonary.
venous drainage.
•Blocked IV line.
•Non-cardiac diagnosis.
-• Arrangement to transfer to regional cardiac center once stabilized.
-3.4.1. Non Cyanotic Heart Diseases

-
-
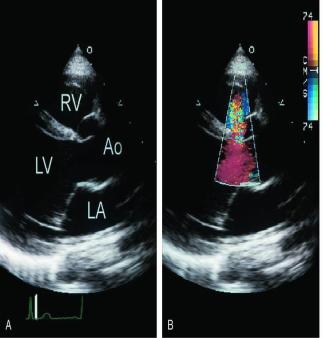
-Small ventricular septal defects may not be apparent on two-dimensional imaging (A), but their presence can be confirmed using color Doppler imaging (B). In this example, the septum appears intact, but medial angulation and the use of color Doppler imaging confirm the presence of a small defect. Ao, aorta; LA, left atrium; LV, left ventricle; RV, right ventricle.
-Common lesions
-
-
-
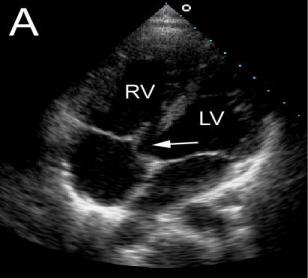
-A trabecular ventricular septal defect (arrow) is shown. The presence of the defect is suggested on two-dimensional imaging
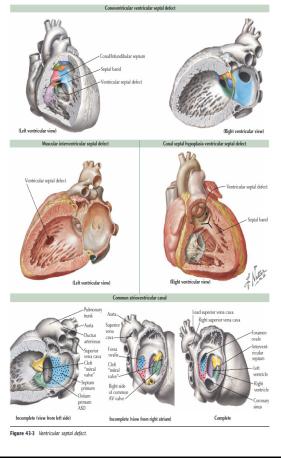
-- Ventricular Septal defect (VSD) most common congenital heart disease
-- Patent ductus arteriosus (PDA)
-- Atrio-ventricular septal defect (AVSD) or endocardial cushion defect (common in trisomy 21)
-Atrial septal defect (rarely causes heart failure)
-Coarctation of aorta
-Signs and Symptoms
-- Tachypnea, dyspnea
-- Tachycardia
-- Sweating
-- Feeding difficulties / failure to thrive
-- Recurrent chest symptoms
-- Hepatomegaly
-- Increased jugular venous pressure
-Complications
-- Failure to thrive
-- Infective Endocarditis
-Pulmonary vascular obstructive disease (pulmonary hypertension) which can lead to Eisenmenger syndrome
-Investigations
-- Chest X-Ray
-- ECG
-- Echocardiogram
-- Cardiac catheterization/angioscan in special cases
-Management
-Treatment depends on the specific condition. Some congenital heart diseases can be treated with medication alone, while others require one or more surgeries.
-- Lasix 2mg/kg/day
- - captopril 1-3mg/kg/day (start with 1mg/kg)
-- Increase calories in feeding
-- Iron if Hb less than 10g/dl (preferably reach 15g/dl)
