
Pediatrics(2)
.pdf


Dr: Essam Abdullah 01123232188
- 5. Endocrine System Conditions
-5.1. Diabetes Mellitus (Type I and Type II)
-Definition: diabetes mellitus is a disorder of absolute or relative insulin deficiency that results in increased blood glucose and disruption of energy storage and metabolism. diabetes Mellitus is generally divided into two classifications: diabetes Mellitus I and diabetes Mellitus Type II.
-- diabetes Mellitus Type I: This results from the destruction of the pancreatic beta cells that leads to absolute insulin deficiency.
-Type IA is secondary to the autoimmune destruction of the beta cells. Type IB is secondary to non-autoimmune destruction of the beta cells. Type I diabetes accounts for approximately 2/3 of the new diagnosis of diabetes in patients < 19 years old. There is a component of genetic susceptibility and close relatives of patients with type I dM are at higher risk of developing the disease.
-- diabetes Mellitus Type II: This is secondary to varying degrees of insulin resistance and insulin deficiency and is related to both genetic and environmental influences including predisposing medication such as steroids and some ARVs. It is the most common type of diabetes mellitus in adults.
-- Neonatal diabetes: This is defined as persistent hyperglycemia occurring in the first months of life that lasts more than 2 weeks and requires insulin therapy for management. It is a rare cause of hyperglycemia in the neonate and has an estimated incidence of 1/500,000 births. The majority of affected infants are small for
-gestational age and present with weight loss, volume depletions, hyperglycemia and glucosuria with or without ketonuria and ketoacidosis.
-Signs and Symptoms
-- Polyuria: This occurs when the serum glucose concentration rises above 180 mg/dL exceeding the renal threshold for glucose and leads to increased urinary glucose excretion and a subsequent
-osmotic diuresis. This may present as nocturia, bedwetting, or daytime incontinence in a previously toilet trained child, or heavy diapers.
-- Polydipsia: This is secondary to increased thirst from increased serum osmolality and dehydration.
-- Polyphagia: This is due to an increased appetite that’s initially secondary to loss of calories from glycosuria. These symptoms are not always present.
-- Weight loss: This is due to hypovolemia and increased catabolism.
-- Weakness/Lethargy with ultimate progression to coma: This is secondary to hypovolemia and electrolyte disturbances including progressive acidosis.
-Visual disturbances: This is secondary to osmotic changes in the lens.
-Complications
-- Short-term complications:
-• diabetic ketoacidosis (dKA): Occurs more frequently in type I diabetes mellitus, but may also occur in some forms of type I diabetes mellitus.
-• Hyperosmolar hyperglycaemic state (HHS): Occurs in type II diabetes mellitus.
-• Insulin resistance secondary to hyperglycemia: This occurs in both type I and type II diabetes mellitus.
-• Infections due to immunosuppression commonly include oral and vaginal candidiasis and Urinary Tract Infections.
-• death: Patients presenting with dKA or HHS have a high mortality rate.
-- Long Term complications:
-• Vascular complications including both micro-angiopathy and macro-angioapthy:
-→Nephropathy
-→ Retinopathy
-→ Neuropathy
-→ Cardiovascular disease
-→ Hypertension
- • dyslipidemia
-• Growth retardation or obesity depending on the insulin therapy. Patients may also have delayed puberty secondary to poor growth.
-• Psychiatric disorders including depression related to their chronic disease.
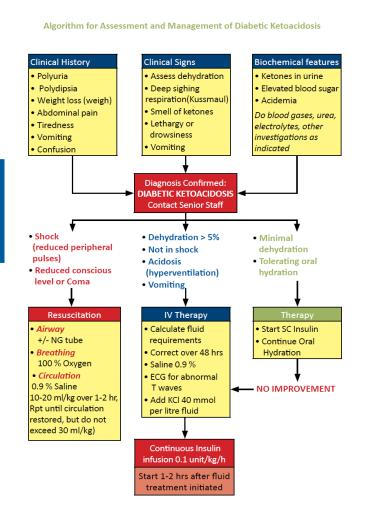
-Investigations
-- Blood sugar: The diagnosis is made based on abnormalities of the blood glucose. See diagnostic criteria below.
-- Additional studies to evaluate severity and complications of the disease:
-• Blood gas if concern for diabetic ketoacidosis.
-• Electrolytes
-• Renal function tests (urea and creatinine) to evaluate for diabetic nephropathy and dehydration.
-• Urine analysis to check for glycosuria, ketones, and protein
-• HbA1c: This can be used for diagnosis (see below) or to assess severity of disease and to assess response to therapy.
-• Lipid profile
-• Fundoscopy: This is to evaluate for diabetic retinopathy.
-• Foot examination: This is to evaluate for diabetic neuropathy and assess for wounds that may already be present.
-• Further history and physical examination to exclude other coexisting autoimmune diseases such as hypothyroidism,
-vitiligo, rheumatoid arthritis, etc., and to further ask about family history of endocrinopathies or autoimmune diseases.
-• Thyroid-stimulating hormone (TSH): This should be performed in type I diabetics as autoimmune diseases may occur together.
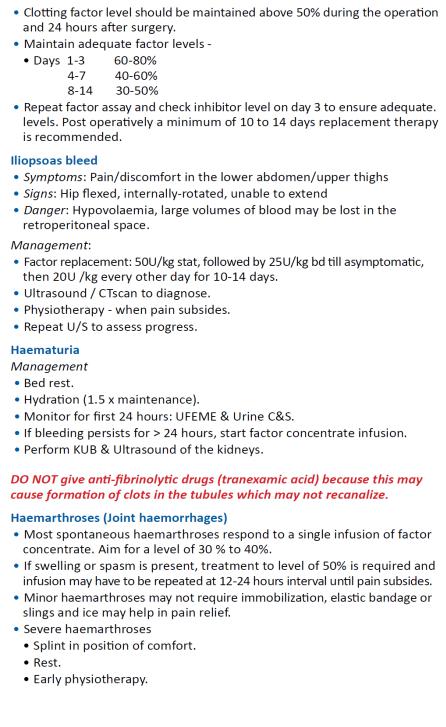
-Diagnosis criteria for diabetes mellitus
-
-Management
-General Objectives
-• Maintain normal glycemia with insulin therapy or oral medications (in type II diabetes mellitus) to prevent both the signs and symptoms of uncontrolled hyperglycemia and the complications mentioned above.
-Non-Pharmaceutical Management
-• Assess A-B-C-d (Airway, Breathing, Circulation, drug)
-• If patient has signs or symptoms of diabetic ketoacidosis (dKA) or hyperosmolar hyperglycaemic state, this is an emergency and treatment must be initiated immediately
-• The patient and the family should be counselled on the cause and treatment of diabetes and its management. The patient and the family should be taught how to monitor blood glucose, record the
test results, administer and adjust insulin doses based on blood glucose values and food intake.
-• They family should be counselled on the complications of diabetes mellitus and how to manage them. In particular, they should know the signs and symptoms of acute hypoglycemia and its management. They should also understand the importance of maintaining normoglycemia to avoid long-term complications. They should be instructed on how to manage acute illnesses in the context of diabetes mellitus, for example how to manage an insulin
-dose if the the patient is unable to tolerate oral intake.
-• diet modification is important in both type I and type II
-diabetes mellitus. A nutritionist should be involved in providing individualized recommendations.
-Pharmaceutical management
-• The majority of children with diabetes mellitus have type I diabetes and may present with diabetic ketoacidosis
-(dKA). The management of dKA is detailed below.
-→ diabetes Mellitus Type I: Children with diabetes Mellitus Type I require insulin therapy. The patient is
-insulin dependent and while the insulin therapy may be adjusted based on the clinical condition and blood
-glucose results; the insulin therapy should NEVER be stopped completely as this could result in the
-development of dKA and death.
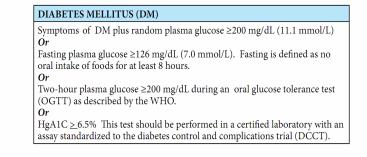
-5.2. Diabetic Ketoacidosis
-
-

-
