
Pediatrics(2)
.pdf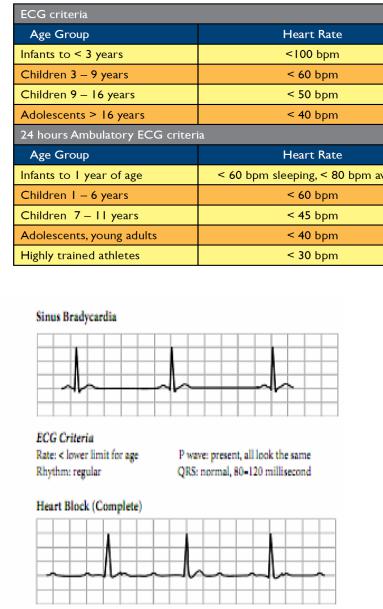
-Causes
-- Hypoxia
-- Hypothermia
-- Head injuries and increased intracranial pressure
-- Toxins and drug overdose
-- Post operative
-- Congenital excessive vagal stimulation
-- Electrolyte disturbances (Hypoor hyperkalaemia, Hypocalcaemia)
-Sinus Bradycardia
-ECG Criteria
-Rate: low, usually < 60 beats per minute P wave: independent P waves QRS’s with no relationship between the two (AV dissociation)
-Management
-- If syncope and Heart rate - below 50/min
-• Start i.v. Isuprel (Isoprenaline) 0. 05 – 0. 4 microgram/kg/min.
- |
Or |
-• Dobutamine (Dobutrex) 2 - 20 microgram/kg/min
-• Insert pacemaker if ineffective
Dr: Essam Abdullah 01123232188
- 4. Haematological Conditions
-4.1. Anemia
-Definition: Anemia is defined as a reduction of the red blood cell
-(RBC) volume or hemoglobin concentration below the range of normal
-values occurring in healthy persons.
-Cause
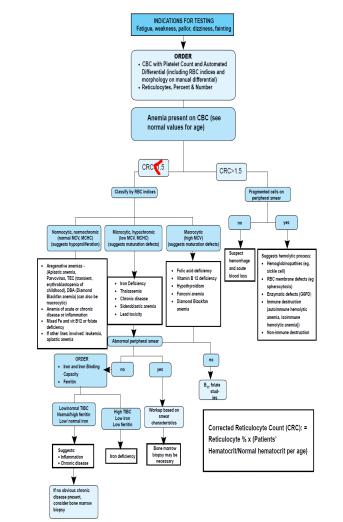
-- Anemia is classified according to physiologic process (decreased production, increased destruction or blood loss). In practice, classifying anemia according MCV is a useful approach to assess the common causes of anemia in children.
-Signs and Symptoms
-- Pale mucous membranes, palms and nail beds
-- dizziness, fainting
-- Headache
-- Shortness of breath on exertion (exercise intolerance)
-- Palpitations
-- Visual disturbances
-- Poor growth
-- Confusion, decreased mental activity
-- Rapid heartbeat or palpitations
-- dyspnoea, tachypnea
-- Signs of cardiac failure if severe anemia

-
-Normal values vary by age, sex and ethnicity. Means and ranges for hemoglobin and hematocrit values by age groups of wellnourished children
-Reticulocytes
are circulating immature RBC. Normal range are in the table above. However, if a person has anemia and his bone marrow is able to produce new blood cells, his/her reticulocyte percentage should be higher than
“normal” Thus, calculating the corrected reticulocyte count is an important step in understanding whether the reticulocyte count is appropriate or inappropriate to the situation.
-Corrected Reticulocyte Count (CRC): = Reticulocyte % x (Patients’ Hematocrit/Normal hematocrit per age)
-- A CRC >1.5 suggests increased Red Blood Cells production as a result of hemolysis and blood loss.
-
-Physiologic classification of Anemia
-- Anemia due to reduced red blood cell/hemoglobin production
-• Bone marrow aplasia:
-→ Fanconi’s anemia (congenital aplastic anemia)
-→ Acquired aplastic anemia, diamondBlackfan
-anemia, Transient Erythroblastopenia of
childhood (red blood cell aplasia).
-• Bone marrow replacement by tumour cells - leukaemias,
-secondary metastases.
-• Bone marrow replacement by fibrous tissue or granulomas
-- granulomas can occur in the congenital toxoplasmosis, other, rubella, cytomegalovirus, herpes simplex (TORCH),
-infections (or in tuberculosis infection. Parvovirus is directly cytotoxic because it replicates in the erythroid precursors
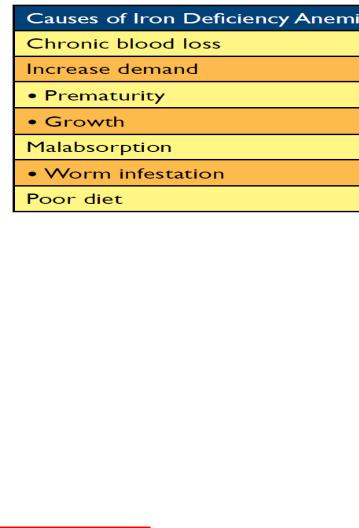
-• deficiency of iron
-
-• deficiency of folic acid: Megaloblastic anemia of infancy can develop due to:
-→ Folic acid deficiency during rapid growth.
-→ Malabsorption syndromes such as coeliac disease, in inflammatory bowel disease and in children taking anticonvulsants.
-• deficiency of vitamin B12 can occur in:
-→ Infants who are breast-fed by a vegetarian mother
-→ Mal-absorption
-→ Worm infestation
-→ Congenital pernicious anemia where there is inability to secrete gastric intrinsic factor
-• Thalassaemias:
Introduction
• β-Thalassaemia major is an inherited blood disorder presenting with anaemia at 4 - 6 months of age.
•Common presenting symptoms are pallor, lethargy, failure to thrive and hepatosplenomegaly.
•In Malaysia, the β-thalassaemia carrier rate is es'mated at (-5%, most of whom are unaware of their carrier / thalassaemia minor status.
•The carrier rates of α-thalassaemia and Haemoglobin E (HbE) are 1.8-7.5% and 5-46% respec'vely. HbE are found more in the northern peninsular states.
•Interaction between a β-thalassaemia carrier with a HbE carrier may result in the birth of a patient with HbE/β-thalassaemia or thalassaemia intermedia with variable clinical severity.
•The moderate to severe forms behave like β- thalassaemia major patients while the milder forms are asymptomatic.
Baseline investigations to be done for all new patients: -
•Full blood count, Peripheral blood film (In typical cases, the Hb is about 7g/dl)
•Haemoglobin analysis by electrophoresis / HPLC:
•Typical findings for β-thalassaemia major: HbA decreased or absent, HbF increased, HbA2 variable.
•Serum ferritin.
•Red cell phenotyping (ideal) before first transfusion.
•DNA analysis (ideal)
•For the detection of α-carrier and confirmation of difficult cases.
•Mandatory in prenatal diagnosis.
•Liver function test.
•Infection screen: HIV, Hepatitis B & C, VDRL screen (before first transfusion).
•HLA typing (for all patient with unaffected siblings)
•All nuclear family members must be investigated by Hb Analysis for genetic counselling.
-• 1st degree and 2nd degree rela'ves should
also be encouraged to be screened & counselled (cascade screening).
Management
Regular maintenance blood transfusion and iron chelation therapy is the mainstay of treatment in patients with transfusion dependent thalassaemia.
. Maintenance Blood Transfusion
Beta thalassaemia major
•When to start blood transfusion?
•After completing blood investigations for confirmation of diagnosis.
•Hb < 7g/dl on 2 occasions > 2 weeks apart (in absence other factors e.g. infection).
•Hb > 7g/dl in β+-thalassaemia major/severe forms of HbE-β-thalassaemia if impaired growth, para-spinal masses, severe bone changes, enlarging
liver and spleen.
•Transfusion targets?
