
Pediatrics(2)
.pdfPharmacological Management according to age
• Neonates
→ cimetidine IV 5-20mg/kg divided in 2 doses OR
Ranitidine IV 2mg/kg/24 divided in 2-3 doses for 10 days
Or
→ Omeprazole, PO 0.5–1 mg/kg, 12– 24 hourly for 10 days
•
→Octreotide, IV bolus, 1–2 mcg then 1–5 mcg/kg/hour by infusion, initiated by the specialist in case of cases of variceal bleeding (difficult to control, to help control bleeding before endoscopy, or when endoscopy is unsuccessful, contraindicated, or unavailable)
→Omeprazole, PO
■1 month–2 years: 2.5mg, 12 hourly
■2–6 years 5 mg, 12 hourly initiated by the specialist for post bleed prophylactic
management
• Older children and adolescents → Omeprazole, PO
■< 20 kg: 10 mg Qd
■>20 kg: 20 mg Qd
Note: Endoscopy is recommended to be
performed within 24 to 48hours for infants and
children presenting with UGI bleeding
that is acute and severe, it can be performed
for diagnosis andtreatment (sclerotherapy in
oesophageal variceal)
Alternative treatment
•Propranolol oral, 2–8 mg/kg/24 hours in 3 divided doses (to reduce the pulse rate by 25%)
•Surgical over sewing if endoscopy and sclerotherapy or banding have failed
Recommendations
- Refer all cases to the specialist for appropriate diagnosis and treatment
- Refer all bleeding varices - after commencement of resuscitation and octreotide, if available
2.7. Peptic Ulcer Disease
Definition: This refers to ulceration of gastric or duodenal mucosa that tends to be chronic and/or recurrent.
Cause
- Helicobacter pylori (H. pylori) - in developing nations, the
majority of children are infected with H. pylori before the age of 10 and adult prevalence peaks at more than 80 percent before age 50
Signs and Symptoms
- Peptic ulcers may be present with dyspeptic or other gastrointestinal symptoms or may be completely asymptomatic,
sometimes until complications such as hemorrhage or perforation occur. The symptoms associated with peptic ulcers are not sensitive or specific and the differential diagnosis is broad.
-Most common: Ulcer-like or acid dyspepsia (burning pain; epigastric hunger-like pain; relief with food, antacids, and/or anti secretory agents). - Food-provoked dyspepsia or indigestion (postprandial epigastric discomfort and fullness, belching, early satiety, nausea, and occasional vomiting): food-stimulated acid secretion persists for three to five hours; thus, classic dU symptoms occur two to five hours after meals.
-Reflux-like dyspepsia
Complications
-The natural history of peptic ulcer ranges from resolution without intervention to development of complications: acute or Chronic blood loss or perforation
-Iron deficiency anaemia
Investigations
-Stool analysis for occult blood
-FBC
-For HP:
• It is recommended that the initial diagnosis of H. pylori infection be based on positive histopathology plus positive
rapid urease test, or positive culture.
•A validated ELISA for detection of H. pylori antigen in stool is a reliable non-invasive test to determine whether H.
pylorus has been eradicated.
•Tests based on the detection of antibodies (IgG, IgA) against H. pylori in serum, whole blood, urine and saliva are not reliable for use in the clinical setting.
Management
-Avoid any foods that cause pain to the patient (e.g. acid foods, soda drinks)
-Avoid gastric irritating drugs (NSAIds)
-Give magnesium-based antacids or combined magnesium-
AluminiumFirst line H pylori eradication regimens are:
• Triple therapy with:
→ PPI + Amoxicillin + Imidazole Or
→ PPI + Amoxicillin + clarithromycin Or
→ Bismuth salts + Amoxicillin + Imidazole Or
• Sequential Therapy Triple therapy for eradication of H. pylori (duration: 10 – 14 days)
→ Omeprazole PO
■15-30 kg: 10 mg twice daily
■>30 kg: 20 mg twice daily Or
→cimetidine 20–40mg/kg/day + clarithromycin : 500mg BId + Amoxicillin 1g twice daily
Or
→cimetidine 20–40mg/kg/day +Clarithromycin : 500mg + Metronidazole 500 mg (15–20mg/kg/day ) twice daily
Recommendations
-Refer to a specialist, if there is severe hemorrhage
-Stabilize the patient before transfer
-Infuse IV fluids/blood to maintain normal volume/pulse
-Ensure continuous assessment of further blood loss (Persistent tachycardia, postural hypotension, continuing haematemesis)
-definitive treatment / eradication of H. pylori
-2.8. Gastroesophageal Reflux
-
-
-
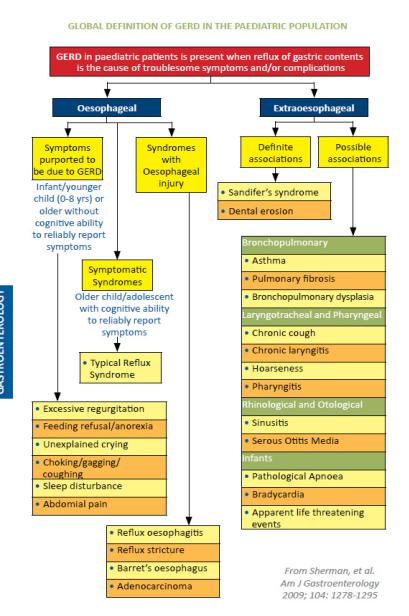
-Definition: GER is the passage of gastric contents into the esophagus with or without regurgitation and vomiting. GER is a normal physiologic process occurring several times per day in healthy infants, children, and adults.
-Most episodes of GER in healthy individuals last <3 minutes, occur in the postprandial period, and cause few or no symptoms. In contrast, Gastroesophagial reflux disease GERd is present when the reflux of gastric contents causes troublesome symptoms and/or complications.
-Causes and risk factors
-- The cause is still unclear
-- Anatomical abnormalities such as a hiatal hernia
-- Long term use of nasal gastric tube
-- diet that stimulates gastric acid production
-- Neurologic impairment (NI), obesity, certain genetic syndromes,
-esophageal atresia (EA), chronic lung diseases, and those with a history of premature birth
-Signs and Symptoms
-In infants and toddlers, there is no symptom or symptom complex that is diagnostic of GERd or predicts response to therapy. In older children and adolescents, as in adult patients, history and physical examination
-may be sufficient to diagnose GERd if the symptoms are typical. The following is suggestive:
-- In newborn: Recurrent vomiting, stridor, apnea
-- In infant: Recurrent vomiting, respiratory manifestations, (dry cough, recurrent wheeze or cough, chronic obstructive airway disease) recurrent aspiration pneumonia, stridor, apnea
In children /adolescent: Heartburn, epigastria or chest pain.
-Respiratory manifestations: (dry cough, recurrent wheeze or cough, chronic obstructive airway disease
-Complications
-- dysphagia
-- Odynophagia
-- Weight loss
-- Anemia
-- Esophagitis
-- Aspiration pneumonia
-- Barrett’s esophagus
-- Abnormal posturing or opisthotonus (Sandifer Syndrome)
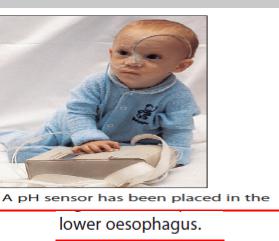
-Investigations (when GER is persisting despite basic management)
-- 24 hours esophageal PH monitoring
-- Endoscopy with biopsy to rule out oesophagitis
-- Barium X-rays for severity of oesophagus stenosis
-- FBC look for anemia
-Management
-Non-pharmacological
-• Postural treatment: Prone and lateral positions are associated with an increased incidence of sudden infant
-death syndrome (SIdS). The risk of SIdS outweighs the benefit of prone or lateral sleep
position on GER; therefore, in most infants from birth to 12 months of age, supine positioning during sleep is recommended.
-• dietary measures such as thickened food if not breastfeeding, frequent small volume of solid foods
-Pharmacological
-• Less Severe or Non Erosive
-→ Anti-acids:
-■ Sodium alginate (Gaviscon Enfant) /antacid
-combination, oral, month 1ml after each meal
-o 1-2 months 1.5 mls after each meal
-o 2-4 months 2mls after each meal
-→ Aluminium and Magnesium hydroxide (Maalox)
-Syrup 0.5 ml/kg/dose PO QId
-→ H2 Antagonists:
-■ cimetidine IV/syrup/tab
-o Neonates: 5-20mg/kg/24 hr divided in 2 doses
-o Infants: 10-20 mg/kg/24hrs divided in 2 doses
-o Children: 20-40mg/kg/24hr divided in 2 doses
-•Severe or Erosive
-→ Omeprazole, oral
-■ Neonate 0.5–1 mg/kg, 12– 24 hourly
-■ Children 1- 16 years
