
- •Table of Contents
- •Front matter
- •Copyright
- •Preface to the twelfth edition
- •Preface to the eleventh edition
- •Preface to the tenth edition
- •Acknowledgements
- •Chapter 1. Introduction to regional anatomy
- •2. Upper limb
- •Part two. Shoulder
- •Part three. Axilla
- •Part four. Breast
- •Part five. Anterior compartment of the arm
- •Part six. Posterior compartment of the arm
- •Part eight. Posterior compartment of the forearm
- •Part nine. Wrist and hand
- •Part ten. Summary of upper limb innervation
- •Part eleven. Summary of upper limb nerve injuries
- •Part twelve. Osteology of the upper limb
- •Chapter 3. Lower limb
- •Part two. Medial compartment of the thigh
- •Part three. Gluteal region and hip joint
- •Part four. Posterior compartment of the thigh
- •Part five. Popliteal fossa and knee joint
- •Part six. Anterior compartment of the leg
- •Part seven. Dorsum of the foot
- •Part eight. Lateral compartment of the leg
- •Part nine. Posterior compartment of the leg
- •Part ten. Sole of the foot
- •Part eleven. Ankle and foot joints
- •Part twelve. Summary of lower limb innervation
- •Part thirteen. Summary of lower limb nerve injuries
- •Part fourteen. Osteology of the lower limb
- •Chapter 4. Thorax
- •Part one. Body wall
- •Part three. Thoracic cavity
- •Part five. Anterior mediastinum
- •Part eight. Pleura
- •Chapter 5. Abdomen
- •Part two. Abdominal cavity
- •Part nine. Spleen
- •Part eleven. Kidneys, ureters and suprarenal glands
- •Part twenty. Female urogenital region
- •Chapter 6. Head and neck and spine
- •Part three. Prevertebral region
- •Part eleven. Mouth and hard palate
- •Part fifteen. Lymph drainage of head and neck
- •Part twenty-two. Vertebral canal
- •Chapter 7. Central nervous system
- •Part two. Brainstem
- •Part three. Cerebellum
- •Part four. Spinal cord
- •Part five. Development of the spinal cord and brainstem nuclei
- •Chapter 8. Osteology of the skull and hyoid bone
- •Part two. Hyoid bone
- •Biographical notes
- •Index
Part eight. Pleura
The pleura is a thin membrane of fibrous tissue surfaced by a single layer of flat cells (mesothelium). It clothes each lung and lines the thoracic cavity.
The parietal layer of the pleura lines the thoracic wall (rib cage, vertebrae and diaphragm), from which it is separated by loose areolar tissue, the endothoracic fascia. But the parietal pleura is attached to the inferior surface of the suprapleural membrane, at the thoracic inlet, and to the mediastinal surface of the fibrous pericardium. The pleura is one continuous sheet. From its mediastinal layer a cuff of membrane is projected around the lung root and passes on to invest the surface of the lung. This is the visceral layer of the pleura; it extends into the depths of the interlobar clefts and is adherent to the lung surface. The pleural cavity is a completely closed space. The visceral pleura on the lung surface is in contact with parietal pleura, the surfaces being lubricated by a thin film of tissue fluid. The parietal pleura, however, extends further than the inferior lung edge, to allow space for lung expansion. In these situations the costal parietal pleura is against the diaphragmatic parietal pleura, separated by a narrow space, the costodiaphragmatic recess.
The cuff of pleura projected around the lung root is too big for it and it hangs down below as an empty fold, the pulmonary ligament, in the manner of a coat cuff at the wrist. It provides ‘dead space’ into which the lung root descends with descent of the diaphragm, and allows for expansion of vessels in the lung root, especially the inferior pulmonary vein.
Vessels and nerves
The vessels and nerves of the parietal pleura are derived from somatic sources. The arterial supply is from the intercostal, internal thoracic and musculophrenic arteries. The venous drainage is to the azygos system of veins. The lymphatics pass to the intercostal, parasternal, diaphragmatic and posterior mediastinal nodes. Intercostal nerves supply the costovertebral pleura. The diaphragmatic pleura is supplied by the phrenic nerve over the domes, and by intercostal nerves around its periphery. The mediastinal pleura is supplied by the phrenic nerve.
The arterial supply and venous drainage of the visceral pleura are provided by the bronchial vessels. The lymphatics join those of the lung (see p. 216). The visceral pleura has an autonomic nerve supply and is insensitive to ordinary stimuli.
Surface markings
The parietal pleura lines the costal walls of the thorax; seen from in front its lateral surface marking is the horizon of the thoracic cage (Fig. 4.28). It projects up to 2.5 cm above the junction of the middle and medial thirds of the clavicle. Due to the obliquity of the thoracic inlet, the pleura does not extend above the neck of the first rib, which lies well above the clavicle.

Figure 4.28 Surface markings of the lungs and pleurae.
Tracing the pleura now (Fig. 4.28) from behind the sternoclavicular joint, downwards behind the sternum and around the costodiaphragmatic gutter, there is a point to be noted at the level of each of the even-numbered ribs (2, 4, 6, 8, 10, 12). The line of pleural reflexion slopes downwards from the sternoclavicular joint to meet its fellow at the second rib level, that is, at the sternal angle. Lying together, or even overlapping, they pass vertically behind the sternum down to the fourth costal cartilage. Here the right pleura continues vertically, but the left arches out and descends lateral to the border of the sternum, half-way to the apex of the heart. Each turns laterally at the sixth costal cartilage, and passing around the chest wall crosses the midclavicular line at the eighth rib, and the midaxillary at the tenth rib. This lower border crosses the twelfth rib at the lateral border of erector spinae and passes in horizontally to the lower border of the twelfth thoracic vertebra. There is thus a triangle of pleura in the costovertebral angle below the medial part of the twelfth rib, behind the upper pole of the kidney, a fact to be noted in incisions and wounds in this region (see Fig. 5.48, p. 283).
Pleural aspiration and drainage
The anatomy of an intercostal space determines the route for removing fluid (or air) from the pleural cavity. Aspiration needles or drainage tubes are passed through the chest wall close to the upper border of a rib (lower part of an intercostal space) to avoid the vessels and nerve which course along the lower border of a rib (upper part of a space) (Fig. 4.4). The choice of space may be determined by the localization of fluid, e.g. a walled-off abscess, but for general purposes the fourth space in or just in front of the midaxillary line is often chosen. A needle, trocar and cannula or drainage tube inserted here is not near any major structure and is high enough to avoid the dome of the diaphragm.

Part nine. Lungs
Each lung, consisting of two lobes on the left and three on the right, lies within its own side of the thoracic cavity and is surrounded by the visceral layer of the pleura. Each has a principal or main bronchus, one pulmonary artery and two pulmonary veins, all of which undergo subdivisions within the lung substance, together with bronchial vessels, nerves and lymphatics. The region of the mediastinum where the lung is connected to the trachea and heart is the root of the lung, and the region of the lung where the bronchi and pulmonary vessels enter or leave is the hilum.
The lung surface is mottled, and in colour is pink or grey according to the atmosphere in which its owner has lived. It is crepitant to the touch.
The lung conforms to the shape of the cavity which contains it. It has a convex costal surface and a concave diaphragmatic surface, separated from each other by a sharp inferior border. The posterior border of each lung is generously rounded to fit the paravertebral gutter, and is continued up to the convex apex. The anterior border is thin and sharp; on the left side the lower part of this border is deeply concave—the cardiac notch. The mediastinal surfaces differ somewhat. On the left side the cardiac notch is seen to be the anterior margin of a deep concavity produced by the pericardium in front of the hilum; the arch and ascending aorta make a deep groove on the lung surface around the hilum. Above the aortic arch are vertical impressions made by the subclavian artery and (behind the artery) the oesophagus. On the right the cardiac impression is much shallower; a groove for the azygos vein curves over the hilum to meet the impression made by the superior vena cava. Above the azygos arch and behind the vena cava is a shallow groove for the trachea and right vagus. The apices are grooved by the subclavian arteries (Fig. 4.10). Inferiorly, in front of the lower end of the pulmonary ligament, both lungs may have shallow impressions, on the left lung for the oesophagus and on the right lung for the inferior vena cava.
Lung roots
The left and right lung roots are similar but not identical.
In the left lung root (Fig. 4.13) the upper part is occupied by the left pulmonary artery lying within the concavity of the arch of the aorta. Below it is the left bronchus. There are two pulmonary veins, one in front of and the other below the bronchus. These structures are enclosed in a sleeve of pleura continuous below with the pulmonary ligament.
In the right lung root (Fig. 4.12) the general arrangement of structures is similar to that on the left, but the bronchus to the upper lobe and the branch of the pulmonary artery to the upper lobe originate outside the lung. Thus the upper lobe bronchus and its accompanying artery are found above the level of the main bronchus and pulmonary artery, the arteries lying in front of their respective bronchi; the right hilum is consequently larger than the left. The two pulmonary veins are disposed as on the left side, in front of and below the main bronchus. The root of the right lung lies within a sleeve of pleura with a dependent pulmonary ligament, as on the left.
In addition to the above large structures, each root contains bronchial vessels, autonomic nerves and lymph nodes and channels.
Pulmonary arteries
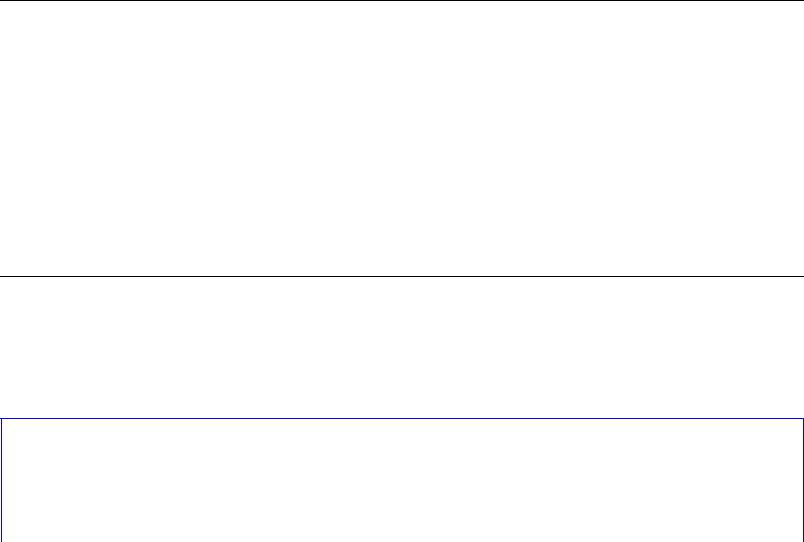
T he left pulmonary artery attached to the undersurface of the aortic arch by the ligamentum arteriosum, quickly spirals over the top of the left bronchus. The right pulmonary artery, longer than the left, passes below the carina anterior to the oesophagus, and at the lung root is anterior to the right main bronchus (Fig. 4.29). It gives off its branch to the upper lobe and then enters the hilum.
Figure 4.29 Bifurcation of the pulmonary trunk and the pulmonary arteries. The trunk divides in front of the left main bronchus. The left pulmonary artery spirals over the main bronchus to descend behind the lobar bronchi. The right pulmonary artery crosses below the tracheal bifurcation (in front of the oesophagus), and its descent behind the lower lobe bronchus is delayed because the artery is held anterior at the lung root by the upper lobe bronchus. The lungs are represented schematically.
Fissures
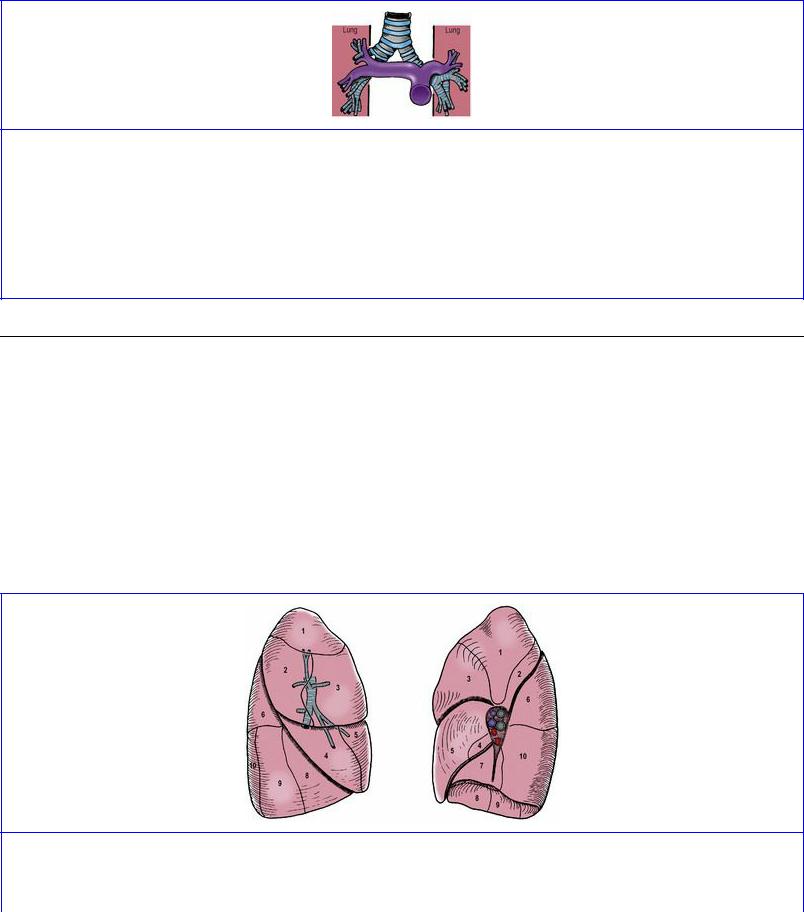
The oblique fissure (Figs 4.30 and 4.31) extends from the surface of the lung to the hilum and divides the organ into separate upper and lower lobes which are connected only by the lobar bronchi and vessels. In some lungs the fissure may not be complete. On the right lung a horizontal fissure (Fig. 4.30) passes from the anterior margin into the oblique fissure to separate a wedge-shaped middle lobe from the upper lobe. The visceral pleura, clothing the surface of the lung, extends inwards to line the depths of the fissures. The middle lobe of the right lung may not be completely separate from the upper lobe, the fissure separating it from the upper lobe being incomplete or even absent. In the left lung the lowest and most medial part of the upper lobe that overlaps the front of the pericardium is the lingula and forms the boundary of the cardiac notch.
Figure 4.30 Bronchopulmonary segments of the right lung, lateral and medial surfaces. Note the distribution of the upper and middle lobe bronchi and the posterior origin of the superior bronchus of the lower lobe (6).

Figure 4.31 Bronchopulmonary segments of the left lung, lateral and medial surfaces. Note the distribution of the lingular bronchi of the upper lobe and the posterior origin of the superior bronchus of the lower lobe (6), as in the right lung.
Surface markings
The hilum of each lung lies approximately behind the third and fourth costal cartilages at the sternal margin, and level with T5–7 vertebrae.
On upper costal walls and the supraclavicular region, the surface markings of the lungs coincide with those of the pleura (Fig. 4.28). The anterior border of the right lung falls very little short of the pleura, lying within the lateral margin of the sternum; that of the left lung in contrast curves laterally to uncover the area of superficial cardiac dullness from the fourth costal cartilage out to the fifth intercostal space just medial to the midclavicular line. The lower border of the lung lies nearly horizontally around the chest wall, but two ribs higher than the pleural reflexion, i.e. in the midclavicular line at the sixth rib, midaxillary line at the eighth rib, and at the lateral border of erector spinae at the tenth rib.
The oblique fissures of each lung are indicated by a line joining the spine of the T3 vertebra, which is opposite the posterior end of the fifth rib, to the sixth rib in the midclavicular line. More simply, this is approximately the line of the fifth rib, or level with the vertebral border of the scapula when the arm is fully abducted above the head. On the right the fourth costal cartilage overlies the horizontal fissure between the upper and middle lobes; continued horizontally this line meets the oblique fissure in the midaxillary line.
Lobar and segmental bronchi
Because the left lung grows into a smaller cavity than the right, the way bronchi divide to supply segments of lung is not identical on the two sides, although there are close similarities.
From the bifurcation of the trachea each main bronchus (Fig. 4.32) passes downwards and laterally to enter the hilum of the lung. The right main bronchus is 2.5 cm long and shorter, wider and more vertical than the left, which is 5 cm long. At the bifurcation the lowest tracheal cartilage has a hook-
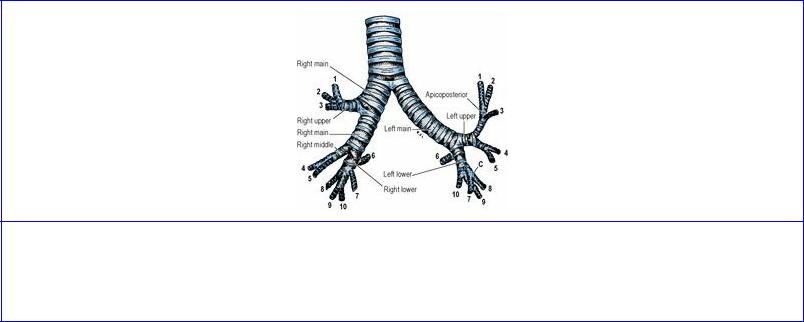
shaped process, the carina, which curves backwards between the bronchi and raises an anteroposterior internal ridge that lies to the left of the midline. Foreign bodies that fall down the trachea are more likely to enter the right bronchus.
Figure 4.32 Main, lobar and segmental bronchi. The main and lobar bronchi are named, the segmental bronchi are given their numbers as listed in the text, and the common stem for the left 7 and 8 bronchi is labelled C.
Each main bronchus gives rise to lobar bronchi (Fig. 4.32) that supply the lobes of the lung. The right main bronchus gives off the upper lobe bronchus outside the hilum and ends within the hilum by dividing into middle and lower lobe bronchi. The left main bronchus divides within the hilum into upper and lower lobar bronchi. The tissues of the bronchi are supplied by the bronchial arteries. The veins of the right main bronchus drain to the azygos vein and those of the left to the accessory hemiazygos vein.
Each lobar bronchus gives rise to further branches, the segmental bronchi (Fig. 4.32), for each segment of the lung. There are typically 10 bronchopulmonary segments in each lung and therefore 10 segmental bronchi; some left segmental bronchi may share a common stem. Each lung segment is roughly pyramidal in shape, with its apex towards the hilum and base towards the surface of the lung. The bronchopulmonary segments are given the same names and numbers as the segmental bronchi, which are listed as follows:
Right lung |
Left lung |
||
Upper lobe |
Upper lobe |
||
1. |
Apical |
1. |
Apical |
2. |
Posterior |
2. |
Posterior |
3. |
Anterior |
3. |
Anterior |
Middle lobe |
|
|
|
4. |
Lateral |
4. |
Superior lingular |
5. |
Medial |
5. |
Inferior lingular |
Lower lobe |
Lower lobe |
||
6. |
Superior (apical) |
6. |
Superior (apical) |
7. |
Medial basal (cardiac) |
7. |
Medial basal (cardiac) |
|
|
|
|
8. |
Anterior basal |
8. |
Anterior basal |
9. |
Lateral basal |
9. |
Lateral basal |
10. Posterior basal |
10. Posterior basal. |
||
From the above it can be seen that the bronchi and segments of the two lungs are very similar. The upper lobe of the right lung bronchus arises from the lateral aspect of the main bronchus and divides into three segmental bronchi. The middle lobe bronchus arises from the front of the main bronchus and divides into lateral and medial segmental bronchi. The upper lobe of the left lung has five segments, the first two (numerically) being supplied by bronchi that have a common apicoposterior stem. The lingular part of the left upper lobe has segments called superior and inferior; otherwise the names on the two sides are identical. Both lower lobes have five segmental bronchi and segments. On the left the medial and anterior basal segments arise from a common stem bronchus which subsequently subdivides.
On both sides the superior (apical) segment of the lower lobe is supplied by a bronchus (6) which is the highest to arise from the posterior surface of the bronchial tree. Material aspirated by a supine, comatose or anaesthetized patient would tend to gravitate into the superior segment of the right lower lobe, which is consequently a common site for aspiration pneumonia and abscess formation.
Blood supply
The bronchial tree receives its own arterial supply by the bronchial arteries. There are usually three: two on the left which are direct branches from the aorta, and one on the right coming from the third right posterior intercostal artery. They supply the bronchi from the carina to the respiratory bronchioles and the visceral pleura. The bronchial veins fall into a superficial system draining from the hilar region and visceral pleura into the azygos vein on the right and the accessory hemiazygos on the left, and a deep system from the deeper lung substance draining to a main pulmonary vein (thus mixing venous with oxygenated blood). The alveoli contain within their walls a rich capillary plexus which is fed with deoxygenated blood by the pulmonary artery. The pulmonary artery divides with the bronchi; every bronchus is accompanied by a branch of the artery. The artery supplies no bronchus but it does supply the alveoli, giving them all they need except oxygen, of which they have more than enough. There is some anastomosis between the bronchial and pulmonary arteries at precapillary level. The pulmonary veins are formed from tributaries which do not closely follow the bronchi but tend to run in the intersegmental septa. Two pulmonary veins leave each hilum, one from above and one from below the oblique fissure.
Lymph drainage
Lymphatic vessels in the lung originate in a superficial subpleural plexus and a deep submucosal plexus. They drain along the lung surface and with the pulmonary vessels to bronchopulmonary, or hilar, nodes in the hilum of each lung. Efferents from bronchopulmonary nodes run to tracheobronchial nodes. Lymphatics from the upper and middle lobes tend to drain to superior, and those from the lower lobes to inferior, tracheobronchial nodes, but these connections are not exclusive.
Nerve supply
Autonomic nerve fibres from the cardiac plexuses, and directly from the thoracic vagus and
sympathetic chain, pass to the pulmonary plexuses, which are situated anterior and posterior to other hilar structures, the anterior plexus being much smaller than the posterior. From here nerve fibres pass into the lung with the bronchi and vessels. The parasympathetic (vagal) fibres are afferent (cell bodies in the inferior ganglion) and efferent (cell bodies in dorsal nucleus, with relay in the bronchial mucosa). They provide the afferent fibres for the cough reflex (see p. 395), important for clearing excess secretions and inhaled substances from the tracheobronchial tree; the receptors are unmyelinated endings in the epithelium. Included among the afferent fibres are those subserving pain. The vagal efferents are bronchoconstrictor, vasodilator and secretomotor to mucous glands. The sympathetic preganglionic fibres originate from cells in the lateral horn of the T2-4 segments of the spinal cord; they relay in the upper thoracic ganglia. The sympathetic efferents are bronchodilator and vasoconstrictor.
Structure
Bronchi have smooth muscle and hyaline cartilage in their walls and are lined by the typical respiratory type of epithelium, pseudostratified columnar ciliated, with mucous glands. By successive divisions they become smaller and smaller; when cartilage disappears (at a diameter of about 1 mm) bronchi become bronchioles. After repeated branching, a lobular bronchiole enters each lung lobule and divides into terminal bronchioles which are the most distal air passages lined by typical respiratory epithelium. They subdivide into respiratory bronchioles, so called because some alveoli (air sacs) open directly off their walls. Beyond the respiratory bronchioles are alveolar ducts which have a lining of cubical epithelium (but no cilia) and many alveoli. Finally there are the alveolar sacs which have walls studded with alveoli.
The walls of the alveoli are lined by two types of epithelial cells covering a layer of connective tissue which contains capillaries. Over 90% of the lining consists of squamous type I alveolar cells through which gaseous exchange can occur. The rest of the alveolar wall is lined by smaller, rounded type II alveolar cells, containing lamellar bodies with a high phospholipid content; when discharged from the cell they produce the surfactant effect (reducing surface tension). Migratory macrophages are also present on the epithelial surface and within the alveolar lumen.
Development
Each lung develops from a bud at the lower end of the laryngotracheal tube that grows down from the floor of the primitive pharynx (see Fig. 1.19, p. 24). These endodermal buds form the epithelial part of the lung; the connective tissue, cartilage and muscle of the bronchial tree are derived from the surrounding mesoderm. By the fifth month the lung has a glandular appearance, with clumps of epithelial cells and hardly any recognizable lumina. The cell groups proliferate, become canalized and lie adjacent to capillaries so that by the seventh month there are sufficient alveoli to sustain a viable infant following premature birth at this time. Surfactant begins to be secreted about the sixth month.
In the fetus the lungs are not just a mass of collapsed air spaces but are full of fluid, largely secreted by the lungs but with a contribution from swallowed amniotic fluid. At the time of birth some is squeezed out by thoracic pressure and the rest escapes into blood capillaries and lymphatics, assisted by surfactant action. After birth there is no new development of any kind of bronchioles, but more than 80% of the adult number of alveoli are budded off during about the first 8 years of life.
Surgical approach
For pneumonectomy the approach on each side is usually a posterolateral thoracotomy through the bed of the sixth rib. It is necessary to divide the main pulmonary artery, both pulmonary veins and the main bronchus, but the sequence in which these principal structures are divided varies in accordance with their ease of isolation and the pathological indication for pneumonectomy. On the left the vagus is divided distal to the recurrent laryngeal branch, and the pulmonary artery is divided distal to the ligamentum arteriosum. The nearness of the aortic arch may make closure of the bronchus difficult. On the right the arch of the azygos vein is preserved if possible, as it affords collateral circulation if the superior vena cava is obstructed. The latter may have to be displaced forwards to allow satisfactory ligation of the pulmonary artery.
Part ten. Osteology of the thorax
Sternum
The sternum consists of an uppermost manubrium, an intermediate body and a small lowermost xiphoid process (Fig. 4.3). The manubrium and body are connected by a secondary cartilaginous joint (see p. 181). Like the ribs, most of the sternum is made of cancellous bone which throughout life is filled with haemopoietic, red marrow.
The manubrium is a flat four-sided bone broader above than below (Fig. 4.5). Its upper margin is concave, the jugular notch, on which lies the adherent interclavicular ligament. The two layers of the investing layer of deep cervical fascia are attached to the anterior and posterior borders of the notch ( s e e p. 330). Each upper angle of the manubrium is scooped out into a concavity for the sternoclavicular joint, an atypical synovial joint (see p. 43). Below this the lateral border is excavated for the first costal cartilage, which articulates here by a primary cartilaginous joint (see p. 181). At the inferior angle is a small facet for articulation (synovial) with the upper part of the second costal cartilage. Between the first and second costal cartilages the internal intercostal muscle is attached to the lateral border. The anterior surface is mainly covered by the attachment of pectoralis major but also gives attachment to the tendon of sternocleidomastoid. Sternohyoid and sternothyroid are attached to the upper part of the posterior surface. The manubrium forms the anterior wall of the superior mediastinum.
The body of the sternum has articular facets along its lateral border for the lower part of the second costal cartilage and for the third to seventh costal cartilages, all these articulations being synovial joints (Fig. 4.3). Between the costal facets the lateral border gives attachment to the anterior intercostal membrane and the internal intercostal muscle. Pectoralis major arises widely from the anterior surface almost to the midline, and transversus thoracis arises from the posterior surface low down. From the posterior surface weak sternopericardial ligaments pass to the fibrous pericardium.
From the posterior margin of the lower end of the sternal body the xiphoid process (xiphisternum) projects downwards for attachment of the linea alba. It articulates with the body by a symphysis which usually ossifies in middle age.
Surface markings
The sternal angle is palpable and the second costal cartilage can be felt at either side of the angle; the ribs can be counted down from here. On account of the downward inclination of the ribs, the jugular notch lies at the level of the upper border of the third, the sternal angle at the lower border of the fourth, and the lower end of the sternum at the lower border of the eighth thoracic vertebral bodies.
Ribs
A typical rib
A typical rib from the middle of the series has a head, a neck and a shaft; a tubercle projects posteriorly from the lateral end of the neck (Fig. 4.33).

Figure 4.33 Typical left rib: posterior aspect.
The head is bevelled by two articular facets that slope away from a dividing ridge. The lower facet is vertical; it articulates with its own vertebra and the upper, sloping facet articulates with the vertebra above. Each makes a synovial joint, and the cavities are separated by a ligament attached to the ridge on the head and to the intervertebral disc.
The neck is flattened, with a sharp crest forming the upper border. The two laminae of the superior costotransverse ligament are attached to the crest (Fig. 4.2). The neck of the rib inclines backwards when traced from head to tubercle.
The tubercle shows two facets. The smooth medial facet makes a synovial joint with the transverse process of its own vertebra; upper ribs have slightly convex, and lower ribs have flat, facets. The rough lateral facet gives attachment to the lateral costotransverse ligament.
The shaft slopes down and back to the angle and there twists forward in its characteristic curvature. Anterior to the angles the shafts of ribs are curved to form arcs of circles whose diameters increase from above downwards. On account of torsion at their angles, the heads of ribs lie at a higher level than their anterior ends; the degree of torsion is most marked in the seventh to ninth ribs. The upper border of a rib is blunt. It gives attachment in its whole length to the external and from the angle forwards to the internal intercostal muscles. The lower border of the shaft is sharp and hangs down to produce a well-marked costal groove on the inner surface. The external intercostal muscle arises from the sharp lower border and the internal intercostal is attached to the costal groove. The transverse thoracic group of muscles are attached to the inner surface of the shaft. The neurovascular bundle lies between this layer and the internal intercostal muscle, deep to the costal groove (Fig. 4.4). The anterior end of the rib is excavated into a concave fossa which is plugged by the costal cartilage in an immovable primary cartilaginous joint.
Atypical ribs
First rib
The first rib (Fig. 4.34) is the strongest, broadest, flattest and most curved rib. Its superior surface is part of the root of the neck; its inferior (pleural) surface is part of the roof of the thoracic cavity. The neck slopes upwards, backwards and laterally from the head to the tubercle. Hence if the rib is laid on the table, the head and anterior extremity both touch the surface, but laid upside down the head lies above the table; this enables right and left sides to be identified. The plane of the shaft is at 45° to the horizontal, with the tubercle the most posterior and highest part of the rib.

Figure 4.34 Right first rib, from above, and with attachments.
The head is small and carries a single facet for the synovial joint it makes with the upper part of the body of T1 vertebra. The sympathetic trunk (or cervicothoracic ganglion) lies in contact with the anterior border of the neck alongside the head. Lateral to it the first posterior intercostal vein and then the superior intercostal artery lie in contact, and more lateral still the first thoracic nerve lies in front of the neck. The cervical dome of the pleura and the apex of the lung hold these vessels and nerves against the front of the neck of the rib.
The rib broadens at the junction of neck and shaft, where a prominent tubercle projects back to form the most posterior convexity of the rib. It is a fusion of tubercle and angle. Medially it has a convex facet for a corresponding concavity on the first transverse process. The lateral prominent part of the tubercle receives the lateral costotransverse ligament.
The undersurface of the shaft, crossed obliquely by the small first intercostal nerve and vessels, is covered by adherent parietal pleura. The external and internal intercostal muscles are attached together to the outer rim of this surface. The outer border is blunt between the tubercle and subclavian groove and the first digitation of serratus anterior is attached to the anterior part of this blunt area. The concave internal border of the shaft gives attachment to the suprapleural membrane in front of the subclavian groove (Fig. 4.5).
The upper surface of the shaft is grooved obliquely at its greatest lateral convexity. Called the groove for the subclavian artery, it lodges the lower trunk of the brachial plexus as well, behind the artery. The fibres in contact with the rib are all T1, the C8 fibres lying above them (Fig. 4.34). Between the groove and the tubercle the large quadrangular area of the upper surface gives attachment to scalenus medius. At the front of the groove the inner border is projected into a small spur, the scalene tubercle. The tendon of scalenus anterior is attached to the tubercle and extends along a triangular impression on the upper surface which may be more discernable than the tubercle itself. Anterior to the attachment of scalenus anterior is another groove on the upper surface of the shaft in which the subclavian vein lies. The anterior end of the shaft expands into a concavity for the first costal cartilage. From the upper surface of this junction subclavius arises from both bone and cartilage.
Eleventh rib
The eleventh rib has a head, with a single facet for T11 vertebra, a short neck, no tubercle, a slight angle and a shallow costal groove.
Twelfth rib
The twelfth rib varies in length. The head has a single facet for T12 vertebra. A short constriction
forms a neck which passes imperceptibly into the shaft. There is no tubercle, no angle and no costal groove. The inner surface of the shaft faces slightly upwards.
Ossification of the sternum
In two longitudinal cartilaginous plates that fuse in the midline, a variable number of primary centres appear at about the fifth fetal month and later. There are one or two in the manubrium, and one or two in each of the four pieces (sternebrae) that will form the body of the sternum. The double centres coalesce, and fusion between sternebrae occurs between puberty and 25 years. Sternal foramina (‘bullet holes’) in the adult sternum are the result of incomplete fusion of double centres. The cartilaginous xiphoid process may ossify any time after the third year but often not until later life.
Ossification of ribs
Primary ossification centres appear at the eighth week of fetal life at the angle, and ossification proceeds anteriorly and posteriorly from here. At birth the unossified anterior end remains as the costal cartilage. Secondary centres for the head and tubercle appear at puberty and fuse with the shaft after 20 years.
Costal cartilages
These form primary cartilaginous joints at the extremities of all twelve ribs. The first is short and thick, and forms also a primary cartilaginous joint with the manubrium. It articulates also with the clavicle and gives attachment to the sternoclavicular disc and the costoclavicular ligament.
Below this the cartilages increase in length down to the seventh, which is the longest. From the fifth to the tenth they are bent from a downward slope in line with the rib to an upward slope towards the sternum (Fig. 4.3). Their medial ends form synovial joints with the sternum or the cartilage above (see p. 181). The cartilages of the eleventh and twelfth ribs have free pointed anterior ends. All cartilages, especially the first, tend to calcify and even ossify in patches after middle age.
