
- •Preface
- •Acknowledgments
- •Reviewers
- •Contents
- •CHAPTER OUTLINE
- •CYTOPLASM
- •Plasmalemma
- •Mitochondria
- •Ribosomes
- •Endoplasmic Reticulum
- •Golgi Apparatus, cis-Golgi Network, and the trans-Golgi Network
- •Endosomes
- •Lysosomes
- •Peroxisomes
- •Proteasomes
- •Cytoskeleton
- •Inclusions
- •NUCLEUS
- •CELL CYCLE
- •CHAPTER OUTLINE
- •EPITHELIUM
- •Epithelial Membranes
- •GLANDS
- •Chapter Summary
- •CHAPTER OUTLINE
- •EXTRACELLULAR MATRIX
- •Fibers
- •Amorphous Ground Substance
- •Extracellular Fluid
- •CELLS
- •CONNECTIVE TISSUE TYPES
- •Chapter Summary
- •CHAPTER OUTLINE
- •CARTILAGE
- •BONE
- •Cells of Bone
- •Osteogenesis
- •Bone Remodeling
- •Chapter Summary
- •CHAPTER OUTLINE
- •FORMED ELEMENTS OF BLOOD
- •Lymphocytes
- •Neutrophils
- •PLASMA
- •COAGULATION
- •HEMOPOIESIS
- •Erythrocytic Series
- •Granulocytic Series
- •Chapter Summary
- •CHAPTER OUTLINE
- •SKELETAL MUSCLE
- •Sliding Filament Model of Muscle Contraction
- •CARDIAC MUSCLE
- •SMOOTH MUSCLE
- •Chapter Summary
- •CHAPTER OUTLINE
- •BLOOD-BRAIN BARRIER
- •NEURONS
- •Membrane Resting Potential
- •Action Potential
- •Myoneural Junctions
- •Neurotransmitter Substances
- •SUPPORTING CELLS
- •PERIPHERAL NERVES
- •Chapter Summary
- •CHAPTER OUTLINE
- •BLOOD VASCULAR SYSTEM
- •HEART
- •ARTERIES
- •Capillary Permeability
- •Endothelial Cell Functions
- •VEINS
- •LYMPH VASCULAR SYSTEM
- •Chapter Summary
- •CHAPTER OUTLINE
- •CELLS OF THE IMMUNE SYSTEM
- •Antigen-Presenting Cells
- •DIFFUSE LYMPHOID TISSUE
- •LYMPH NODES
- •TONSILS
- •SPLEEN
- •THYMUS
- •Chapter Summary
- •CHAPTER OUTLINE
- •PITUITARY GLAND
- •Pars Intermedia
- •Pars Nervosa and Infundibular Stalk
- •Pars Tuberalis
- •THYROID GLAND
- •Parathyroid Glands
- •Suprarenal Glands
- •Cortex
- •Medulla
- •Pineal Body
- •Chapter Summary
- •CHAPTER OUTLINE
- •SKIN
- •Epidermis of Thick Skin
- •Dermis
- •DERIVATIVES OF SKIN
- •Chapter Summary
- •CHAPTER OUTLINE
- •CONDUCTING PORTION OF THE RESPIRATORY SYSTEM
- •Extrapulmonary Region
- •Intrapulmonary Region
- •RESPIRATORY PORTION OF THE RESPIRATORY SYSTEM
- •MECHANISM OF RESPIRATION
- •Chapter Summary
- •CHAPTER OUTLINE
- •ORAL CAVITY AND ORAL MUCOSA
- •Oral Mucosa
- •Tongue
- •Teeth
- •Odontogenesis (See Graphic 13-2)
- •Chapter Summary
- •CHAPTER OUTLINE
- •REGIONS OF THE DIGESTIVE TRACT
- •Esophagus
- •Stomach
- •Small Intestine
- •Large Intestine
- •GUT-ASSOCIATED LYMPHOID TISSUE
- •DIGESTION AND ABSORPTION
- •Carbohydrates
- •Proteins
- •Lipids
- •Water and Ions
- •Chapter Summary
- •CHAPTER OUTLINE
- •MAJOR SALIVARY GLANDS
- •PANCREAS
- •LIVER
- •Exocrine Function of the Liver
- •Endocrine and Other Functions of the Liver
- •GALLBLADDER
- •Chapter Summary
- •CHAPTER OUTLINE
- •KIDNEY
- •Uriniferous Tubule
- •Nephron
- •Collecting Tubules
- •FORMATION OF URINE FROM ULTRAFILTRATE
- •EXTRARENAL EXCRETORY PASSAGES
- •Chapter Summary
- •CHAPTER OUTLINE
- •OVARY
- •Ovarian Follicles
- •Regulation of Follicle Maturation and Ovulation
- •Corpus Luteum and Corpus Albicans
- •GENITAL DUCTS
- •Oviduct
- •Uterus
- •FERTILIZATION, IMPLANTATION, AND THE PLACENTA
- •Fertilization and Implantation
- •Placenta
- •VAGINA
- •EXTERNAL GENITALIA
- •MAMMARY GLANDS
- •Chapter Summary
- •CHAPTER OUTLINE
- •TESTES
- •Spermatogenesis
- •GENITAL DUCTS
- •ACCESSORY GLANDS
- •PENIS
- •Erection and Ejaculation
- •Chapter Summary
- •CHAPTER OUTLINE
- •SENSORY ENDINGS
- •Chapter Summary
- •Terminology of Staining
- •Common Stains Used in Histology
- •Hematoxylin and Eosin
- •Wright Stain
- •Weigert Method for Elastic Fibers and Elastic van Gieson Stain
- •Silver Stain
- •Iron Hematoxylin
- •Bielschowsky Silver Stain
- •Masson Trichrome
- •Periodic Acid-Schiff Reaction (PAS)
- •Alcian Blue
- •von Kossa Stain
- •Sudan Red
- •Mucicarmine Stain
- •Safranin-O
- •Toluidine Blue

260 I N T E G U M E N T
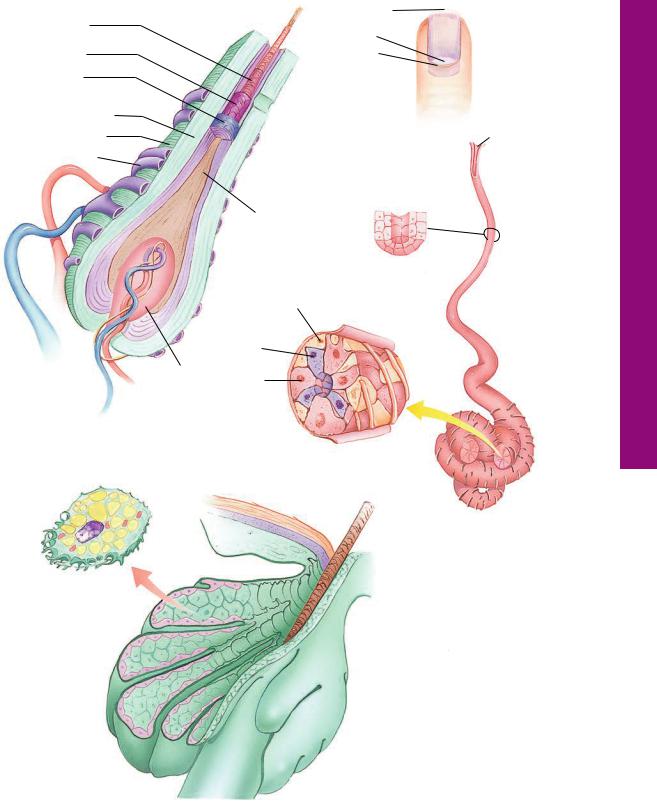
DERIVATIVES OF SKIN
Derivatives of skin include hair, sebaceous glands, sweat glands, and nails (see Graphic 11-2). These structures originate from epidermal downgrowths into the dermis and hypodermis, while maintaining their connection to the outside.
•Each hair is composed of a shaft of cornified cells and a root contained within a hair follicle
is associated with a sebaceous gland that secretes an oily sebum into the neck of the hair follicle.
A small bundle of smooth muscle cells, the arrector pili muscle, attaches to the hair follicle and, cradling the sebaceous gland, inserts into the superficial aspects of the skin.
•Sweat glands do not develop in association with hair follicles.These are simple, coiled, tubular glands whose secretory units produce sweat, which is delivered to the surface of the skin by long ducts.
Myoepithelial cells surround the secretory portion of these glands.
•Nails are cornified structures on the distal phalanx of each finger and toe. These horny plates lie on a nail bed and are bounded laterally by a nail wall.
The cuticle (eponychium) lies over the lunula, an opaque, crescent-shaped area of the nail plate.
The hyponychium is located beneath the free edge of the nail plate.
CLINICAL CONSIDERATIONS
Itching (Pruritis)
The sensation of itching is accompanied by an instinctive, almost irrepressible urge to scratch. There are many different causes of itching, some as simple as a fly walking on one’s skin and moving the hair follicles, or as serious as debilitating systemic conditions such as kidney failure or liver disease. If the itching is accompanied by a rash, then the probable cause is not the kidney or the liver. Parasitic infestations (mites, scabies, etc.), insect bites, plant toxins (such as poison oak and poison ivy), and drug allergies are usually accompanied by a rash and require medical intervention. If the itching is long-term, the patient should seek the assistance of a physician. Pregnancy and cold, dry weather may also be contributing factors to itching.
Psoriasis Vulgaris
Psoriasis vulgaris is a commonly occurring condition characterized by reddish patchy lesions on the skin with grayish sheen, located especially around joints, sacral region, the navel, and the scalp. This condition is produced by increased proliferation of keratinocytes and an acceleration of the cell cycle, resulting in an accumulation of cells in the stratum corneum but with an absence of a stratum granulosum and, frequently, the presence of lymphocytic infiltrates in the papillary layer. The condition is cyclic and is of unknown etiology.
This photomicrograph is of a patient suffering from psoriasis vulgaris. Note that the stratum spinosum and stratum corneum are thickened and that the stratum granulosum is absent. The papillary layer of the dermis displays an infiltration by lymphocytes. (Reprinted with permission from Mills SE, Carter D, et al., eds. Sternberg’s Diagnostic Surgical Pathology, 5th ed., Philadelphia, Lippincott, Williams & Wilkins, 2010,. p. 6.)
Erythema Multiforme
Patches of elevated red skin, frequently resembling a target, displaying a symmetrical distribution over the face and extremities, that occurs periodically indicate the disorder erythema multiforme. It is most frequently due

I N T E G U M E N T 261
CLINICAL CONSIDERATIONS
to herpes simplex infection. The condition is not usually accompanied by itching, although painful lesions (blisters) on the lips and buccal cavity are common occurrences. Usually the condition resolves itself, but in more severe cases, medical intervention is indicated.
Warts
Warts are benign epidermal growths on the skin caused by papilloma viral infection of the keratinocytes. Warts are common in young children, in young adults, and in immunosuppressed patients.
Vitiligo
A condition in which the skin has patches of white areas due to the lack of pigmentation is known as vitiligo. The melanocytes of the affected region are destroyed in an autoimmune response. The condition may appear suddenly after a physical injury or as a consequence of sunburn. If the area affected has hair, as the hair grows it will be white. Although there are no physical consequences to vitiligo, there may be psychological sequelae.
Malignancies of Skin
The three most common malignancies of skin are basal cell carcinoma, squamous cell carcinoma, and malignant melanoma.
Basal cell carcinoma, the most common human malignancy, develops in the stratum basale from
damage caused by ultraviolet radiation. The foremost type of basal cell carcinoma is the nodulocystic type where small hyperchromatic cells form spherical nodules that are separated from the surrounding connective tissue elements of the dermis by narrow spaces. The most frequent site of basal cell carcinoma is on the nose, occurring as papules or nodules, which eventually craters. Surgery is usually 90% effective with no recurrence.
Squamous cell carcinoma, the second most frequent skin malignancy, is invasive and metastatic. Its probable etiology is environmental factors, such as ultraviolet radiation and x-irradiation, as well as a variety of chemical carcinogens, including arsenic. The carcinoma originates in cells of the stratum spinosum and appears clinically as a hyperkeratotic, scaly plaque with deep invasion of underlying tissues, often accompanied by bleeding. Surgery is the treatment of choice.
Malignant melanoma may be a life-threatening malignancy. It develops in the epidermis where melanocytes become mitotically active and form a dysplastic nevus. It may then enter a radial-growth phase where individual melanocytes invade the dermis, then enter the vertical growth phase where they begin to form tumors in the dermis, and eventually become a full-fledged, metastatic melanoma whose cells eventually enter the lymphatic and circulatory system to metastasize to other organ systems.
This photomicrograph is of a patient with basal cell carcinoma. Note that the lesion is composed of dark, dense basal cells that form rounded nodules that are separated from the dermal connective tissue by narrowed spaces. (Reprinted with permission from Mills SE, Carter D, et al., eds. Sternberg’s Diagnostic Surgical Pathology, 5th ed., Philadelphia, Lippincott, Williams & Wilkins, 2010. p. 49.)
This photomicrograph is of a patient suffering from malignant melanoma. Note that the melanocytes are invading the dermis in large numbers, indicating that the melanoma is in the vertical growth phase. (Reprinted with permission from Mills SE, Carter D, et al., eds. Sternberg’s Diagnostic Surgical Pathology, 5th ed., Philadelphia, Lippincott, Williams & Wilkins, 2010. p. 92.)

Derivatives Its and Skin • 1-11 GRAPHIC
262 I N T E G U M E N T
Epidermis
Stratum corneum
Stratum spinosum
Stratum basale 
Dermis
Papillary layer Reticular layer
Eccrine sweat gland 
Apocrine sweat gland
Root hair plexus 
Hypodermis
(superficial fascia)
Meissner’s corpuscle
Hair shaft
Sebaceous (oil) gland
Arrector pili muscle
Eccrine sweat gland
Apocrine sweat gland
Hair follicle
 Hair root
Hair root
Pacinian corpuscle
 Artery
Artery
Vein
Adipose tissue of hypodermis
Skin and its appendages, hair, sweat glands (both eccrine and apocrine), sebaceous glands, and nails, are known as the integument. Skin may be thick or thin, depending on the thickness of its epidermis. Thick skin epidermis is composed of five distinct layers of keratinocytes (strata basale, spinosum, granulosum, lucidum, and corneum) interspersed with three additional cell types, melanocytes, Merkel’s cells, and Langerhans’ cells. Thin skin epidermis lacks strata granulosum and lucidum, although individual cells that constitute the absent layers are present.
Stratum corneum
Stratum lucidum 
Stratum granulosum 
Stratum spinosum
Langerhans’ cell |
Epidermis |
|
|
Merkel cell |
|
Melanocyte |
|
Basement membrane
Dermis
Blood vessel
Stratum basale
I N T E G U M E N T 263
Internal Root Sheath
Sheath cuticle
Huxley’s layer
Henle’s layer
External root sheath
Glassy membrane
Root hair plexus 
Hair papilla
Hair Root
Sebaceous cell
Free edge
Nail body 
Lunula
Cuticle
Nail root 
 Duct of
Duct of
sebaceous
gland
Pore
Hair shaft
Excretory duct
Myoepithelial cell
Dark cell
Clear cell
Secretory portion
Eccrine Sweat
Gland
Secretory components of eccrine sweat glands consist of simple cuboidal epithelium composed of dark cells, clear cells, and myoepithelial cells. The ducts of these glands are composed of a stratified cuboidal (two layers of cuboidal cells) epithelium.
|
|
Sebaceous glands are |
|
|
|
branched acinar holocrine |
|
|
|
glands whose short ducts |
|
|
|
empty into a hair follicle into |
|
Sebaceous |
Hair |
the space created by the |
|
disappearance of the |
|||
follicle |
|||
Gland |
internal root sheath. |
||
|
Glands Sebaceous and Glands, Sweat Hair,• 2-11 GRAPHIC

Skin hick • T1-11 PLATE
264 I N T E G U M E N T
FIGURE 1. Thick skin. Paraffin section. ×132.
Skin is composed of the superficial epidermis (E) and the deeper dermis (D). The interface of the two tissues is demarcated by epidermal ridges (ER) and dermal ridges (DR) (dermal papillae). Between successive epidermal ridges are the interpapillary pegs, which divide each dermal ridge into secondary dermal ridges. Note that in thick skin the keratinized layer, stratum corneum (SC), is highly developed. Observe also that the duct (d) of the sweat gland pierces the base of an epidermal ridge. The dermis of skin is subdivided into two regions, a papillary layer (PL), composed of the looser, collagenous connective tissue of the dermal ridges, and the deeper, denser, collagenous connective tissue of the reticular layer (RL). Blood vessels (BV) from the reticular layer enter the dermal ridges.
FIGURE 3. Thick skin. Monkey. Plastic section. ×540.
This is a higher magnification of a region similar to the boxed area in the previous figure. The papillary layer (PL) of the dermis displays nuclei (N) of the various connective tissue cells as well as the interface between the dermis and the stratum basale (SB). Observe that these cells are cuboidal to columnar in shape, and interspersed among them are occasional clear cells, probably inactive melanocytes (M), although it should be stressed that Merkel cells also appear as clear cells. Cells of the stratum spinosum (SS) are polyhedral in shape, possessing numerous intercellular bridges, which interdigitate with those of other cells, accounting for their spiny appearance.
FIGURE 2. Thick skin. Monkey. Plastic section. ×132.
This photomicrograph of thick skin presents a view similar to that in Figure 1. However, the layers of the epidermis (E) are much easier to delineate in this plastic section. Observe that the squames of the stratum corneum (SC) appear to lie directly on the stratum granulosum (SG), whose cells contain keratohyalin granules. The thickest layer of lining cells in the epidermis is the stratum spinosum (SS), whereas the stratum basale (SB) is only a single cell layer thick. The stratum lucidum is not evident, although a few transitional cells (arrows) may be identified. Note that the secondary dermal ridges (SDR), on either side of the interpapillary peg
(IP), present capillary loops (CL). Regions similar to the boxed areas are presented in Figures 3 and 4 at higher magnification.
FIGURE 4. Thick skin. Monkey. Plastic section. ×540.
This is a higher magnification of a region similar to the boxed area of Figure 2. Observe that as the cells of the stratum spinosum (SS) are being pushed surfaceward, they become somewhat flattened. As the cells reach the stratum granulosum (SG), they accumulate keratohyalin granules (arrows), which increase in number as the cells progress through this layer. Occasional transitional cells (arrowheads) of the poorly defined stratum lucidum may be observed as well as the squames (S) of the stratum corneum (SC). Inset. Thick skin. Paraffin section. ×132. This photomicrograph displays the stratum lucidum (SL) to advantage. Note that this layer is between the stratum granulosum (SG) and stratum corneum (SC). Observe the duct (d) of a sweat gland.
KEY
BV |
blood vessel |
IP |
interpapillary peg |
SDR |
secondary dermal ridges |
CL |
capillary loop |
M |
melanocytes |
SG |
stratum granulosum |
D |
dermis |
N |
nucleus |
SB |
stratum basale |
d |
duct |
PL |
papillary layer |
SS |
stratum spinosum |
DR |
dermal ridges |
RL |
reticular layer |
S |
squames |
E |
epidermis |
SC |
stratum corneum |
SL |
stratum lucidum |
ER |
epidermal ridges |
|
|
|
|

SC |
|
|
|
E |
|
|
|
|
|
|
|
|
|||
ER |
|
|
|
3 |
|
||
E |
|
|
|||||
|
SC |
|
|
SG |
|
|
|
|
|
|
SDR |
||||
|
|
|
|
|
|
||
|
|
|
|
|
IP |
||
CL
DR |
|
SS |
|
4 SB
d |
|
D |
|
|
|
RL |
BV |
|
|
|
|
|
FIGURE 1 |
FIGURE 2 |
N
S SG
PL
SS
SC
M
SS
SL
SB 
SG
d SC
FIGURE 3 |
FIGURE 4 |
Skin hick • T1-11 PLATE

Skin hin • T2-11 PLATE
266 I N T E G U M E N T
FIGURE 1. Thin skin. Human. Paraffin section. ×19.
Thin skin is composed of a very slender layer of epidermis (E) and
the underlying dermis (D). Although thick skin has no hair follicles |
|
|
|
|
Stratum basale |
|
|
|
|
|
|
and sebaceous glands associated with it, most thin skin is richly |
|
|
|
|
Papillary layer |
endowed with both. Observe the hair (H) and the hair follicles (HF), |
Epidermis |
|
|
|
|
|
|
|
|
||
whose expanded bulb (B) presents the connective tissue papilla |
|
|
|
|
Sebaceous gland |
|
|
|
|
||
|
|
|
|
||
(P). Much of the follicle is embedded beneath the skin in the super- |
Dermis |
|
|
|
Hair follicle |
ficial fascia, the fatty connective tissue layer known as the hypo- |
|
|
|
||
|
|
|
|
||
|
|
|
|
|
|
dermis (hD), which is not a part of the integument. Sebaceous |
|
|
|
|
Hair bulb |
glands (sG) secrete their sebum into short ducts (d), which empty |
Hypodermis |
|
|
|
|
|
|
|
|
||
into the lumen of the hair follicle. Smooth muscle bundles, arrec- |
|
|
|
|
|
|
|
|
|
|
|
tor pili muscle (AP), cradle these glands, in passing from the hair |
|
|
Sweat gland |
||
follicle to the papillary layer of the dermis. Sweat glands (swG) are |
|
|
|||
|
|
|
|
|
|
also present in the reticular layer of the dermis. A region similar to |
|
|
|
|
|
the boxed area is presented at a higher magnification in Figure 2. |
|
|
|
|
|
FIGURE 2. Thin skin. Human. Paraffin section. ×132.
This is a higher magnification of a region similar to the boxed area of the previous figure. Observe that the epidermis (E) is much thinner than that of thick skin and that the stratum corneum (SC) is significantly reduced. The epidermal ridges and interpapillary pegs (IP) are well represented in this photomicrograph. Note that the papillary layer (PL) of the dermis is composed of much finer bundles of collagen fibers (CF) than those of the dense irregular collagenous connective tissue of the reticular layer (RL). The dermis is quite vascular, as evidenced by the large number of blood vessels (BV) whose cross-sectional profiles are readily observed. The numerous nuclei (N) of the various connective tissue cells attest to the cellularity of the dermis. Note also the presence of the arrector pili muscle (AP), whose contraction elevates the hair and is responsible for the appearance of “goose bumps.” The boxed area is presented at a higher magnification in the following figure.
FIGURE 3. Thin skin. Human. Paraffin section. ×270.
This photomicrograph is a higher magnification of the boxed area of Figure 2. Epidermis of thin skin possesses only three of four of the layers found in thick skin. The stratum basale (SB) is present as a single layer of cuboidal to columnar cells. Most of the epidermis is composed of the prickle cells of the stratum spinosum (SS), whereas stratum granulosum and stratum lucidum are not represented as complete layers. However, individual cells of stratum granulosum (arrow) and stratum lucidum are scattered at the interface of the stratum spinosum and stratum corneum (SC). The papillary layer of the dermis (D) is richly vascularized by capillary loops (CL), which penetrate the secondary dermal ridges
(sDR). Observe that the collagen fiber (CF) bundles of the dermis become coarser as the distance from the epidermis increases.
KEY
AP |
arrector pili muscle |
H |
hair |
RL |
reticular layer |
B |
bulb |
hD |
hypodermis |
SC |
stratum corneum |
BV |
blood vessels |
HF |
hair follicles |
sDR |
secondary dermal ridges |
CF |
collagen fibers |
IP |
interpapillary peg |
sG |
sebaceous glands |
CL |
capillary loops |
N |
nuclei |
SB |
stratum basale |
D |
dermis |
P |
papilla |
SS |
stratum spinosum |
d |
ducts |
PL |
papillary layer |
swG |
sweat glands |
Eepidermis

HF
E 
D
 d
d
swG
AP
B
P |
hD |
|
FIGURE 1
SC
E
PL
IP
CF
N
AP
RL
 BV
BV
FIGURE 2
H
sG
SC
SS
sDR
CL
SB
CF D
D
FIGURE 3
Skin hin • T2-11 PLATE

Glands Sweat Structures, Associated and ollicles F Hair• 3-11 PLATE
268 I N T E G U M E N T
FIGURE 1. Hair follicle. l.s. Human. Paraffin section. ×132.
The terminal expansion of the hair follicle, known as the bulb, is composed of a connective tissue, papilla (P), enveloped by epithelially derived cells of the hair root (HR). The mitotic activity responsible for the growth of hair occurs in the matrix, from which several concentric sheaths of epithelial cells emerge to be surrounded by a connective tissue sheath (CTS). Color of hair is due to the intracellular pigment that accounts for the dark appearance of some cells (arrow).
FIGURE 3. Sebaceous gland. Human. Paraffin section. ×132.
Sebaceous glands (sG) are branched, acinar holocrine glands, which produce an oily sebum. The secretion of these glands is delivered into the lumen of a hair follicle (HF), with which sebaceous glands are associated. Basal cells (BC), located at the periphery of the gland, undergo mitotic activity to replenish the dead cells, which, in holocrine glands, become the secretory product. Note that as these cells accumulate sebum in their cytoplasm, they degenerate, as evidenced by the gradual pyknosis of their nuclei (N). Observe the arrector pili muscle (AP), which cradles the sebaceous glands.
FIGURE 2. Hair follicle. x.s. Human. Paraffin section. ×132.
Many of the layers comprising the growing hair follicle may be observed in these cross sections. The entire structure is surrounded by a connective tissue sheath (CTS), which is separated from the epithelially derived components by a specialized basement membrane, the inner glassy membrane (BM). The clear polyhedral cells compose the external root sheath (ERS), which surrounds the internal root sheath (IRS), whose cells become keratinized. At the neck of the hair follicle, where the ducts of the sebaceous glands enter, the internal root sheath disintegrates, providing a lumen into which sebum and apocrine sweat are discharged. The cuticle (Cu) and cortex (Co) constitute the highly keratinized components of the hair, whereas the medulla is not visible at this magnification. Note the presence of arrector pili muscle (AP).
FIGURE 4. Sweat gland. Monkey. Plastic section. ×132.
The simple, coiled, tubular eccrine gland is divided into two compartments: a secretory portion (s) and a duct (d). The secretory portion of the gland consists of a simple cuboidal epithelium, composed of dark and clear secretory cells (which cannot be distinguished from each other unless special procedures are utilized). Intercellular canaliculi are noted between clear cells, which are smaller than the lumen (L) of the gland. Ducts (d) may be recognized readily since they are darker staining and composed of stratified cuboidal epithelium. Insets a and b. Duct and secretory unit. Monkey. Plastic section. ×540. The duct is readily evident, since its lumen (L) is surrounded by two layers of cuboidal cells. Secretory cells (s) of the eccrine sweat gland are surrounded by darker-staining myoepithelial cells (My). Hair root, eccrine sweat gland, and sebaceous gland.
External root sheath |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||
Glassy membrane |
|
|
|
Myoepithelial |
Duct |
|
|
Duct |
||
|
|
|
||||||||
|
|
|
|
|
|
|||||
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
cell |
|
|
|
|
|
|
|
|
|
|
Dark cell |
|
|
|
|
|
|
|
|
Papilla |
Clear cell |
|
|
|
|
|
|
Hair root Eccrine sweat gland Sebaceous gland
KEY
AP |
arrector pili muscle |
d |
ducts |
L |
lumen |
BC |
basal cells |
ERS |
external root sheath |
My |
myoepithelial cells |
BM |
inner glassy membrane |
HF |
hair follicle |
N |
nucleus |
Co |
cortex |
HR |
hair root |
P |
papilla |
CTS |
connective tissue sheath |
IRS |
internal root sheath |
s |
secretory |
Cu |
cuticle |
|
|
sG |
sebaceous glands |

Co AP
CTS |
Cu |
|
IRS |
CTS
BM 
ERS
P
HR
FIGURE 1 |
FIGURE 2 |
BC |
L |
My |
|
s
s
N
d
b)
AP
sG
s
s
L
HF
d
a)
FIGURE 3 |
FIGURE 4 |
Glands Sweat Structures, Associated and ollicles F Hair• 3-11 PLATE

Corpuscles Meissner’s and Pacinian Nail,• 4-11 PLATE
270 I N T E G U M E N T
FIGURE 1. Fingernail. l.s. Paraffin section. ×14.
The nail is a highly keratinized structure that is located on the dorsal surface of the distal phalanx (Ph) of each finger and toe. The horny nail plate (NP) extends deep into the dermis, forming the nail root (NR). The epidermis of the distal phalanx forms a continuous fold, resulting in the eponychium (Ep) or cuticle, the nail bed (NB) underlying the nail plate, and the hyponychium (Hy). The epithelium (arrow) surrounding the nail root is responsible for the continuous elongation of the nail. The dermis (D) between the nail bed and the bone (Bo) of the distal phalanx is tightly secured to the fibrous periosteum (FP). Note that this is a developing finger, as evidenced by the presence of hyaline cartilage (HC) and endochondral osteogenesis (arrowheads).
FIGURE 3. Meissner’s corpuscle. Paraffin section. ×540.
Meissner’s corpuscles are oval, encapsulated mechanoreceptors lying in dermal ridges just deep to the stratum basale (SB). They are especially prominent in the genital areas, lips, fingertips, and soles of the feet. A connective tissue capsule (Ca) envelops the corpuscle. The nuclei (N) within the corpuscle belong to flattened (probably modified) Schwann cells, which are arranged horizontally in this structure. The afferent nerve fiber (NF) pierces the base of Meissner’s corpuscle, branches, and follows a tortuous course within the corpuscle.
FIGURE 2. Fingernail. x.s. Paraffin section. ×14.
The nail plate (NP) in cross section presents a convex appearance. On either side, it is bordered by a nail wall (NW), and the groove it occupies is referred to as the lateral nail groove (NG). The nail bed (NB) is analogous to four layers of the epidermis, whereas the nail plate represents the stratum corneum. The dermis (D), deep to the nail bed, is firmly attached to the fibrous periosteum (FP) of the bone (Bo) of the terminal phalanx. Observe that the fingertip is covered by thick skin whose stratum corneum (SC) is extremely well developed. The small, darkly staining structures in the dermis are sweat glands (swG).
FIGURE 4. Pacinian corpuscle. Paraffin section. ×132.
Pacinian corpuscles, located in the dermis and hypodermis, are mechanoreceptors. They are composed of a core with an inner (IC) and an outer (OC) region, as well as a capsule (Ca) that surrounds the core. The inner core invests the afferent nerve fiber (NF), which loses its myelin sheath soon after entering the corpuscle. The core cells are modified Schwann cells, whereas the components of the capsule are continuous with the endoneurium of the afferent nerve fiber. Pacinian corpuscles are readily recognizable in section since they resemble the cut surface of an onion. Observe the presence of an arrector pili muscle (AP) and profiles of ducts (d) of a sweat gland in the vicinity of, but not associated with, the pacinian corpuscle.
Nail plate
Nail groove
|
Nail bed |
|
Nail |
Hyponychium |
|
root |
||
|
Fingernail
KEY
AP |
arrector pili |
Hy |
hyponychium |
NW |
nail wall |
Ca |
capsule |
IC |
inner core |
OC |
outer core |
Bo |
bone |
N |
nuclei |
Ph |
distal phalanx |
D |
dermis |
NB |
nail bed |
SC |
stratum corneum |
d |
duct |
NF |
nerve fiber |
SB |
stratum basale |
Ep |
eponychium |
NG |
nail groove |
swG |
sweat glands |
FP |
fibrous periosteum |
NP |
nail plate |
|
|
HC |
hyaline cartilage |
NR |
nail root |
|
|

FIGURE 1
SB
Ca N
NF
FIGURE 3
Corpuscles Meissner’s and Pacinian Nail,• 4-11 PLATE
FIGURE 2
AP
d
IC Ca
OC
NF
FIGURE 4

Microscopy Electron Gland, weat • S5-11 PLATE
FIGURE 1
FIGURE 1. Sweat gland. x.s. Human. Electron microscopy. ×5,040.
Tight junctions (arrows) occur at three locations in the secretory coil of human sweat glands: (1) between clear cells (C) separating the lumen of the intercellular canaliculus (arrowhead) and the basolateral intercellular space, (2) between
two dark cells (D) separating the main lumen and the lateral intercellular space, and (3) between a clear cell and a dark cell, separating the main lumen (L) and intercellular space. Note the presence of secretory granules (SG) and myoepithelial cell
(ME). (From Briggman JV, Bank HL, Bigelow JB, et al. Structure of the tight junctions of the human eccrine sweat gland. Am J Anat 1981;162:357–368.)
